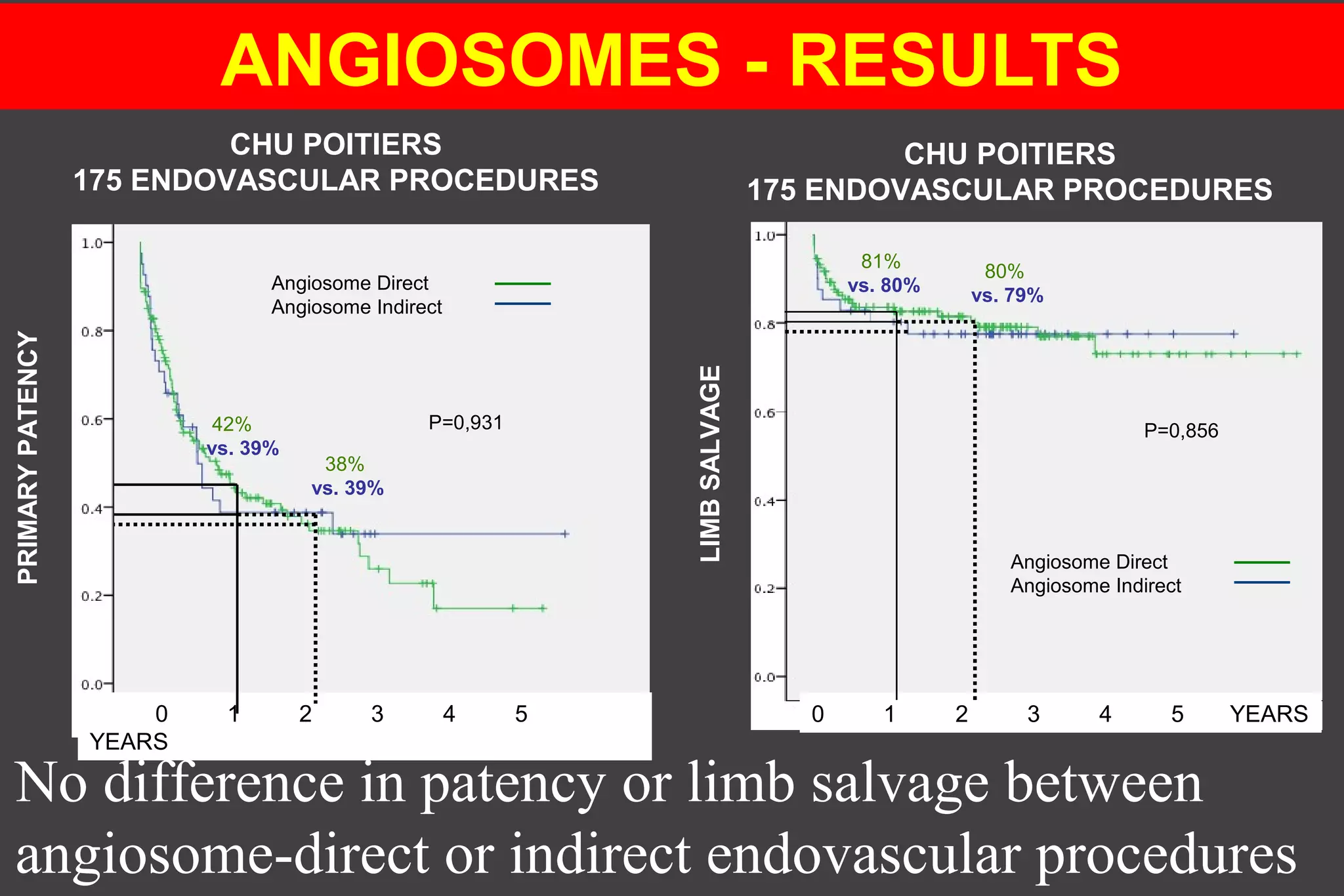
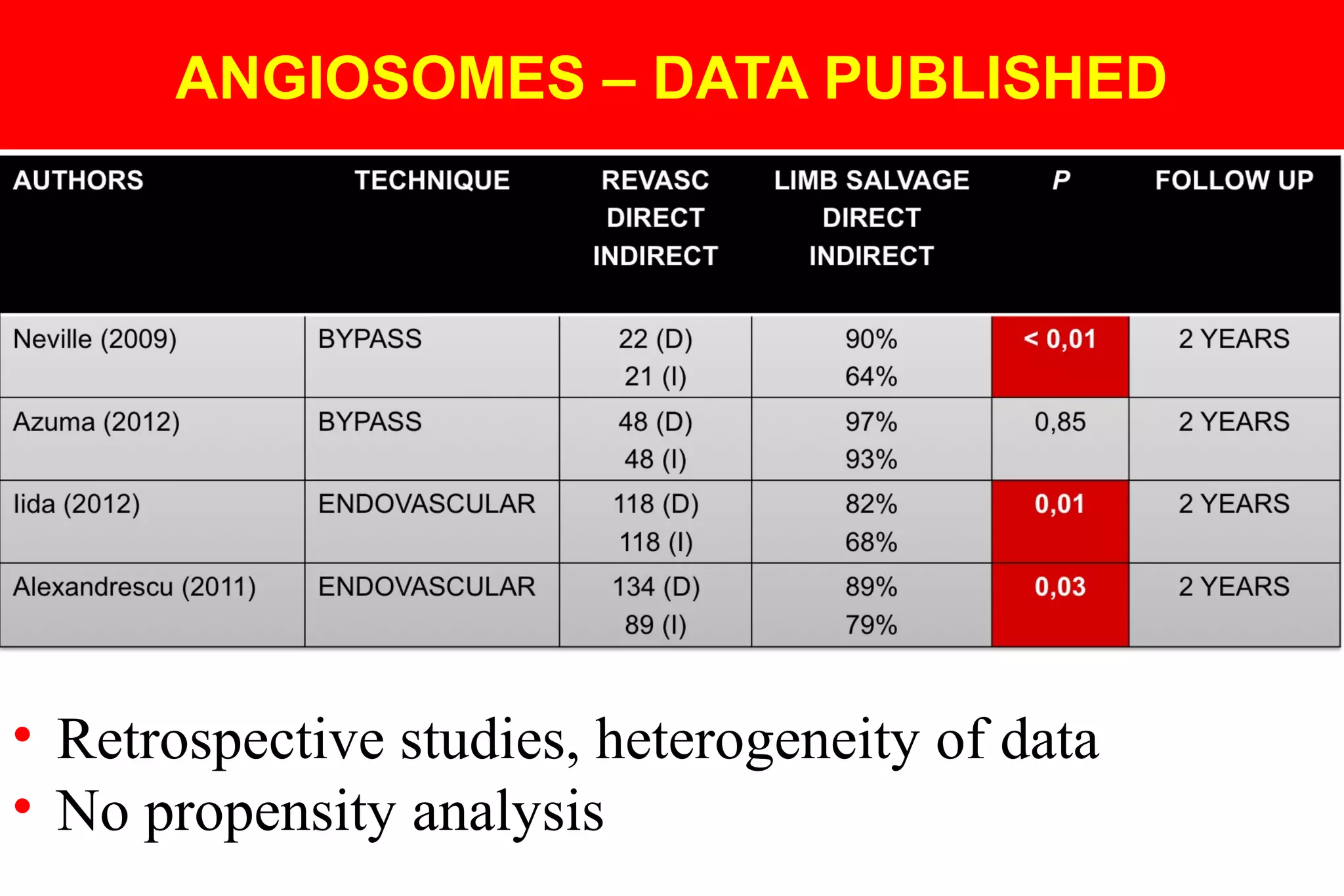
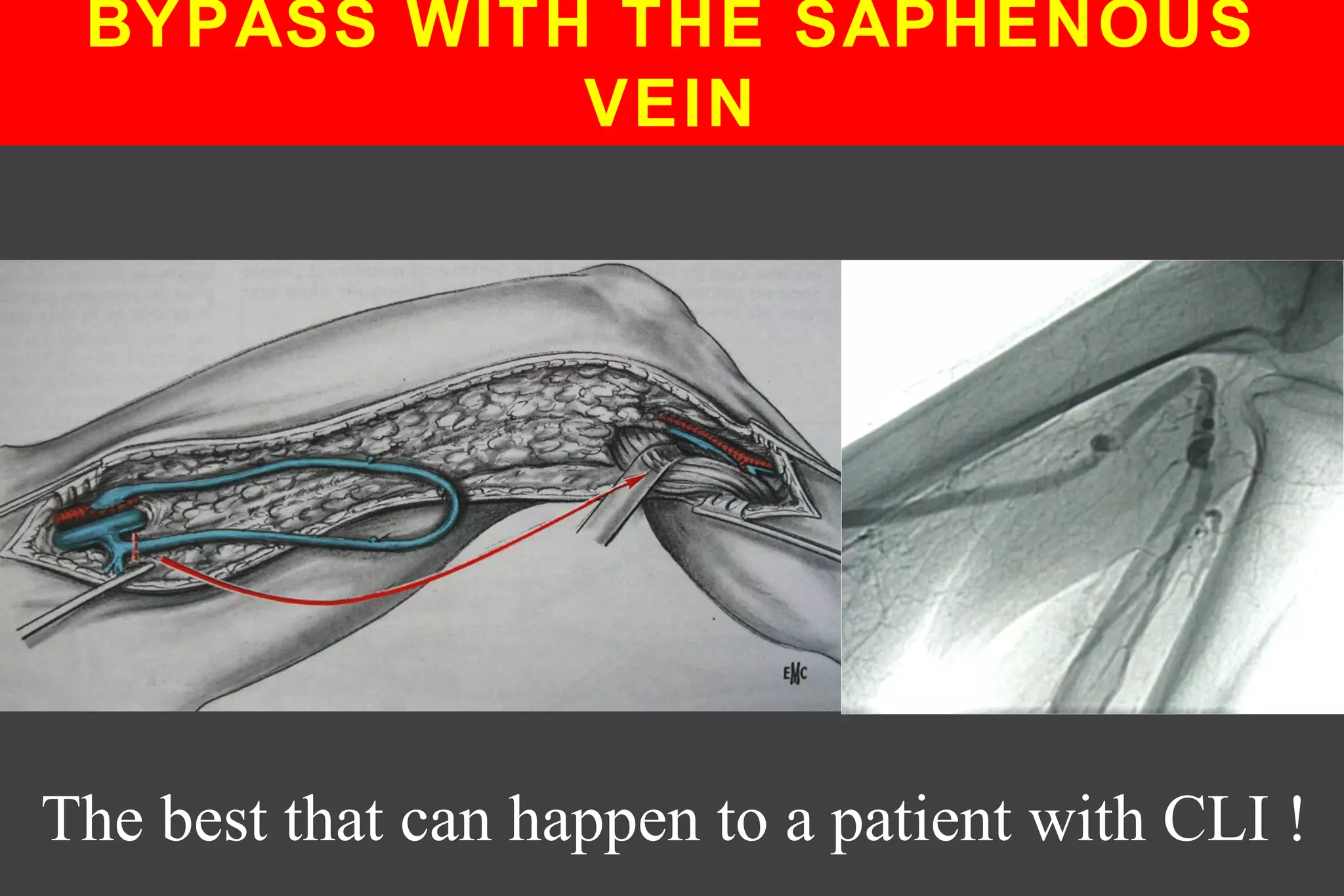
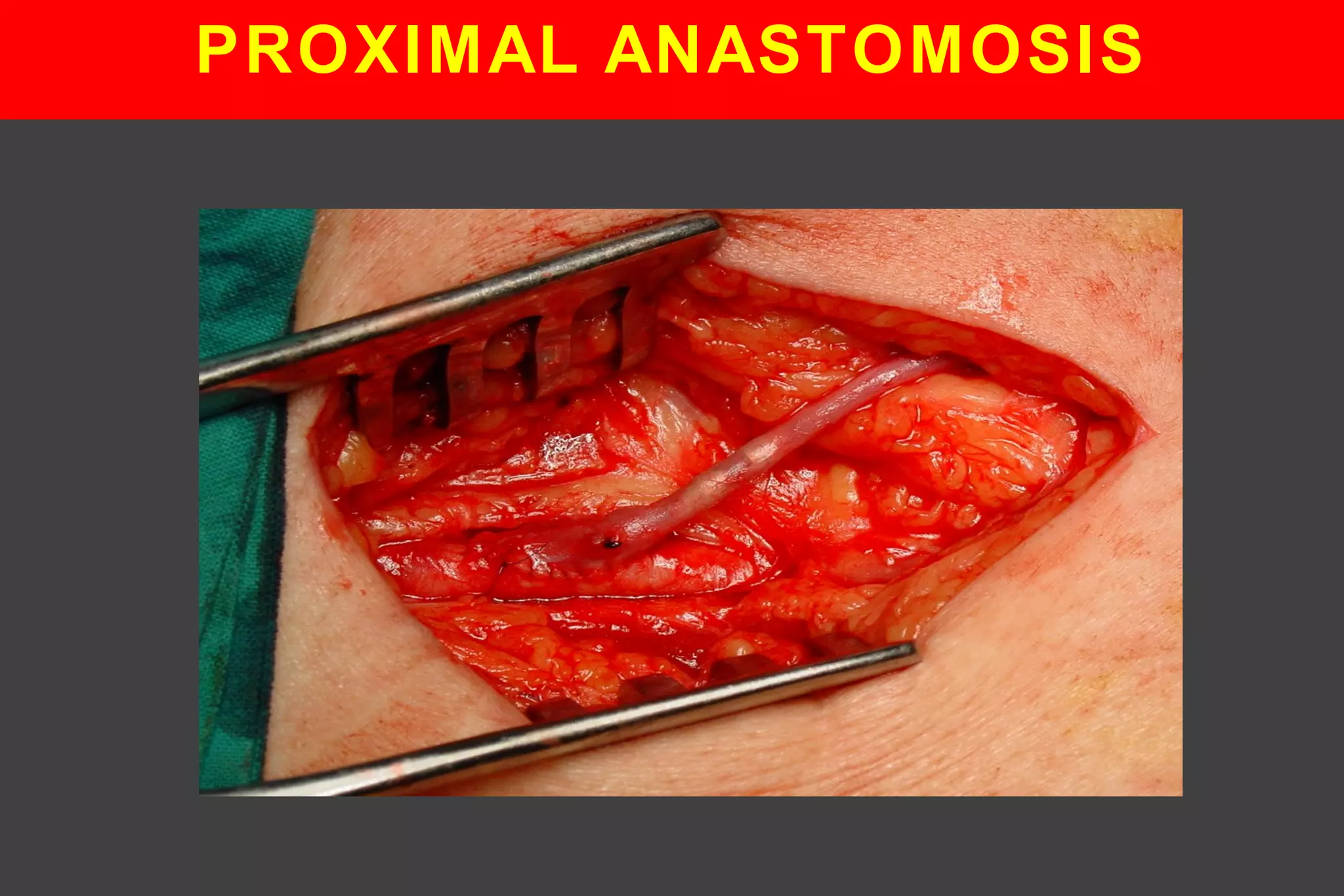
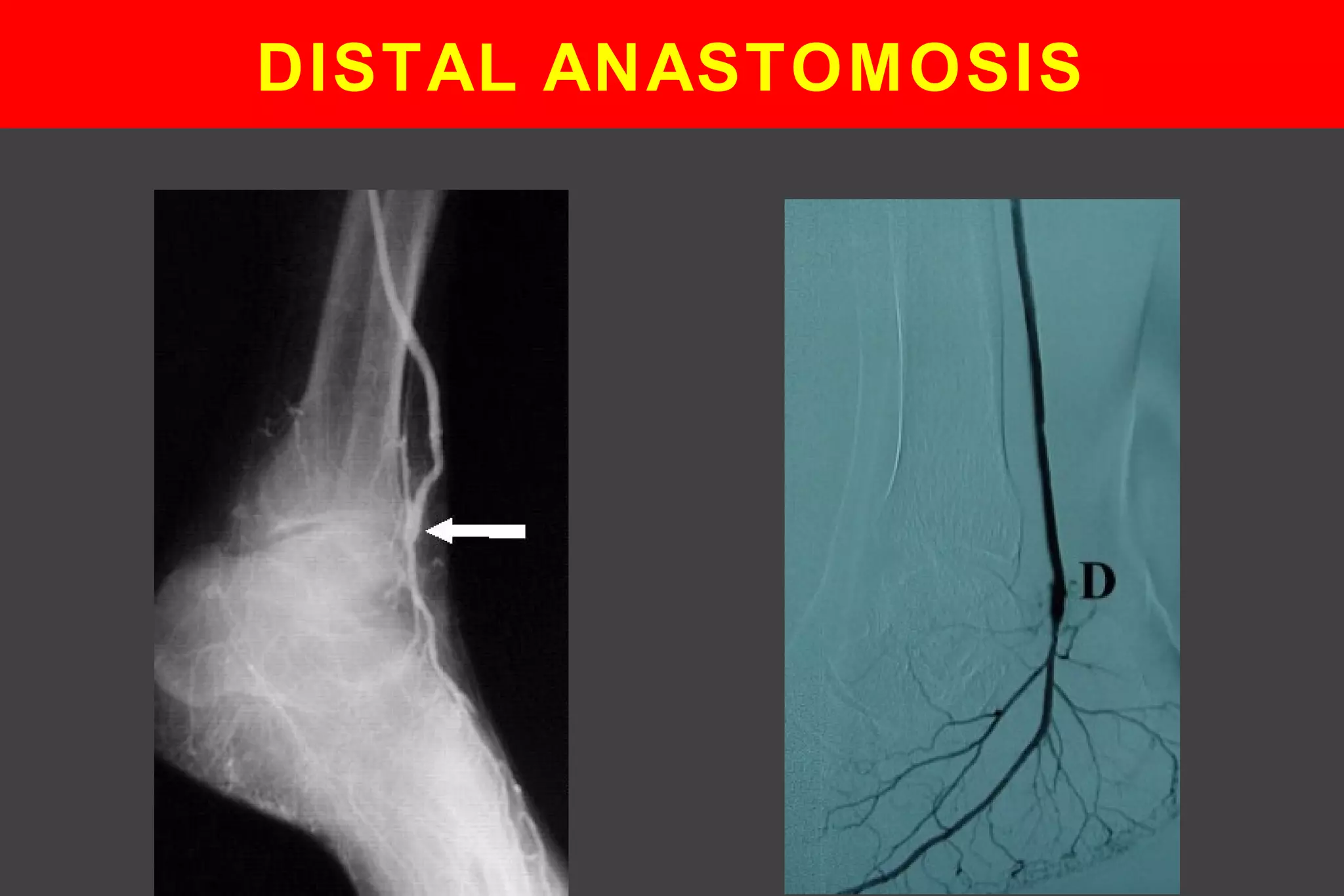
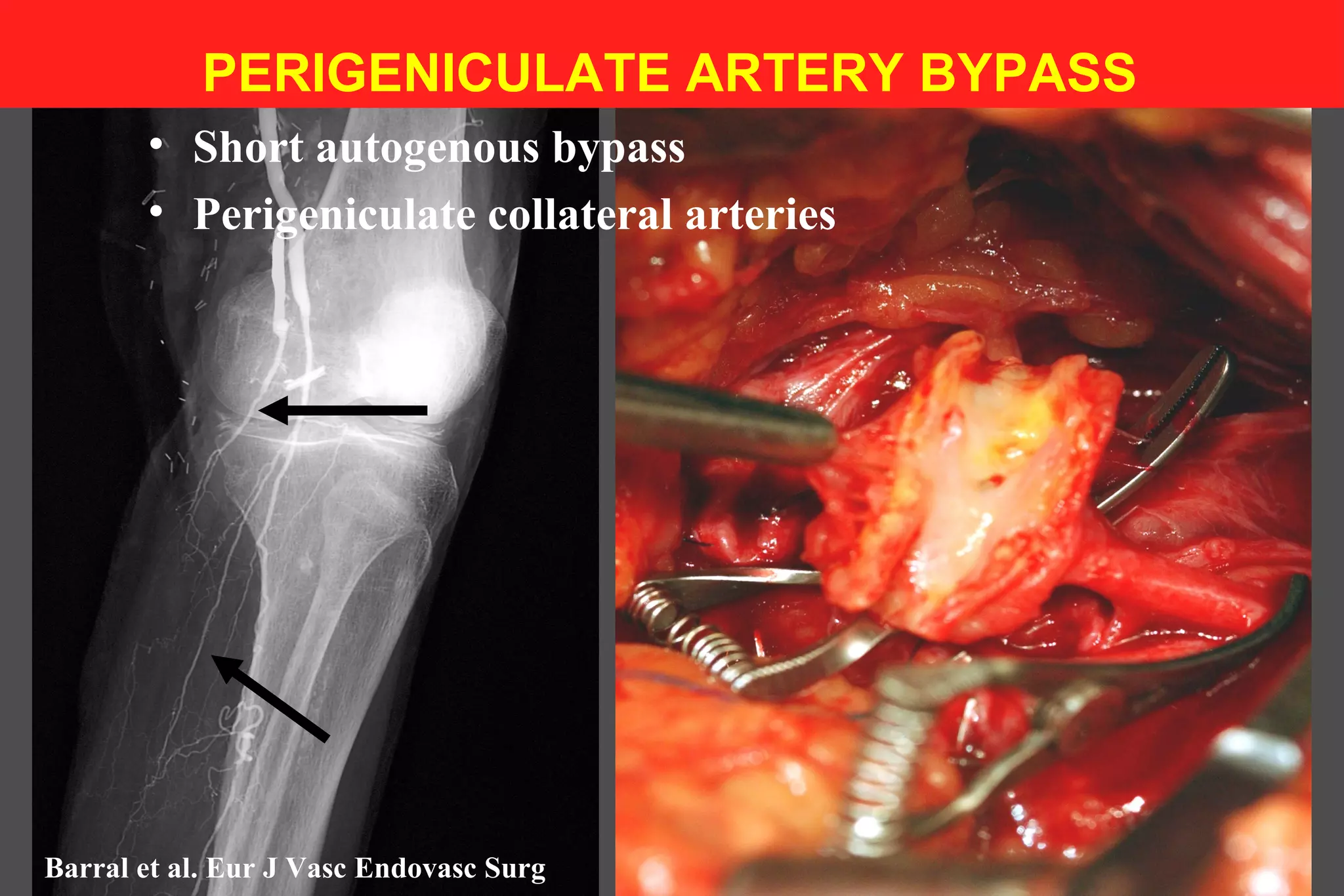
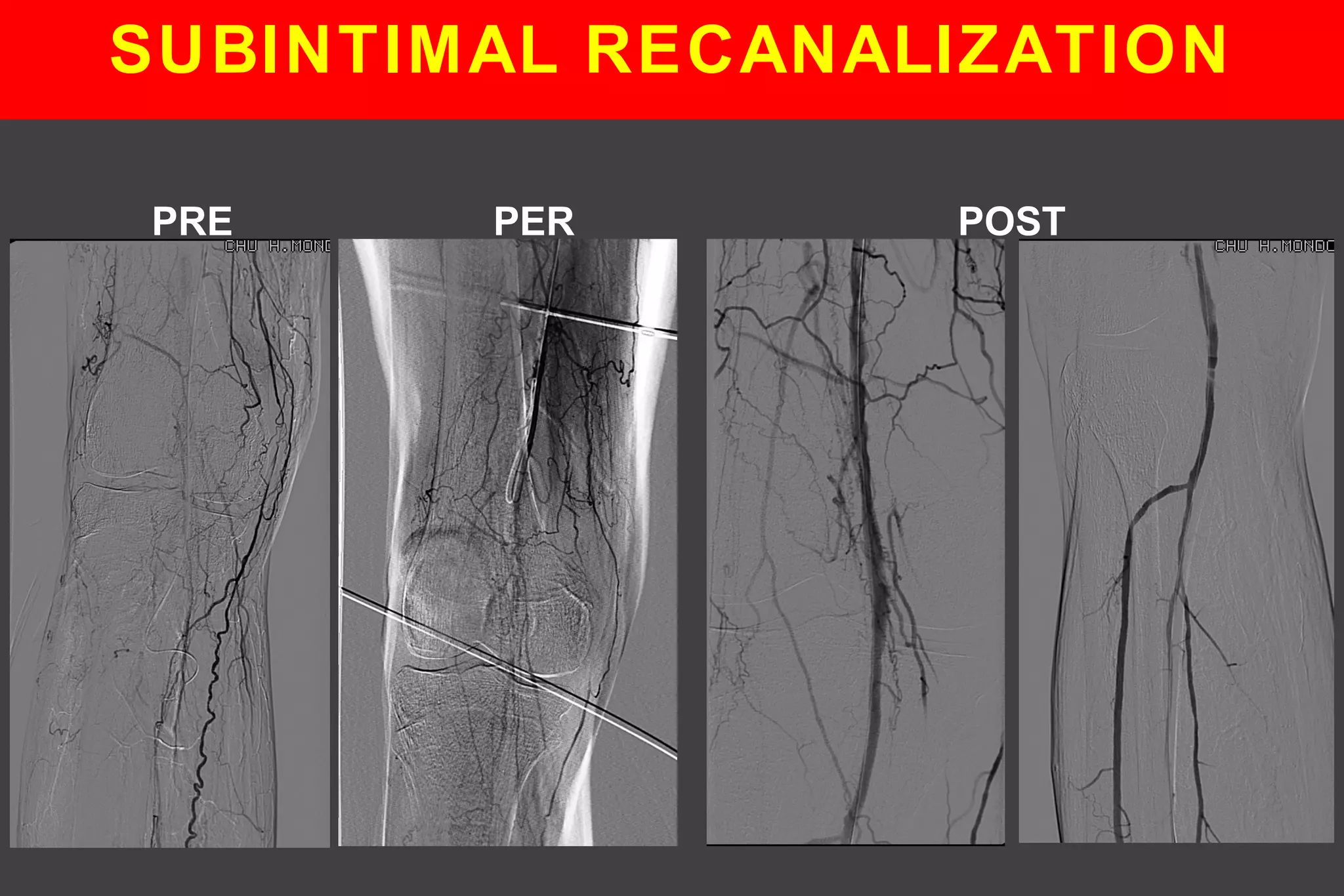
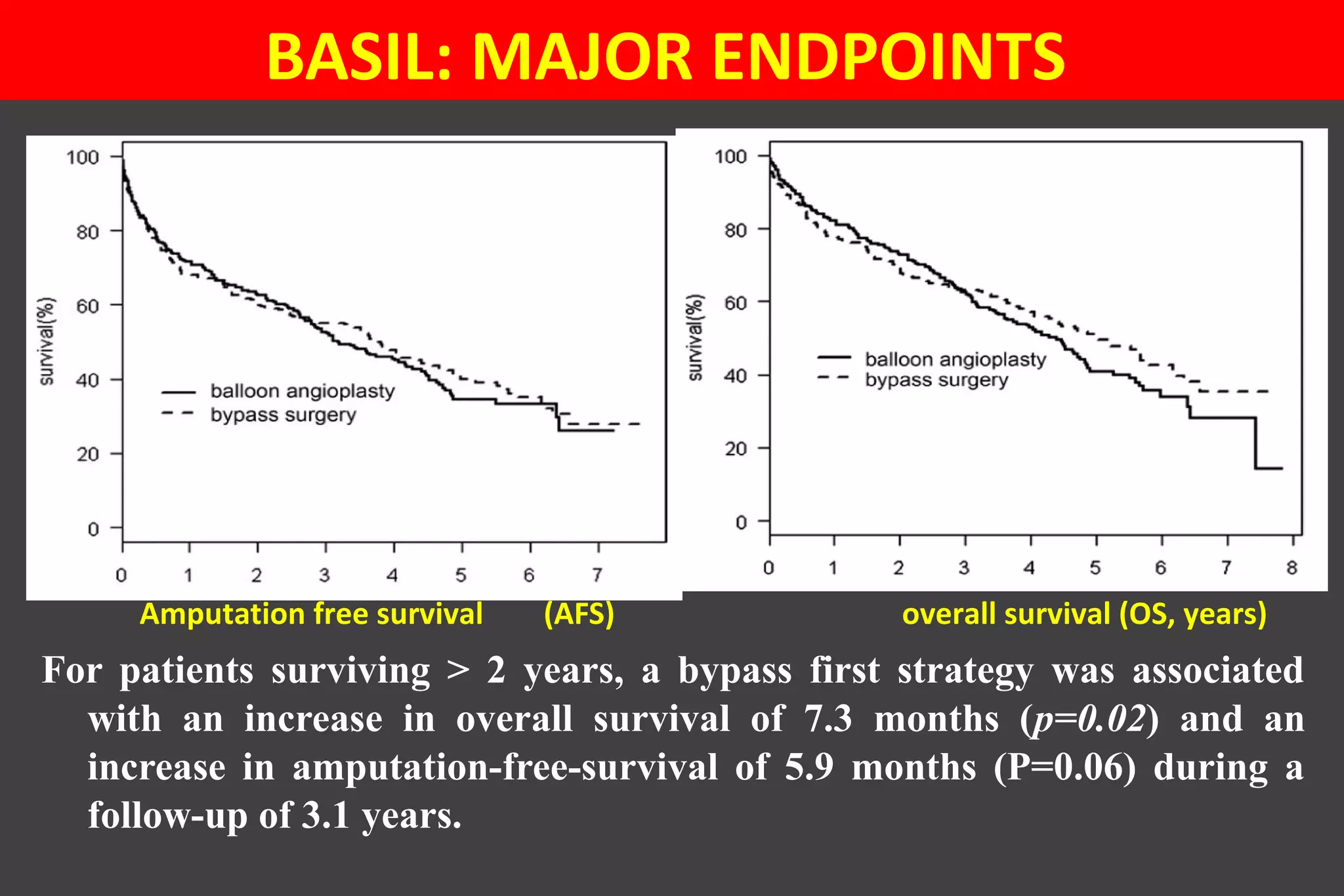
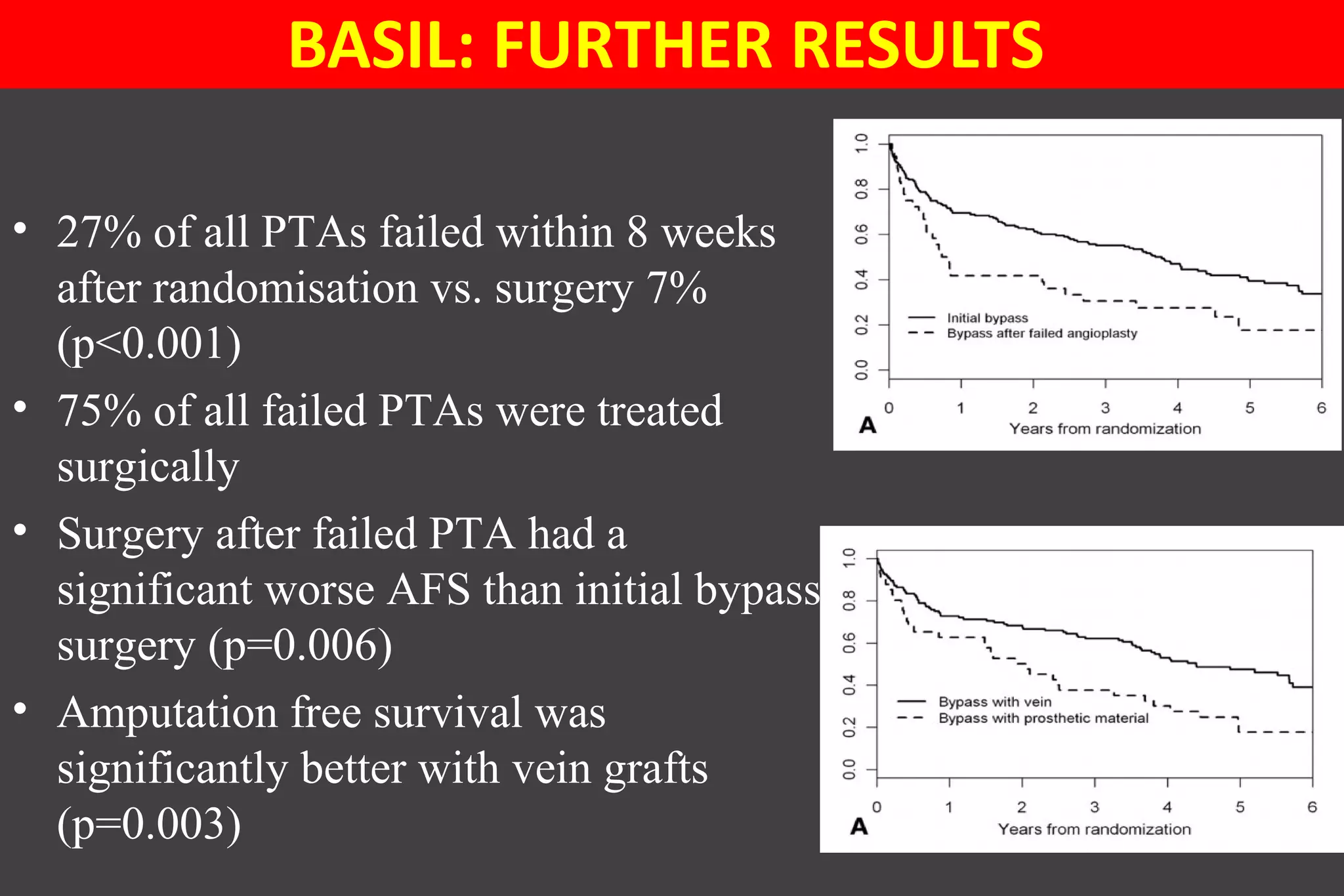
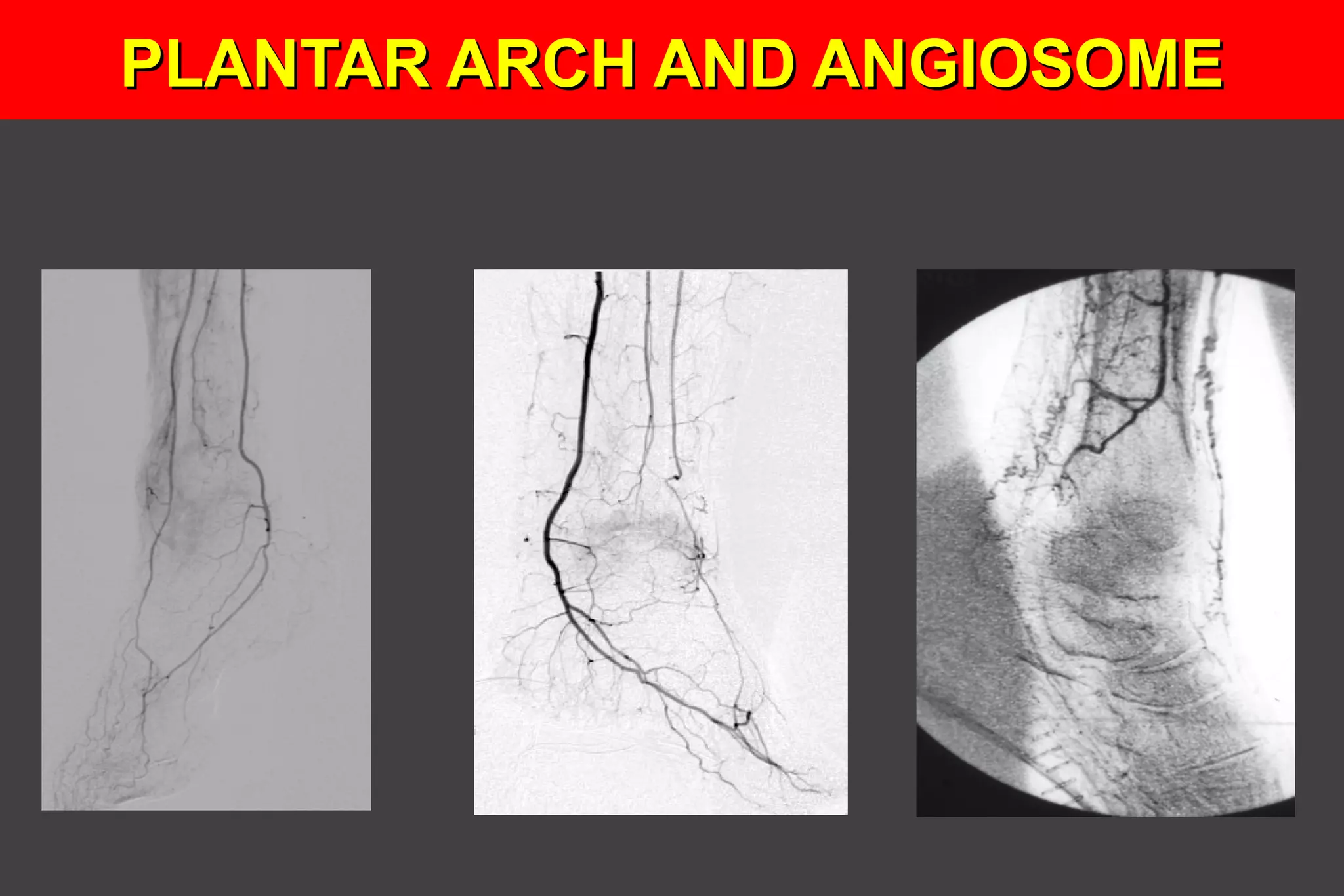
This document summarizes key points from a presentation on treating chronic critical limb ischemia. It discusses the benefits of revascularization over amputation for patient survival. Bypass surgery using the saphenous vein has better outcomes than prosthetic grafts, especially below the knee. Endovascular techniques have improved but primary patency remains lower than bypass. The BASIL trial found initial bypass surgery led to better amputation-free survival compared to initial angioplasty. The concept of angiosomes provides a framework for endovascular revascularization but published data on outcomes based on direct versus indirect angiosome targeting is limited.

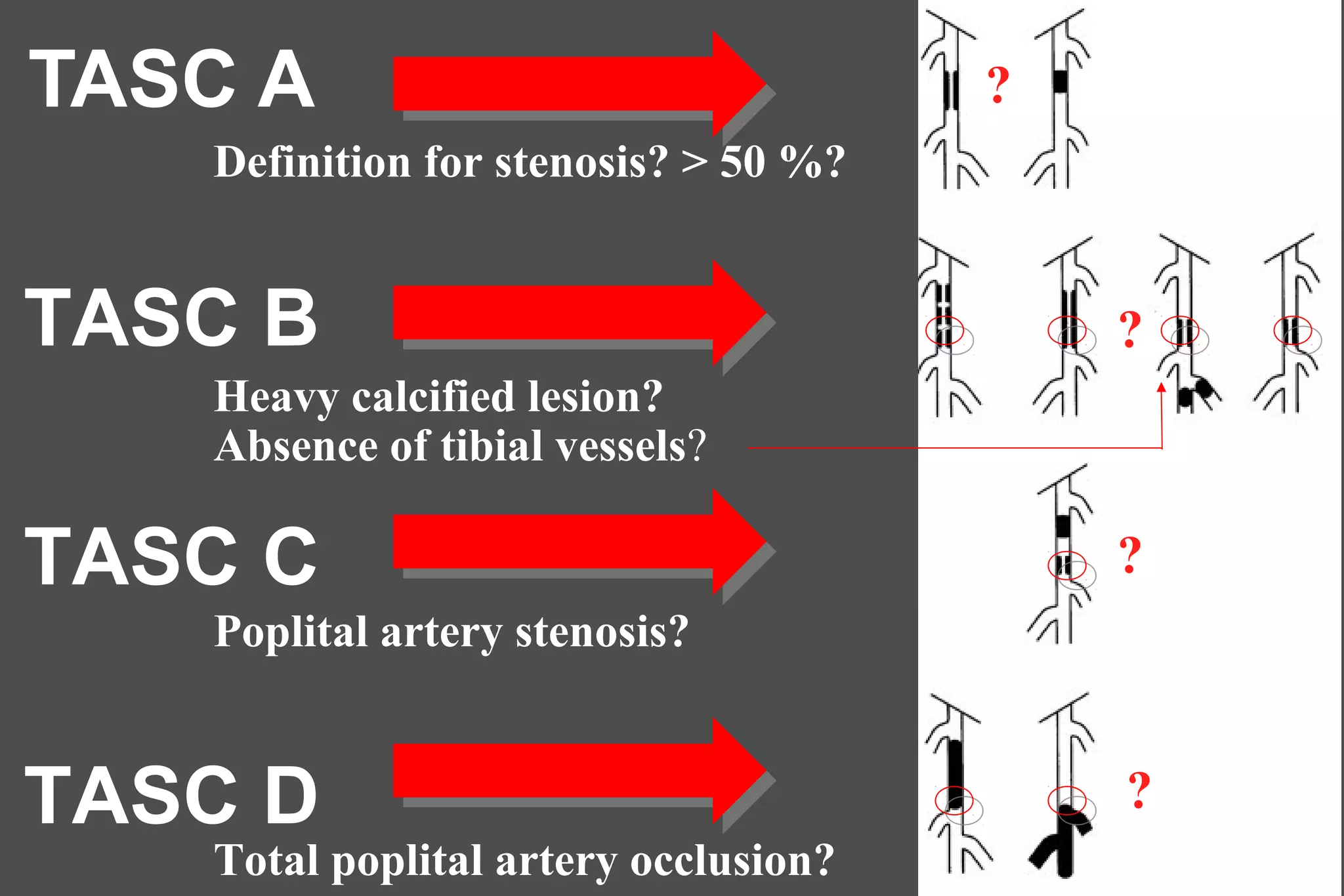
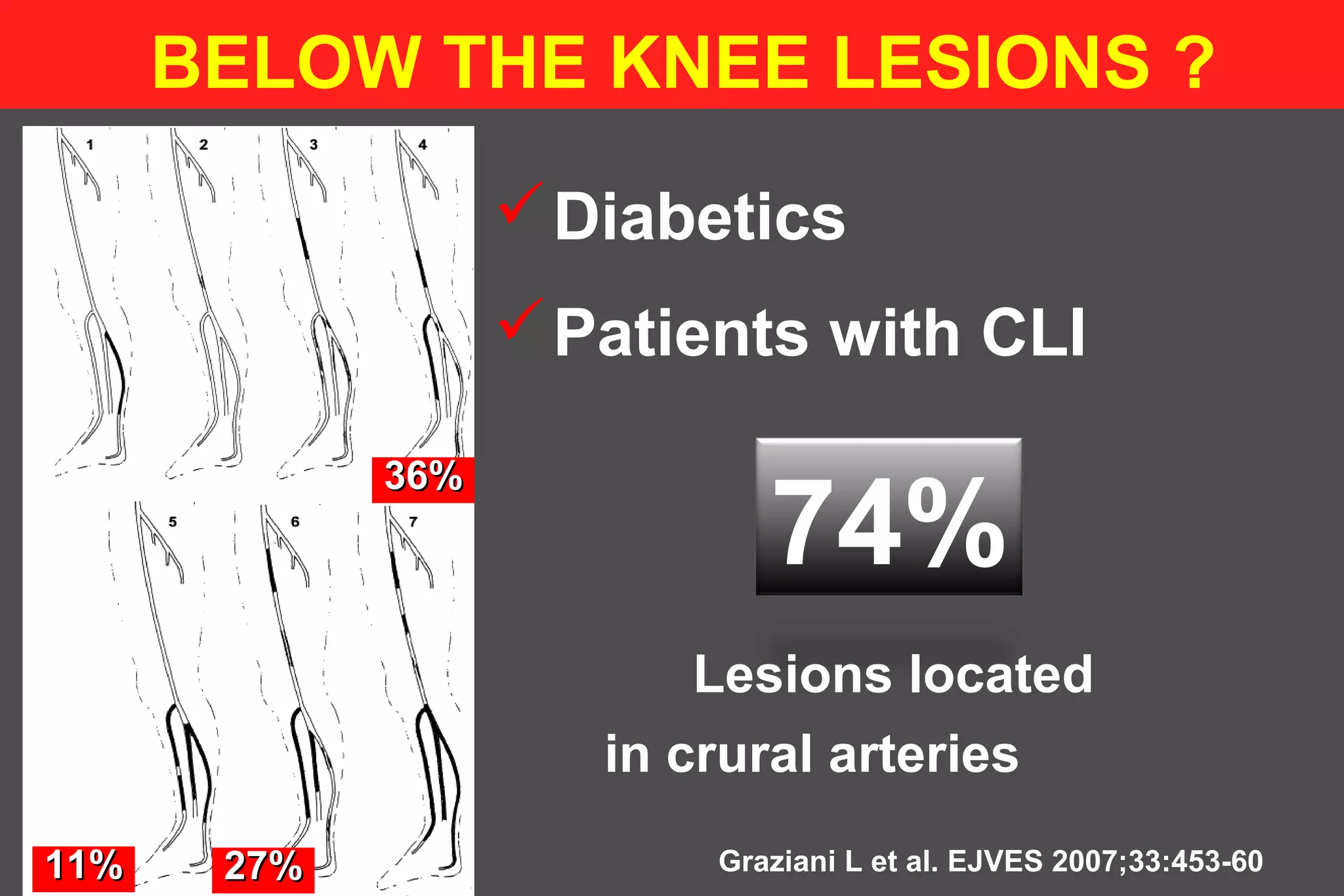

![TASC II B [2011]TASC II B [2011]
• Not endorsed by the SVS and by the ESVS
• Recommendations were not the product of rigorous
scientific scrutinity
• TASC II B advocates an endovascular first option even
in patients with claudication secondary to an isolated
tibial artery disease while there is no Grade A/B
supporting this conclusion](https://image.slidesharecdn.com/chroniccriticallimbischemia-150318094604-conversion-gate01/75/Chronic-critical-limb-ischemia-17-2048.jpg)
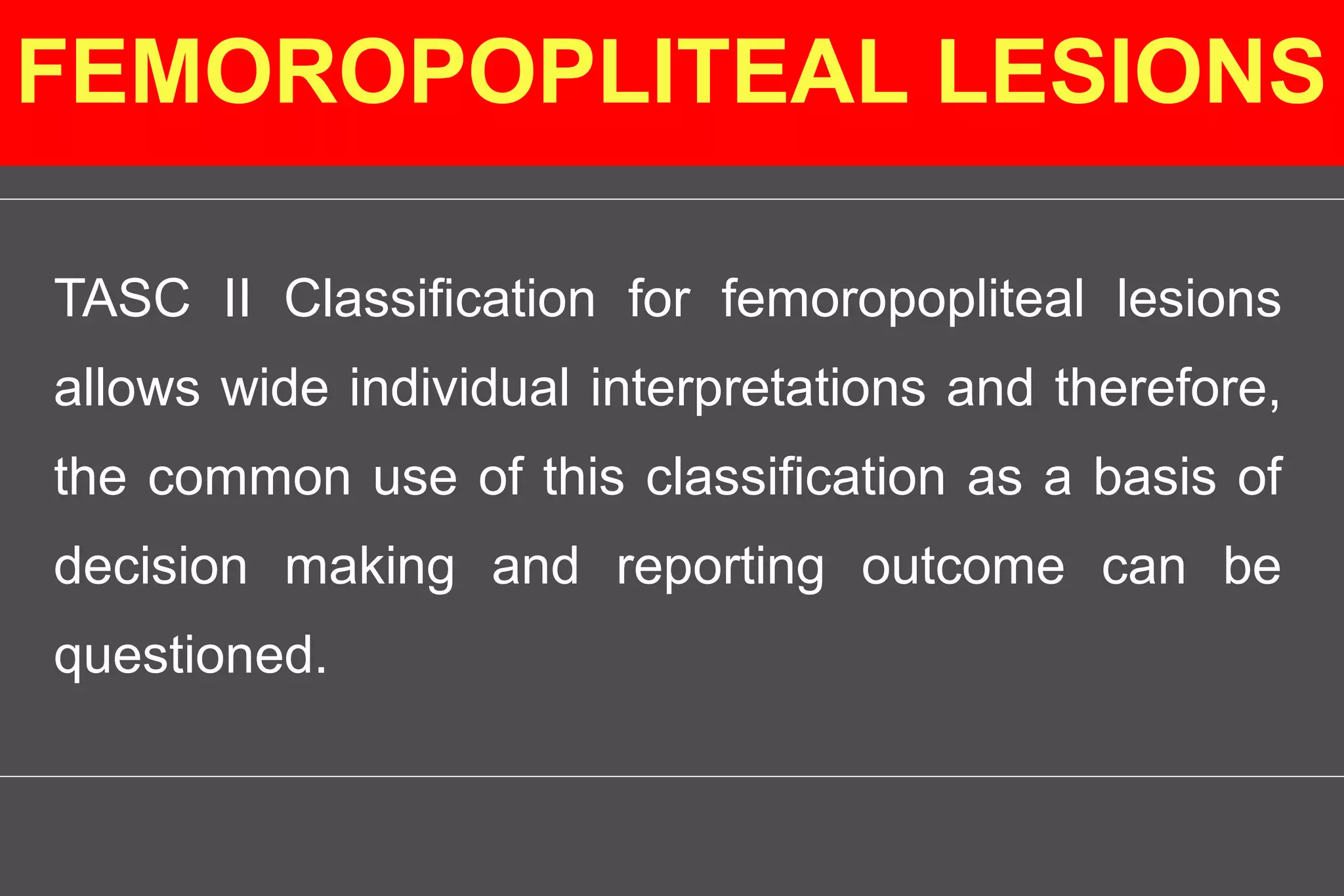
![TASC II B [2011]TASC II B [2011]
TASC II B guidelines adopt a primarily
anatomical approach, which pays
insufficient attention to the clinical
symptoms and risk factors](https://image.slidesharecdn.com/chroniccriticallimbischemia-150318094604-conversion-gate01/75/Chronic-critical-limb-ischemia-18-2048.jpg)
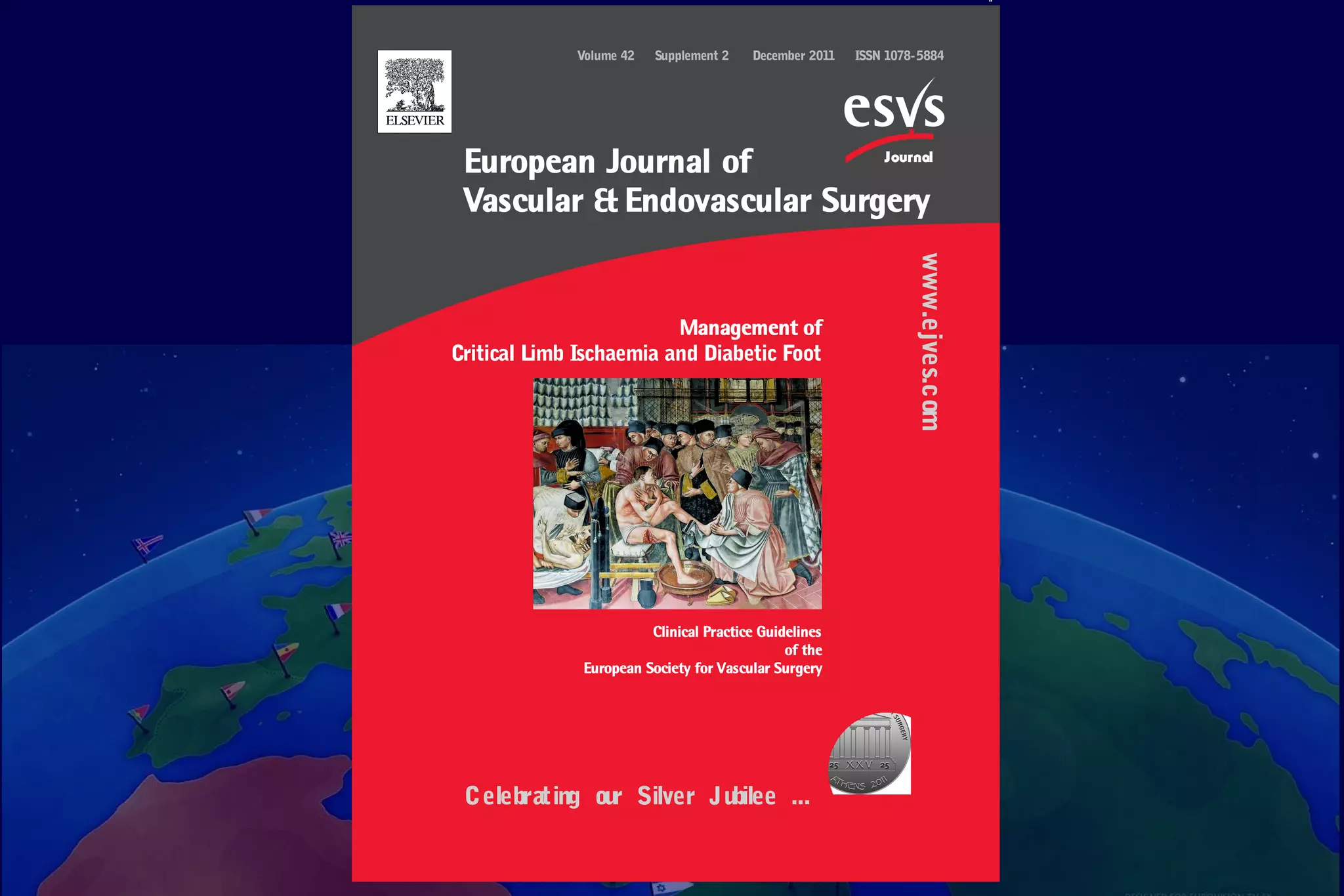







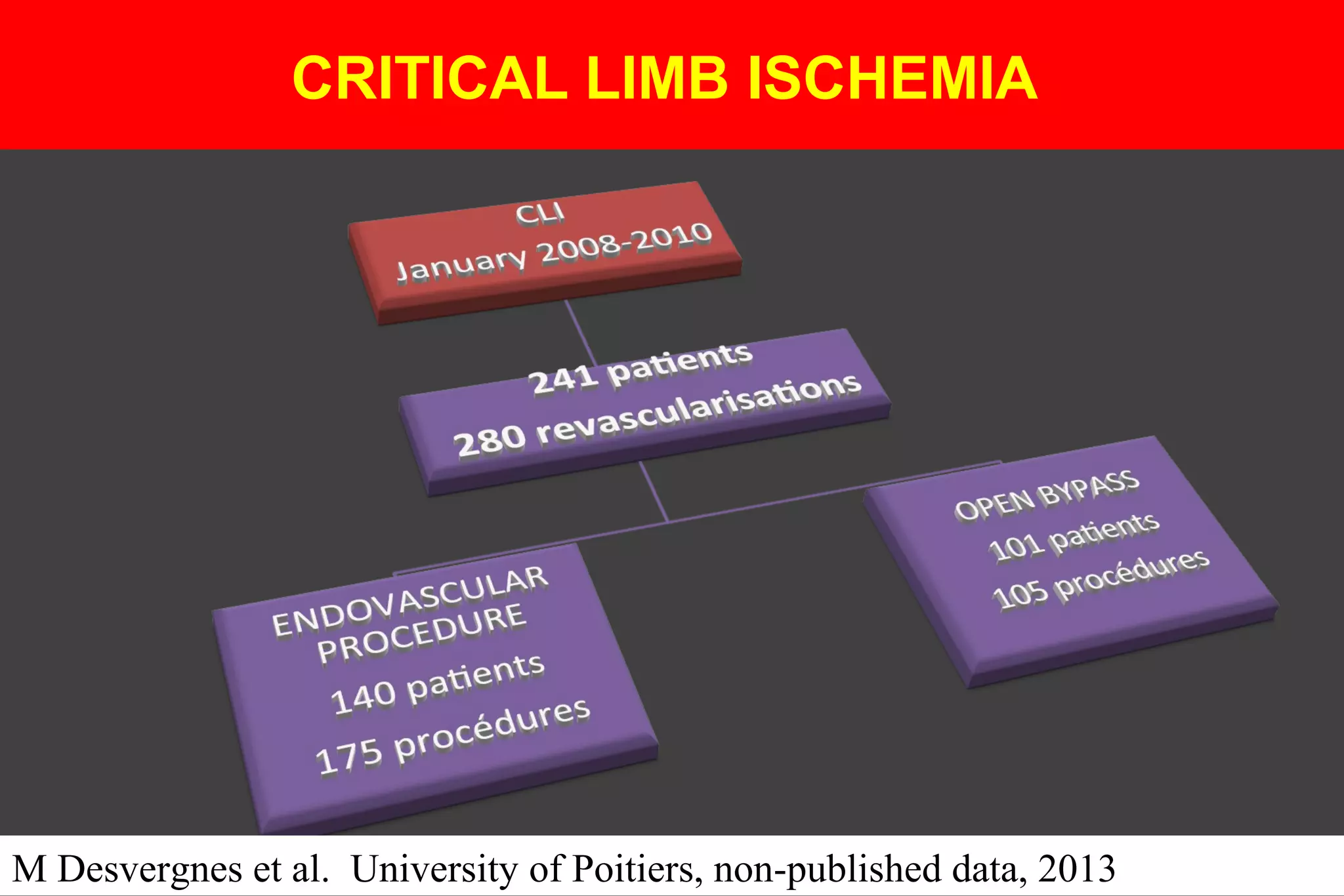
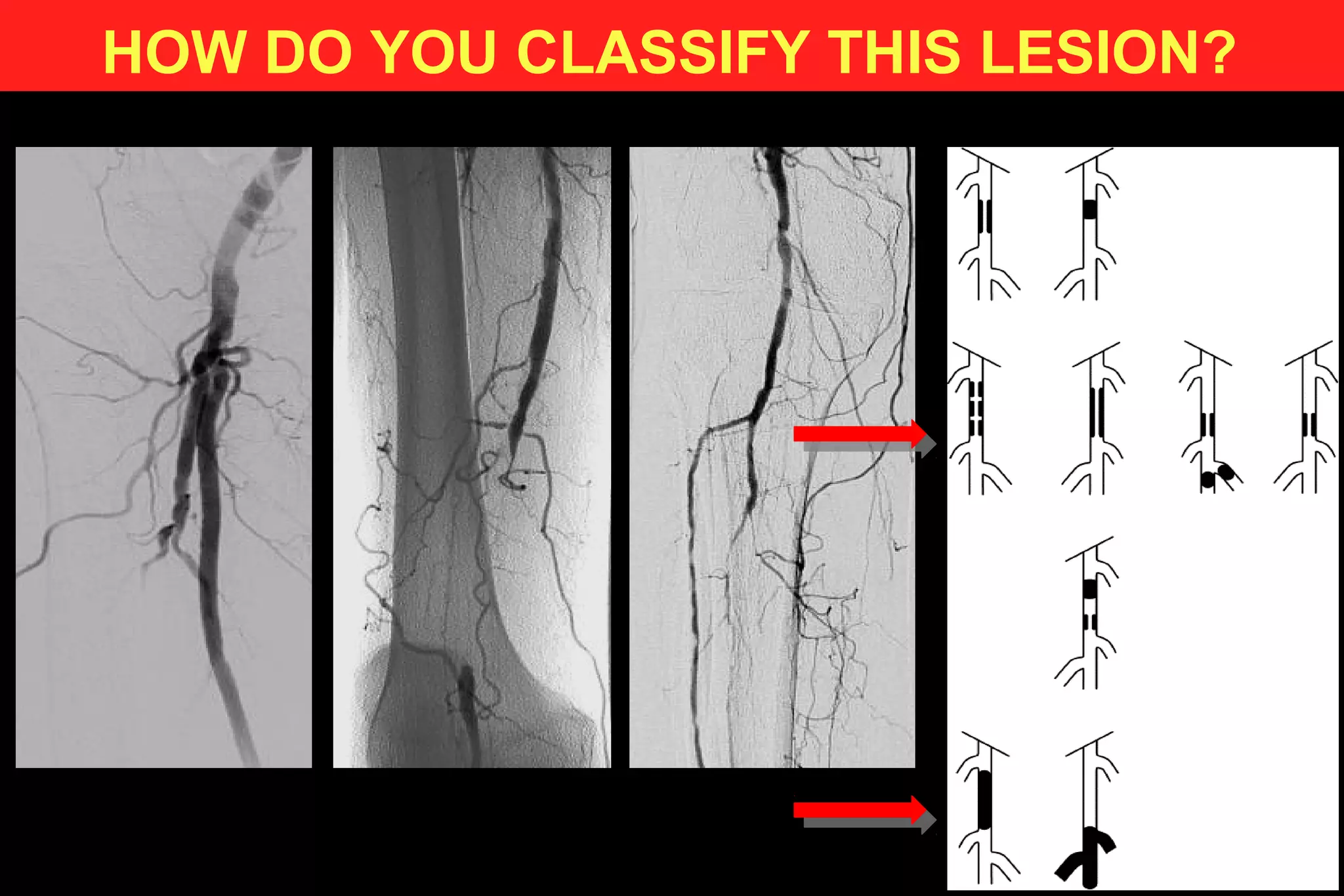
![ENDOVASCULAR PROCEDURES
TASC ? N (%)
A 1 (0,6%)
B 61 (34,9%)
C 75 (42,9%)
D 38 (21,7%)
RUN-OFF [LEG] N (%)
0 23 (13,1%)
1 94 (53,7%)
2 52 (29,7%)
3 6 (3,4%)
M Desvergnes et al. University of Poitiers, non-published data, 2013](https://image.slidesharecdn.com/chroniccriticallimbischemia-150318094604-conversion-gate01/75/Chronic-critical-limb-ischemia-53-2048.jpg)






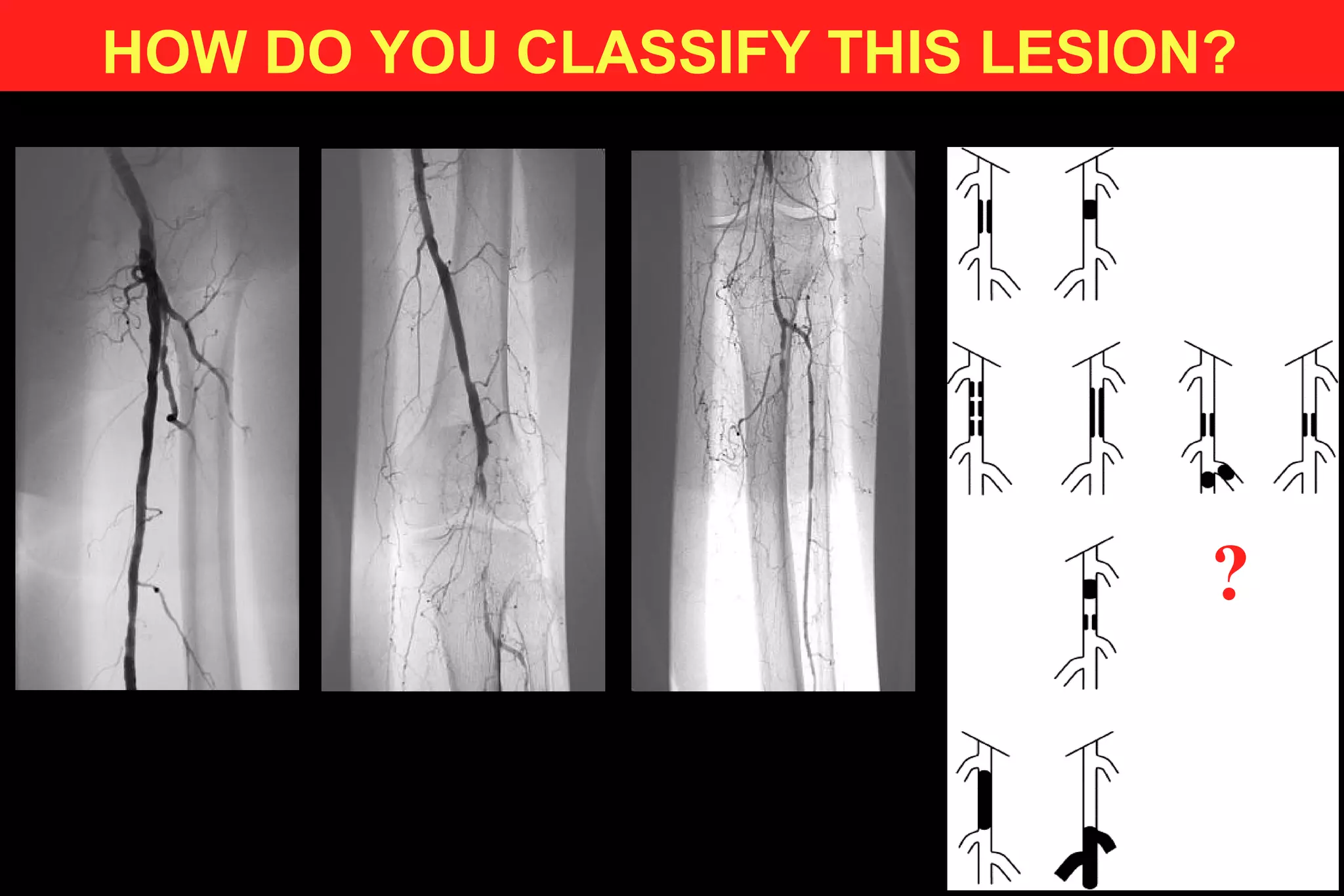
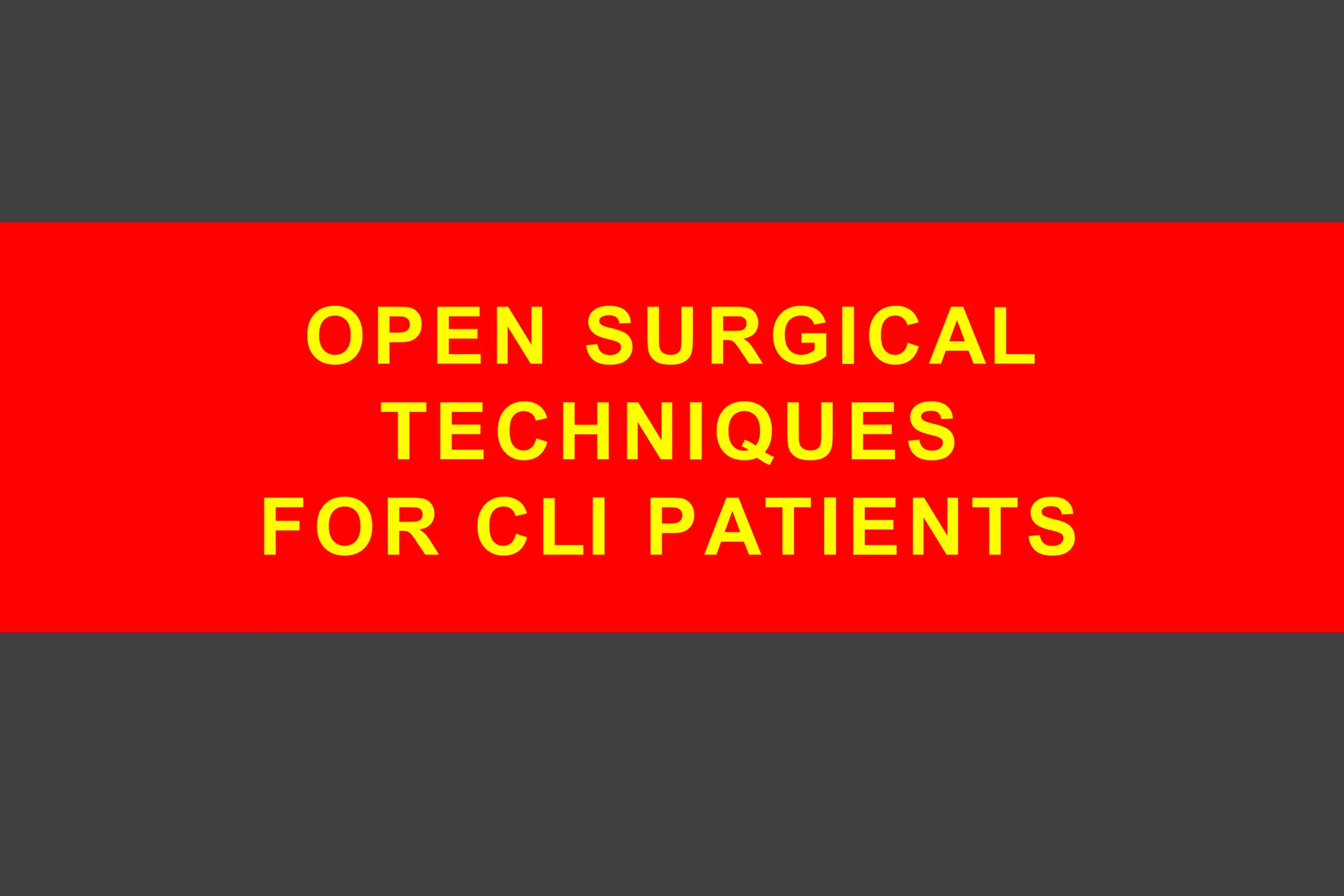
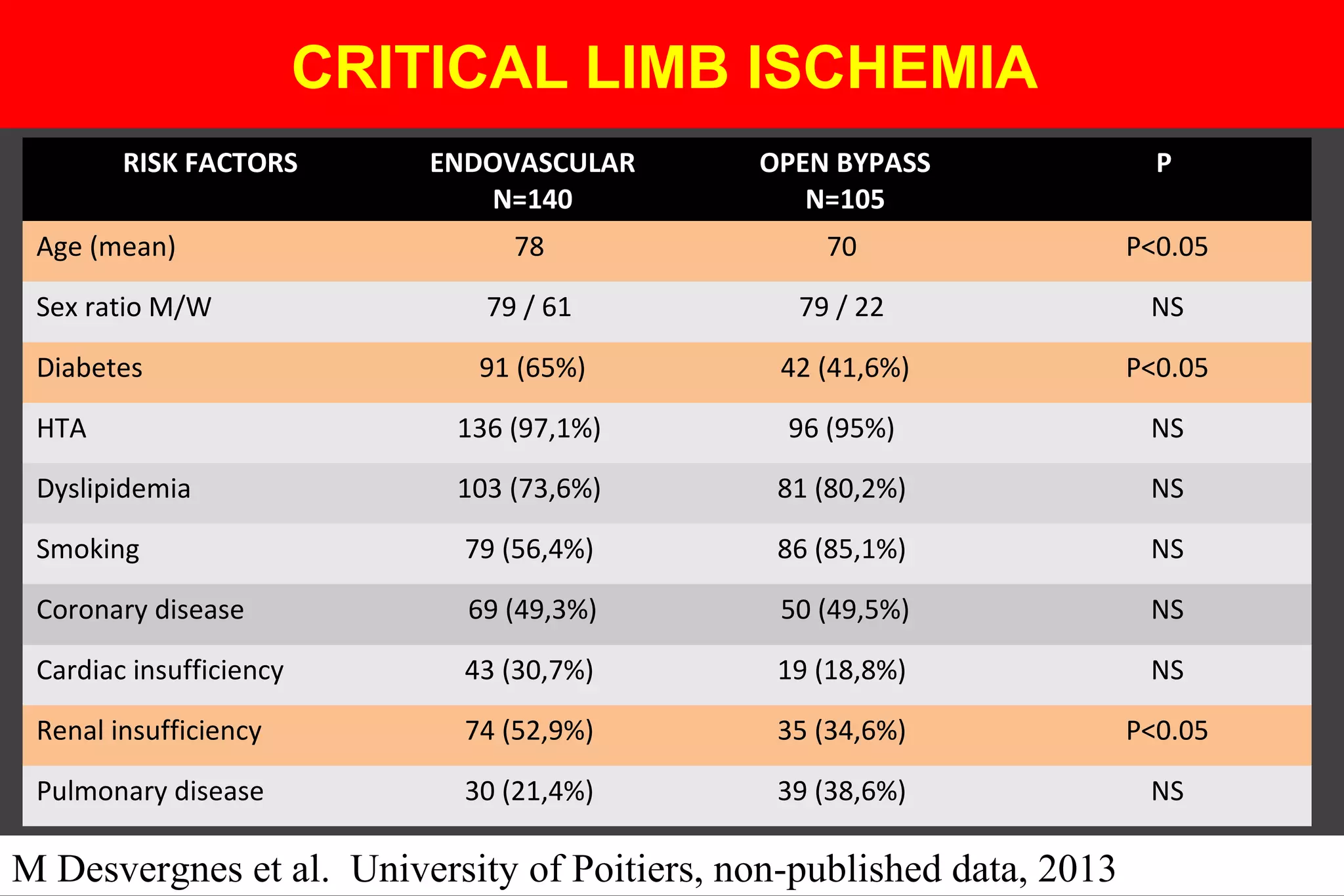
![ANGIOSOMES – CLI PATIENTS
CHU POITIERS
175 ENDOVASCULAR
PROCEDURES
ANGIOSOME
DIRECT
(N=134)
ANGIOSOME
INDIRECT
(N=41)
p
MEAN AGE 77 [42-97] 77,4 [43-89] 0,98
SEX RATIO (M/F) 49,2% 68,9% 0,01
DIABETES 61,9% 78,04% 0,05
RENAL FAILURE 56,7% 48,7% 0,37
HTA 97,7% 97,5% 0,94
CORONARY DISEASE 46,2% 82,9% 0,01
SMOKING 55,9% 58,5% 0,77](https://image.slidesharecdn.com/chroniccriticallimbischemia-150318094604-conversion-gate01/75/Chronic-critical-limb-ischemia-67-2048.jpg)