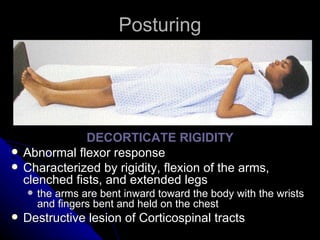
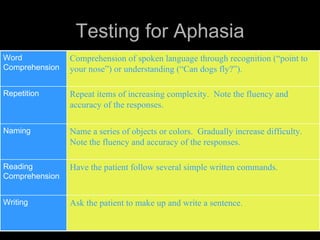
This document provides an overview of performing a neurological examination, including objectives, components, and techniques. It discusses evaluating various areas such as mental status, cranial nerves, motor function, reflexes, and sensory status. It also covers localizing neurological lesions, differentiating central and peripheral nervous system disorders, and assessing various conditions including movement disorders, levels of consciousness, and aphasia.