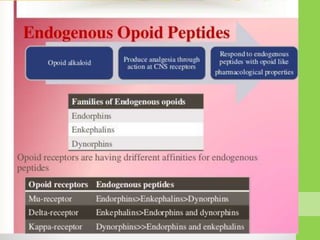
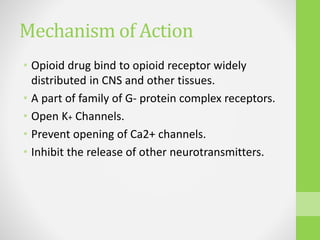
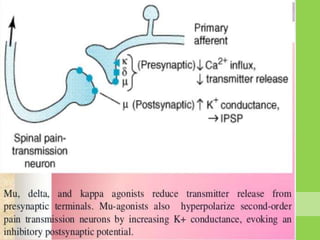
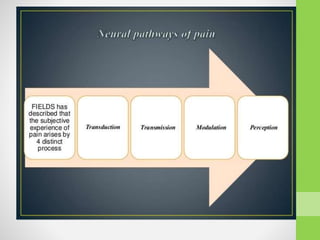
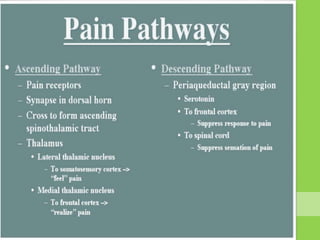
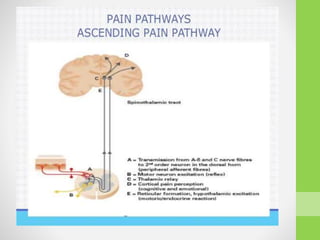
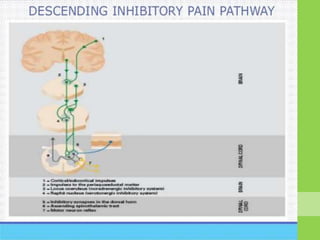
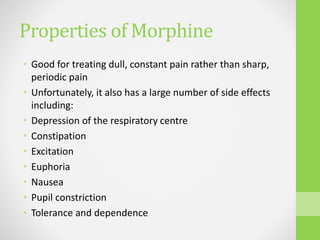
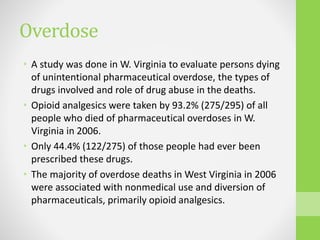
This document summarizes opioids and their use as analgesics. It discusses the classification of opioids as natural, semi-synthetic, or synthetic and describes their mechanisms of action through mu, delta, and kappa receptors in the central nervous system. The document outlines the pharmacokinetics of opioid absorption, distribution, metabolism, and excretion. It also discusses the clinical uses of opioids like morphine, as well as their side effects, risks of overdose and addiction, and treatment options for opioid overuse.