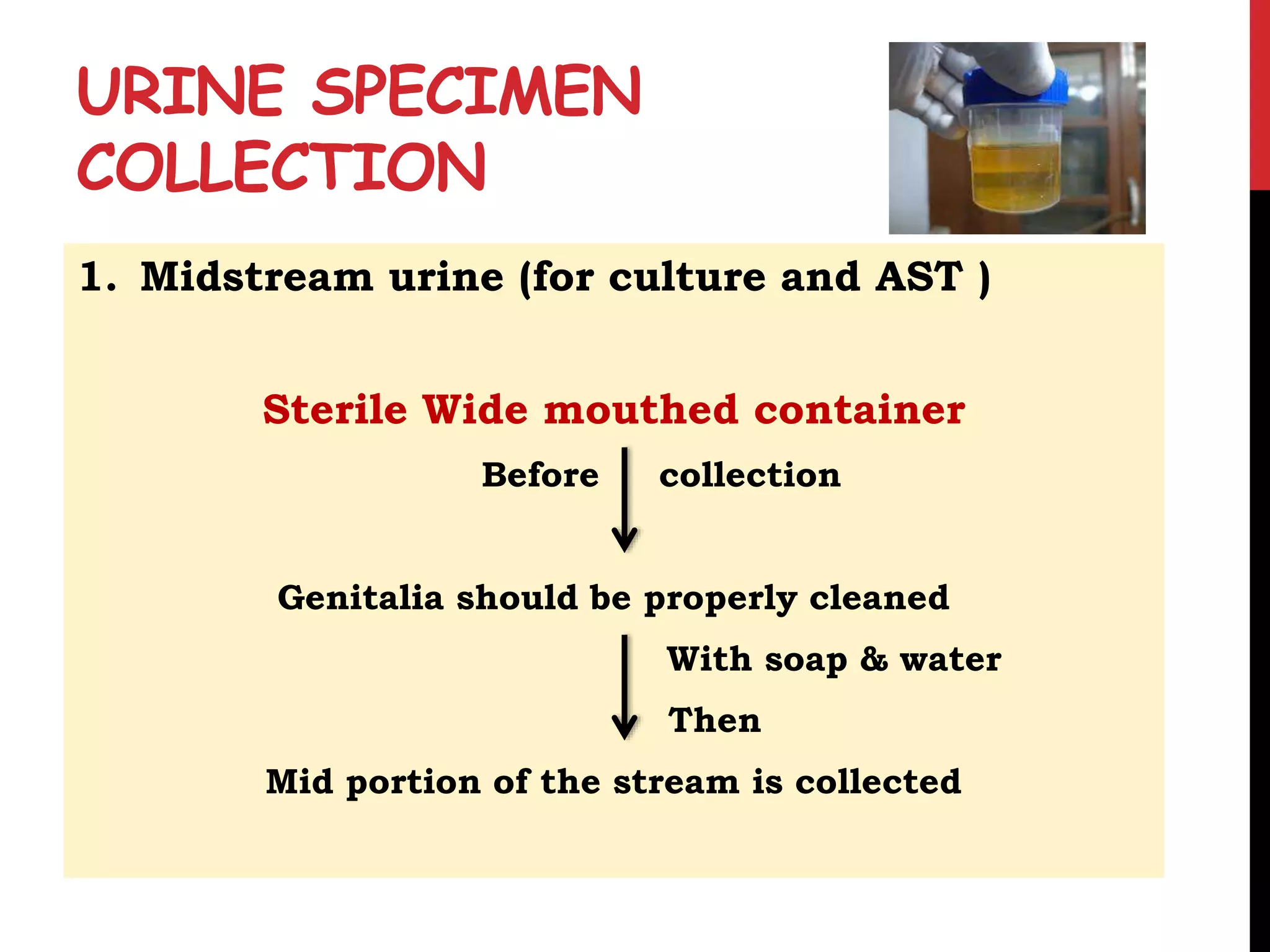
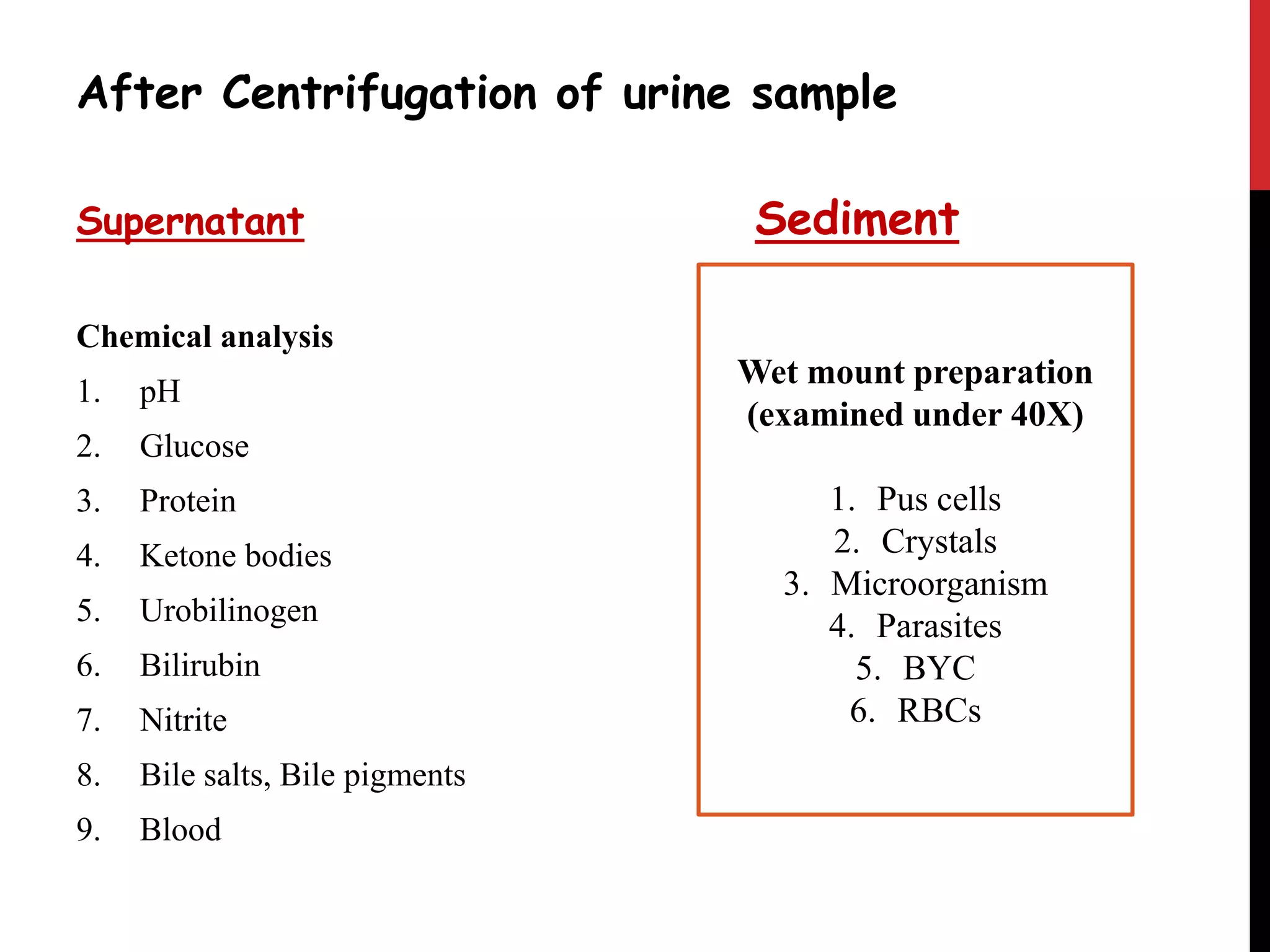
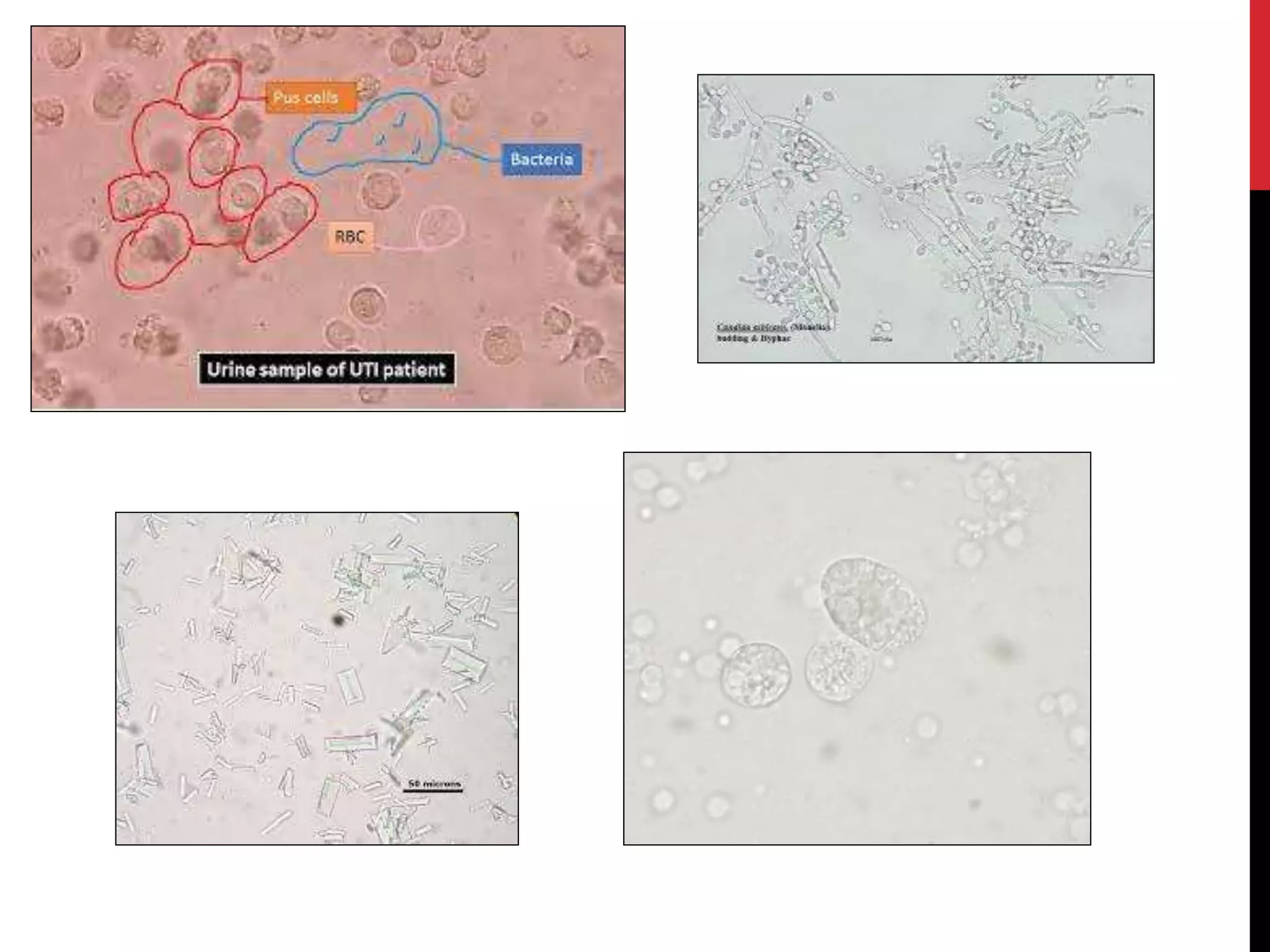
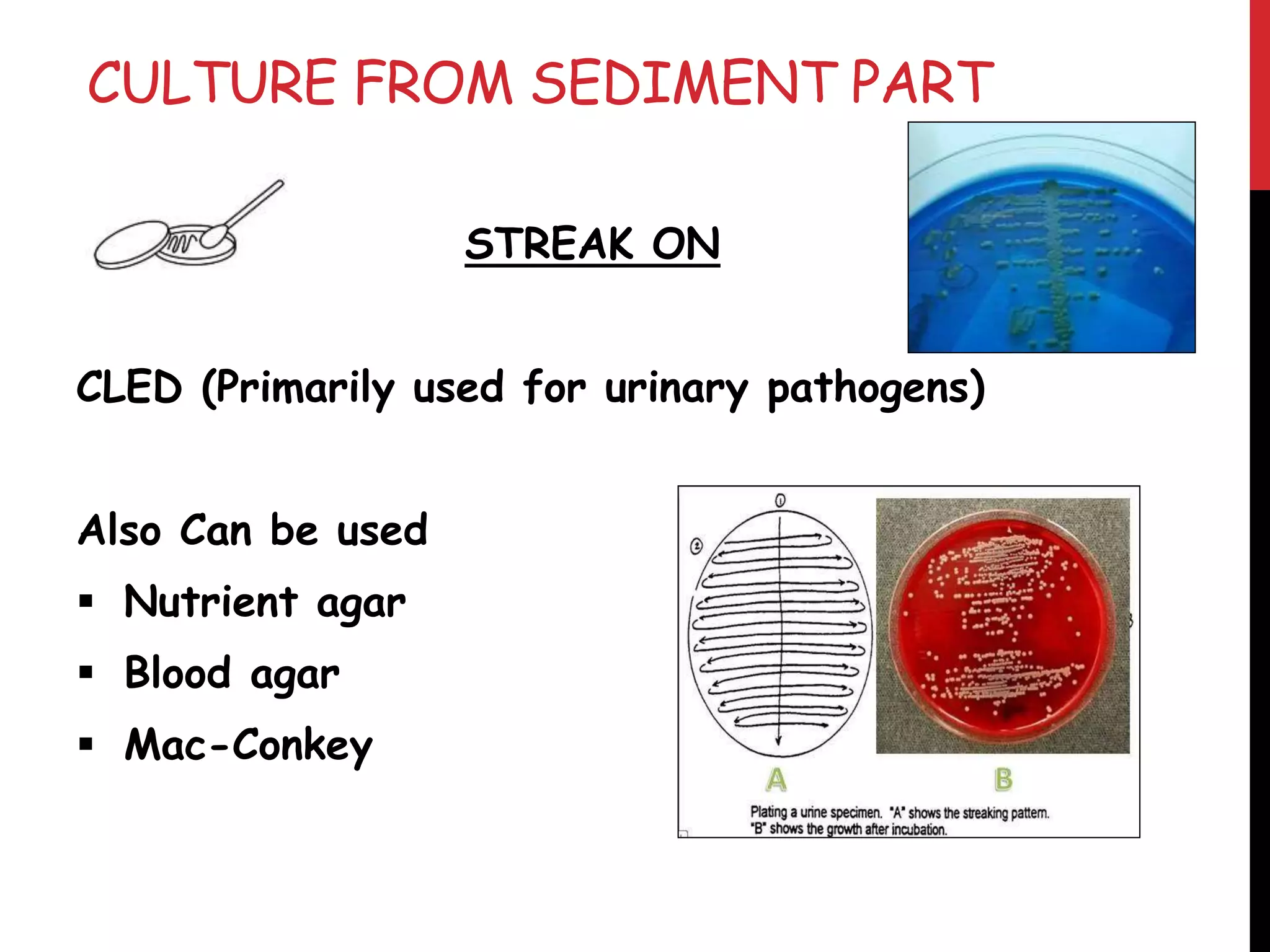
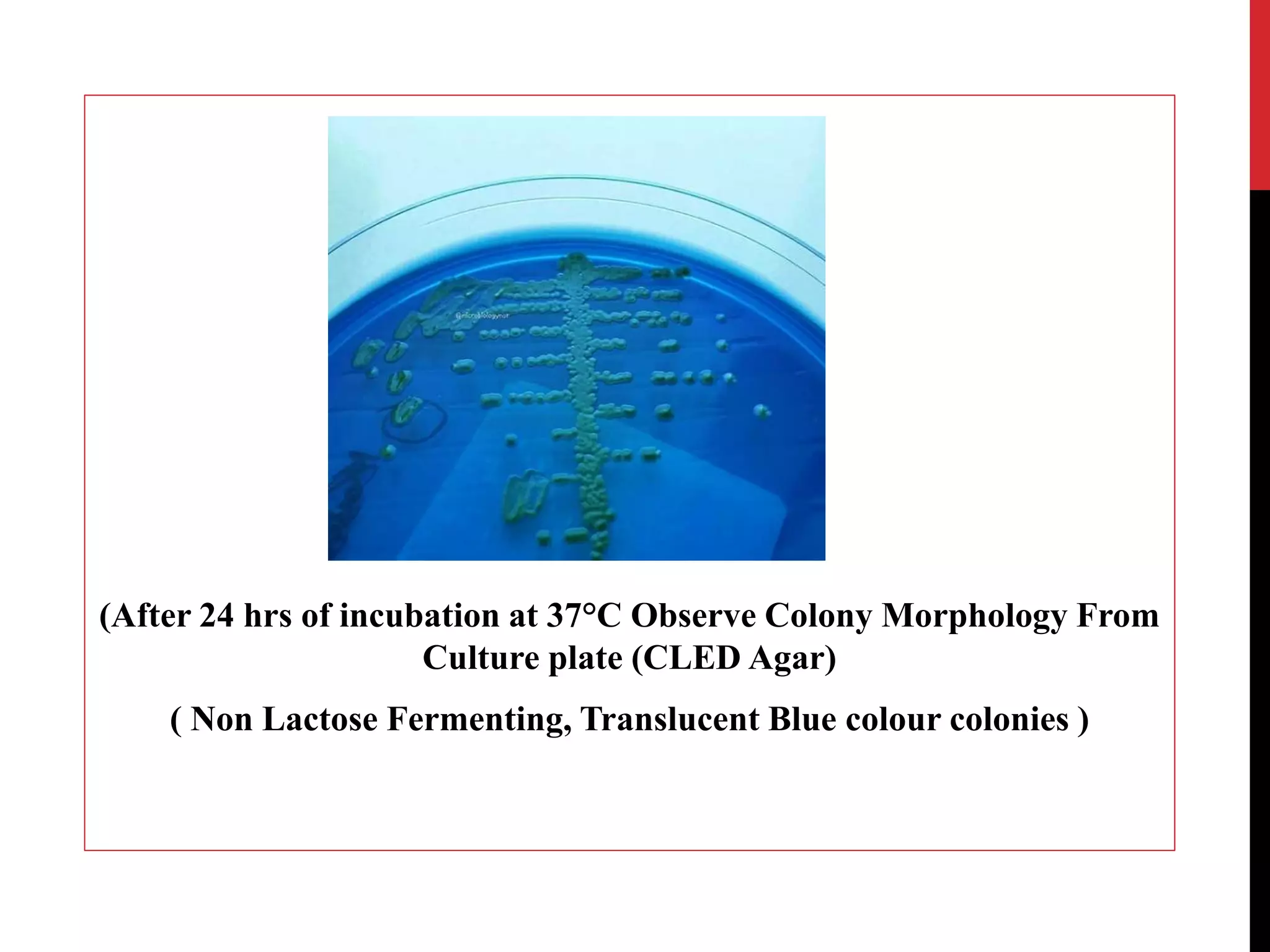
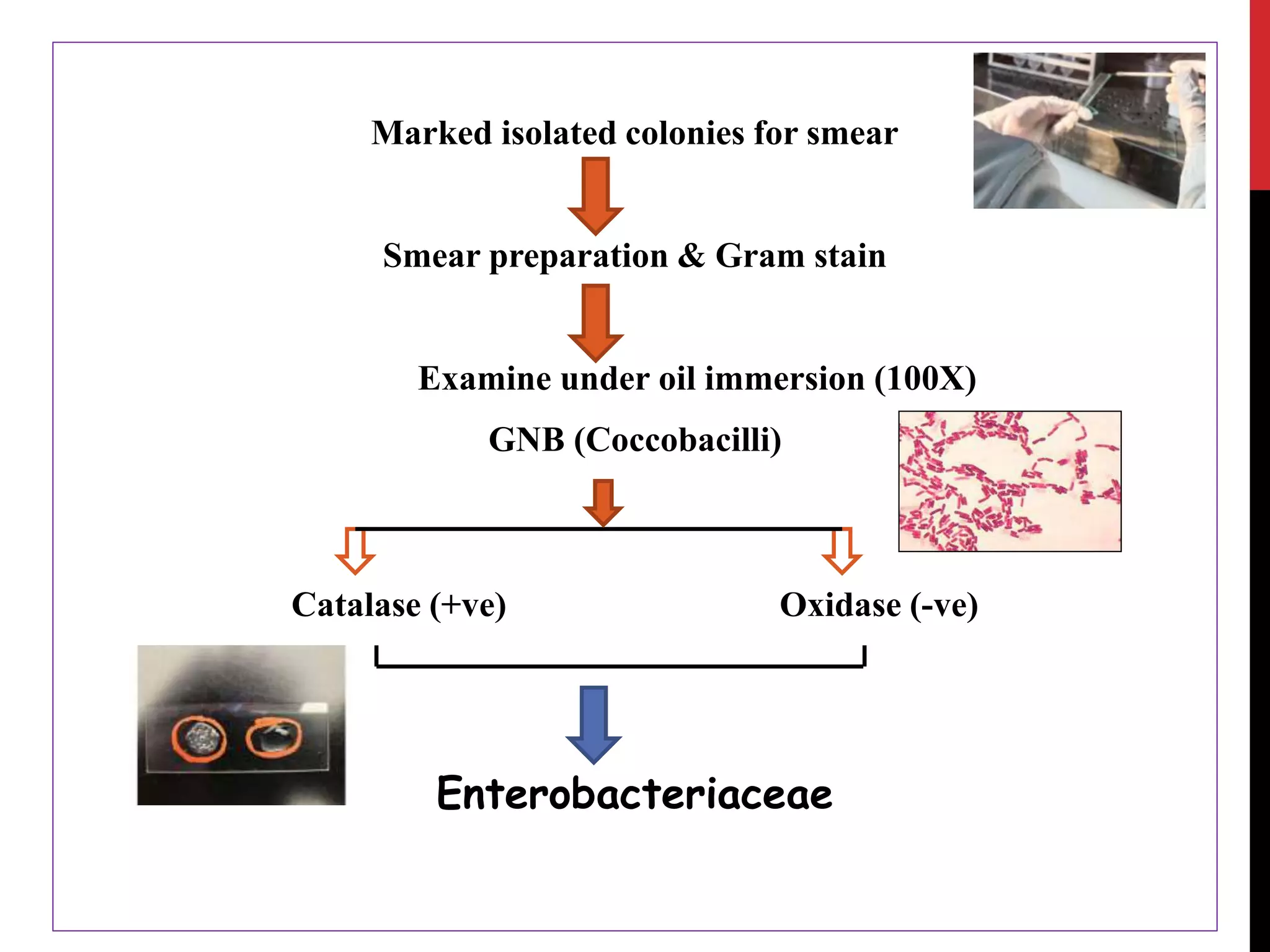
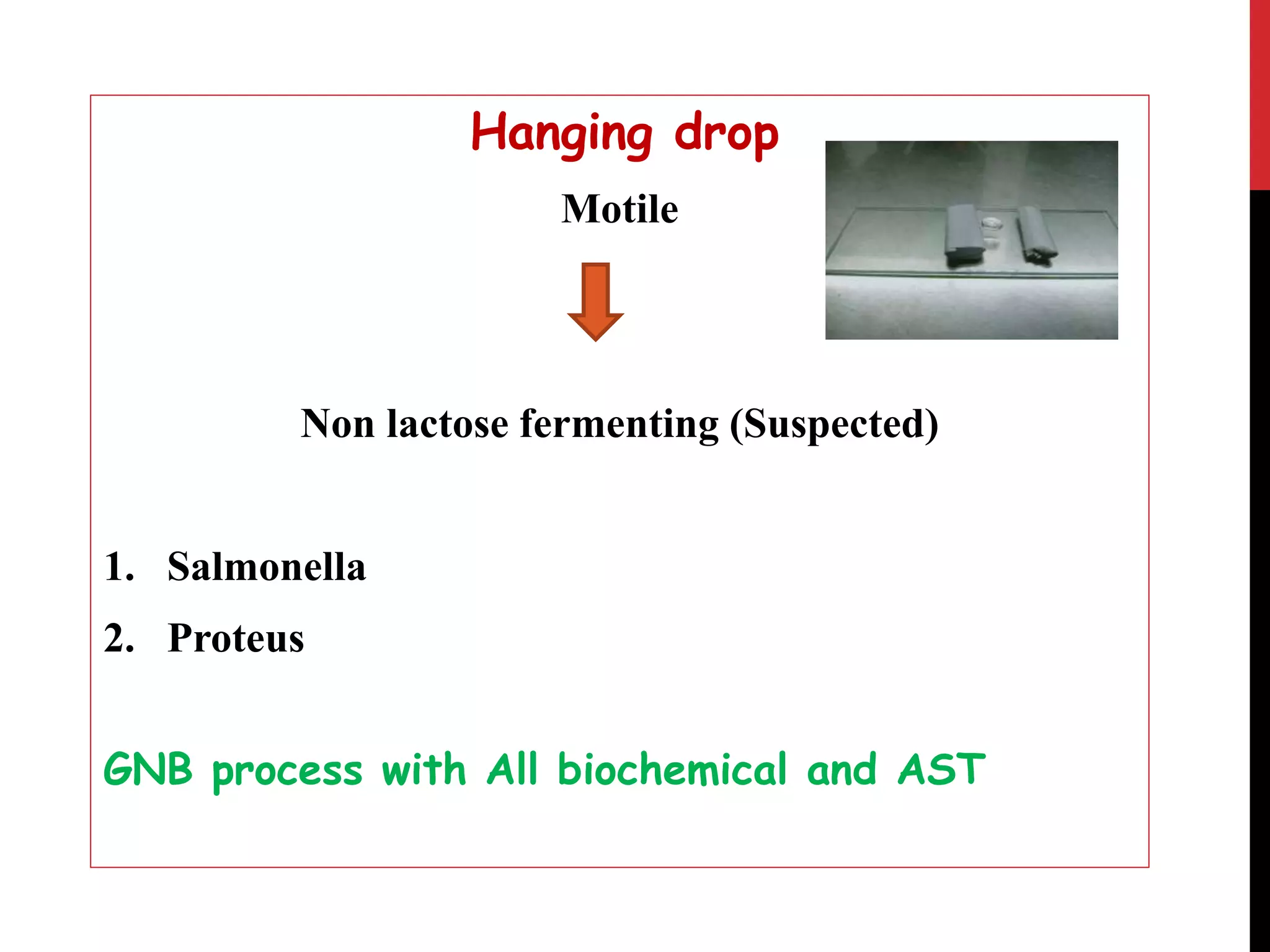
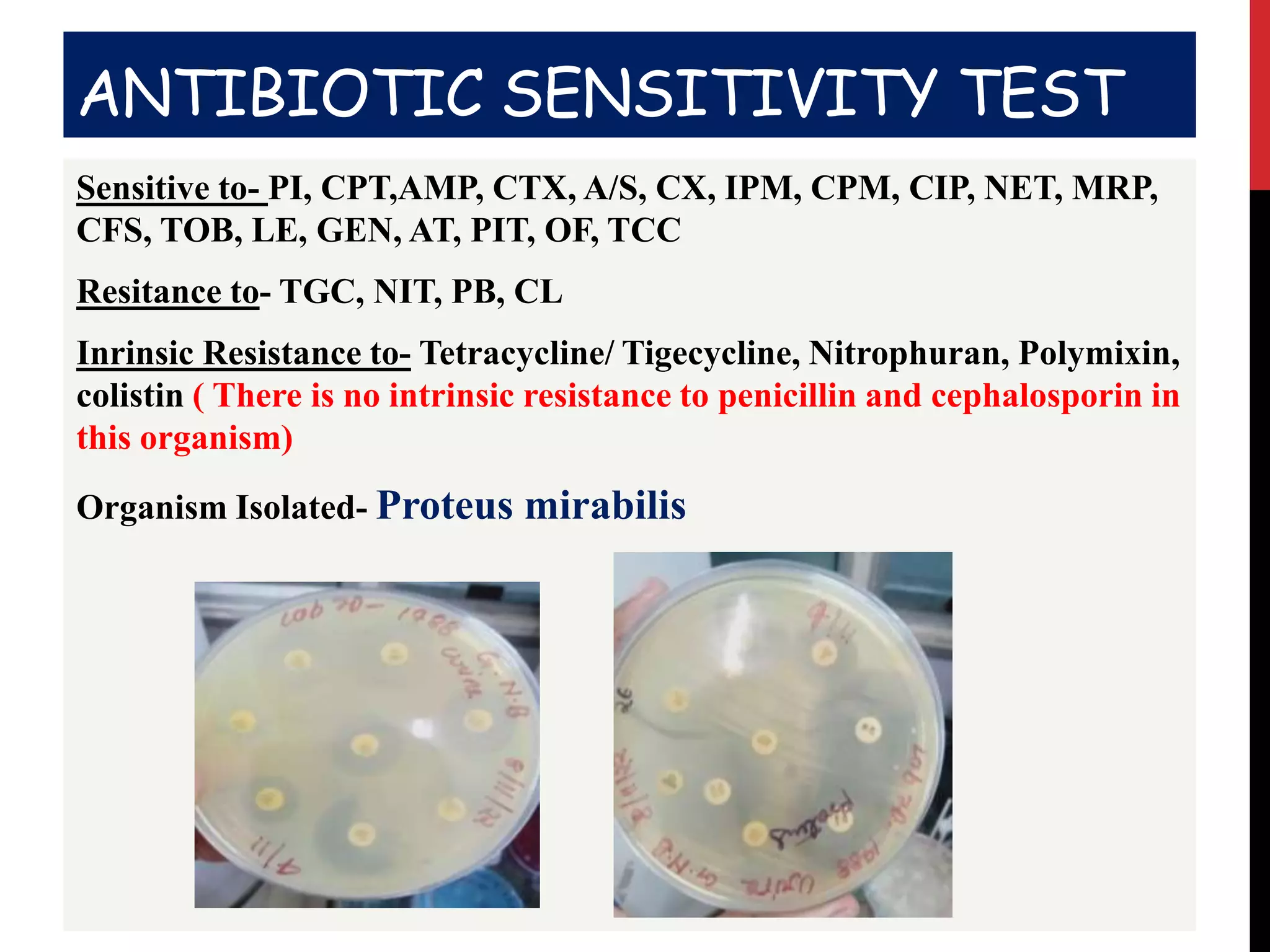
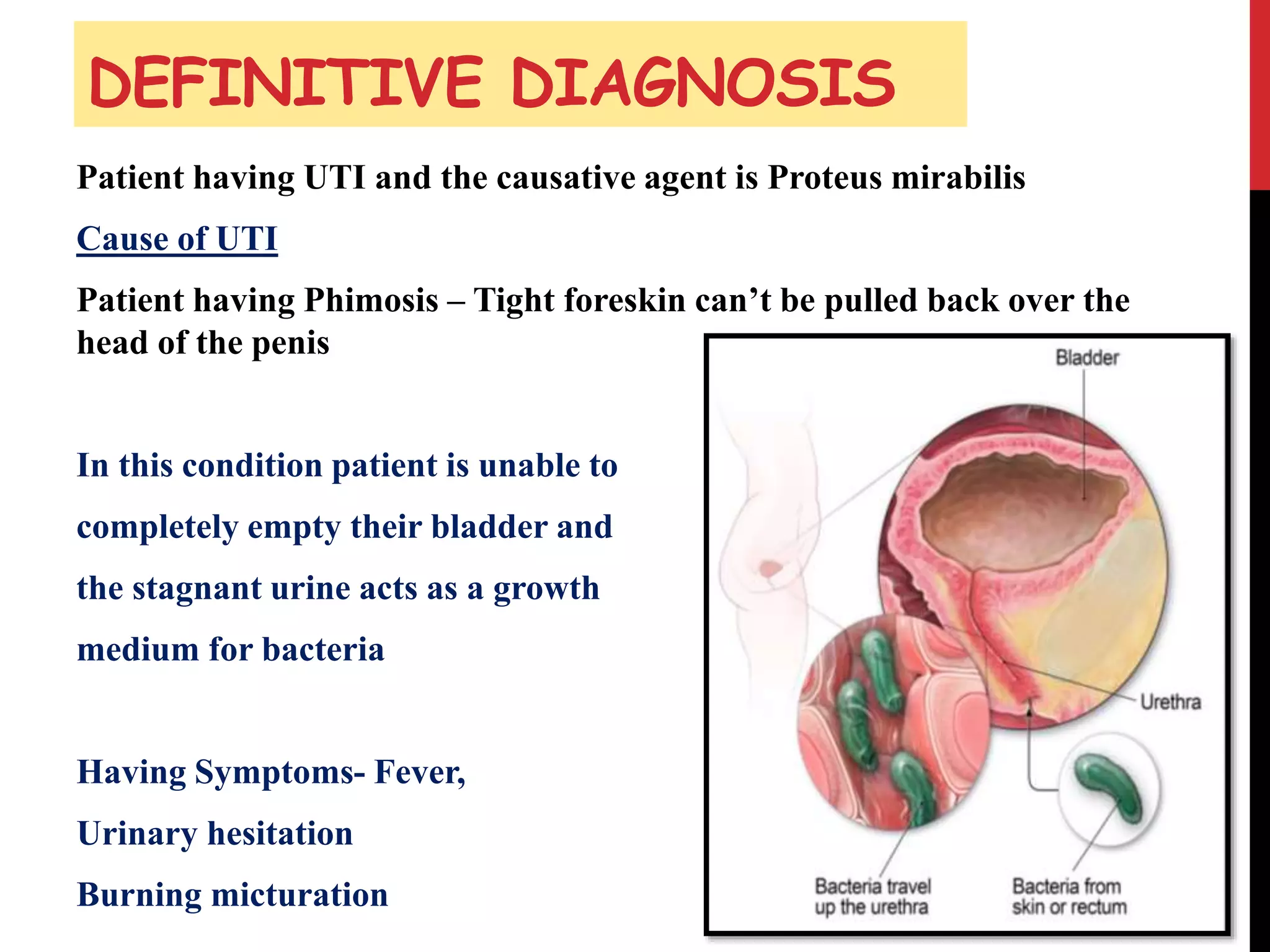
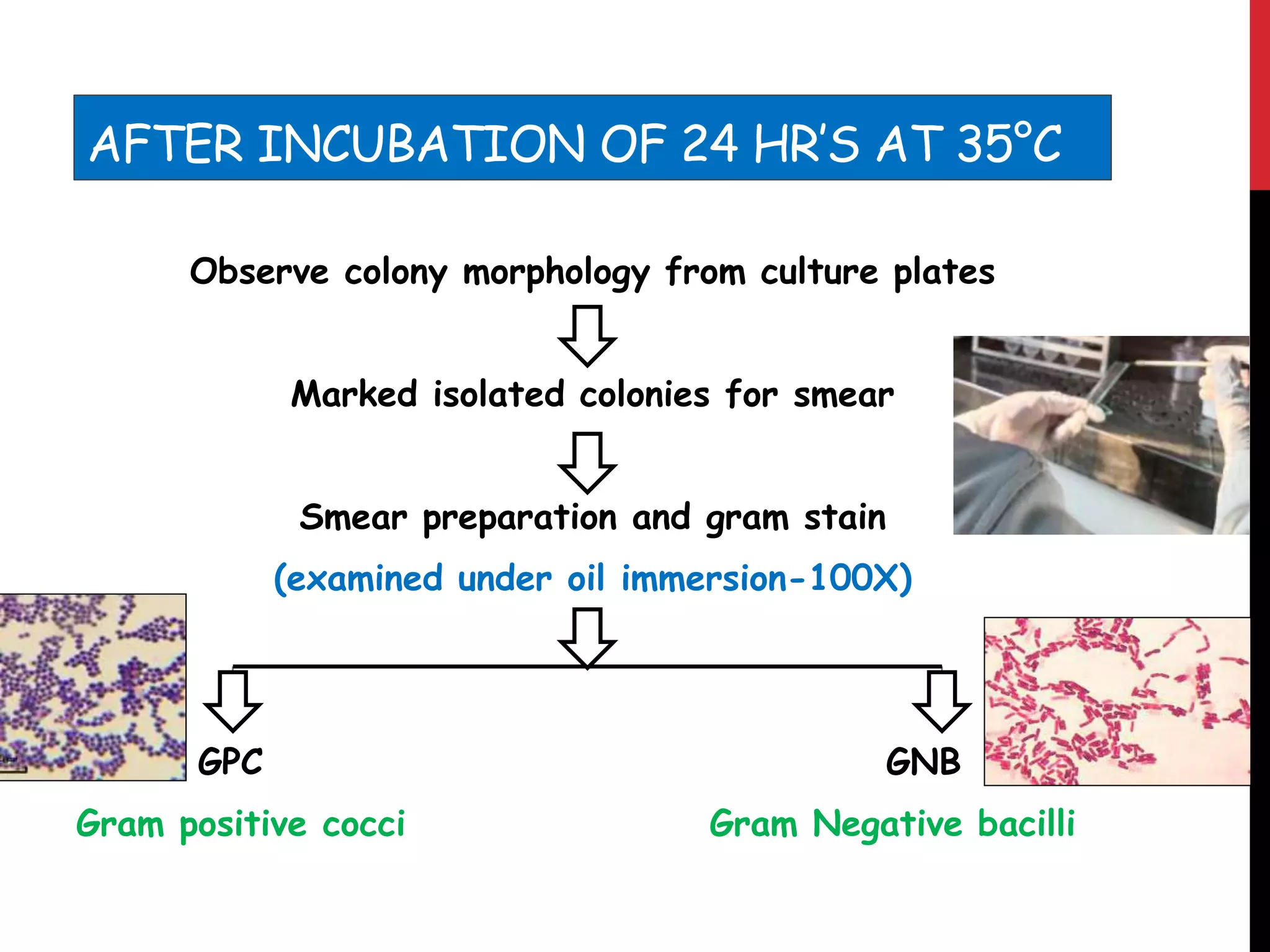
The case study presents an 11-year-old patient diagnosed with a urinary tract infection (UTI) caused by Proteus mirabilis, linked to phimosis. The microbiological evaluation included urine culture, biochemical testing, and antibiotic sensitivity assessment. The findings revealed significant bacteriuria and offered insights into treatment options and the organism's pathogenic characteristics.