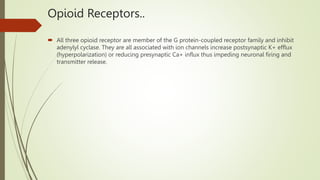
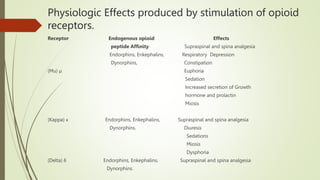
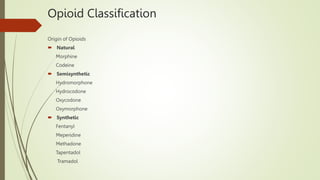
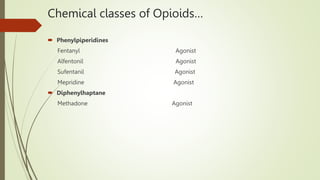
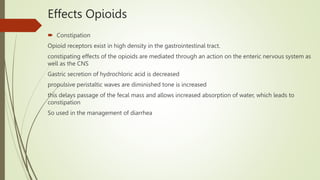
The document discusses opioids and their use in pain management. It provides an overview of opioids, describing them as natural, semisynthetic, or synthetic drugs that bind to opioid receptors in the central nervous system. It then discusses several specific opioids like morphine, codeine, oxycodone, fentanyl, and methadone, outlining their classifications, mechanisms of action, indications, and side effects. The document also covers topics like opioid receptors, partial agonists and mixed agonist-antagonists, and the physiological effects of stimulating opioid receptors.

![Hydromorphone and Hydrocodone
Hydromorphone
Hydromorphone, also known as dihydromorphinone, and sold under the brand name Dilaudid
among others, is an opioid used to treat moderate to severe pain. Hydromorphone and
Hydrocodone are orally active, semisynthetic analogs of morphine and codeine respectively oral
hydromorphone is approximately 8 to 10 times more potent than morphine. It is preferred over
morphine in patients with renal dysfunction due to less accumulation of active metabolites. It may
be used by mouth or by injection into a vein, muscle, or under the skin.[4] Effects generally begin
within half an hour and last for up to five hours.
Hydrocodone
Hydrocodone is methyl ether of hydromorphone but is a weaker analgesic than hydromorphone
with an oral analgesic efficiency comparable to that of morphine.
This agent is often combined with acetaminophen or ibuprofen to treat moderate to severe pain. It
is also used as an antitussive
Hydrocodone is metabolized in the liver via the action of CYP450 2D6 metabolism to hydrocodone
can be affected by drug-drug interaction.](https://image.slidesharecdn.com/opioids-221108131050-379e23a4/85/Opioids-pptx-17-320.jpg)
![Opioid Withdrawal
Users of hydromorphone may experience painful symptoms if the drug is suspended.[23] Some
people cannot tolerate the symptoms, which results in continuous drug use.[23] Symptoms of
opioid withdrawal are not easy to decipher, as there are differences between drug-seeking
behaviors and true withdrawal effects. Symptoms associated with hydromorphone withdrawal
include:
Abdominal pain
Anxiety or panic attacks
Depression
Goose bump skin
Inability to enjoy daily activities
Muscle and joint pain
Nausea
Runny nose and excessive secretion of tears
Sweating
Vomiting](https://image.slidesharecdn.com/opioids-221108131050-379e23a4/85/Opioids-pptx-36-320.jpg)