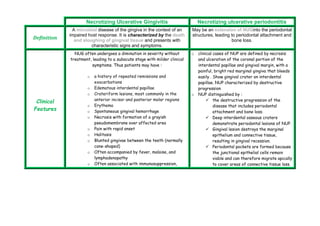
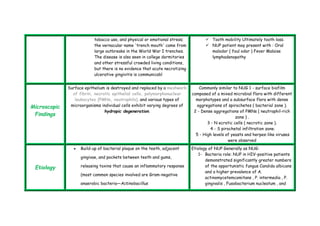
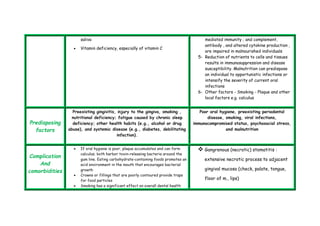
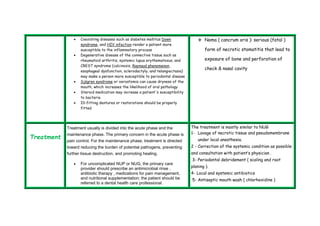
Necrotizing ulcerative gingivitis (NUG) and necrotizing ulcerative periodontitis (NUP) are microbial diseases characterized by the death of gingival tissue and can lead to significant periodontal destruction and tooth loss, particularly in immunocompromised individuals. Clinical features include painful ulcerations, malodor, and systemic symptoms such as fever and lymphadenopathy, while contributing factors include poor oral hygiene, smoking, malnutrition, and psychological stress. Treatment focuses on pain management, antimicrobial therapy, and addressing underlying conditions to prevent further tissue damage and promote healing.