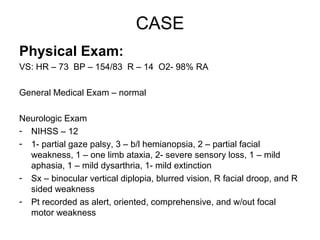
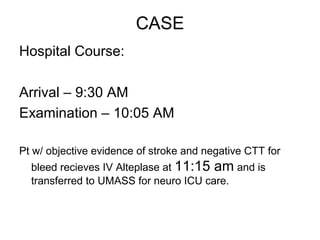
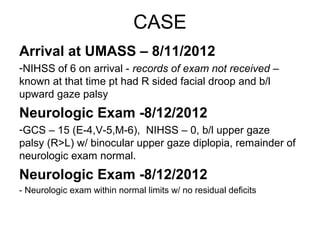
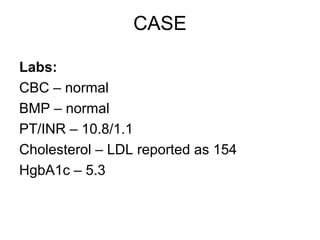
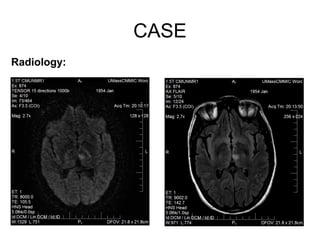
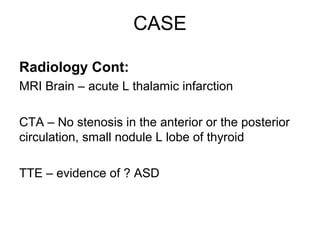
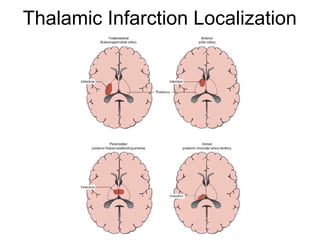
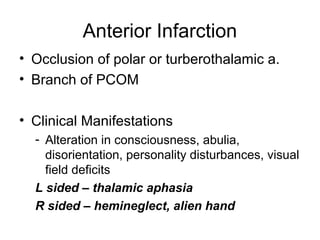
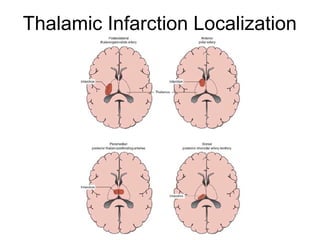
A 58-year-old female presented with sudden onset blurred vision and right-sided weakness and was found to have an acute left thalamic infarction; imaging showed no vascular abnormalities but she had an incidental finding of a possible atrial septal defect; she was treated with tPA and made a full recovery with no residual deficits.