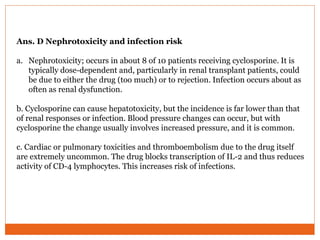
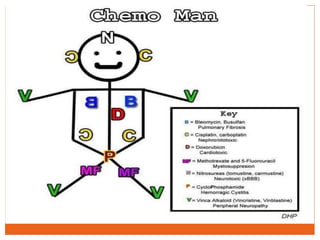
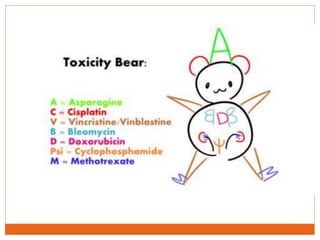
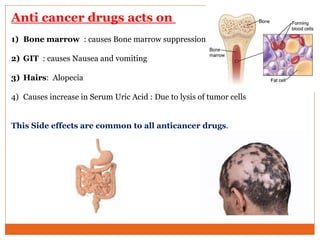
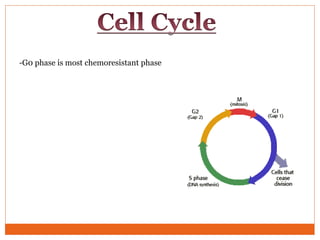
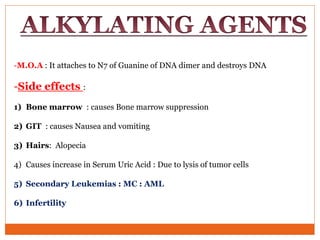
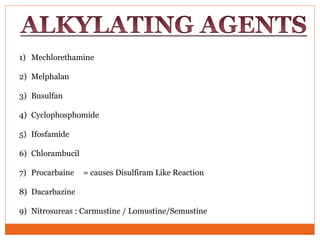
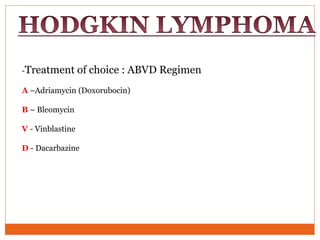
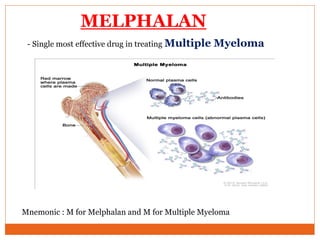
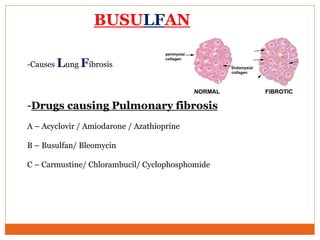
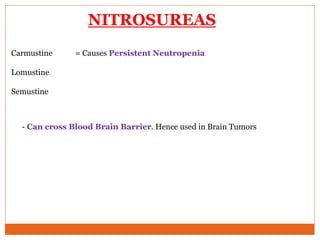
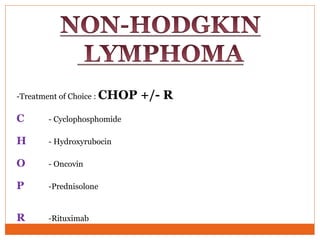
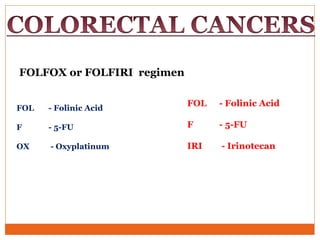
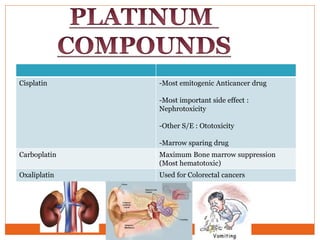
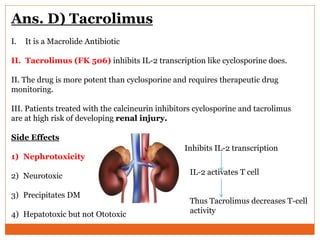
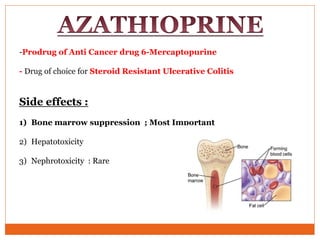
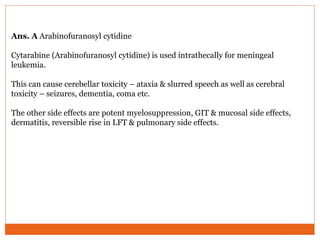
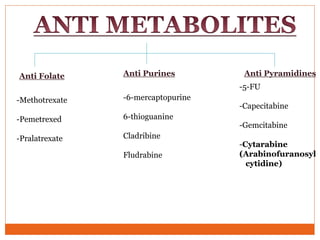
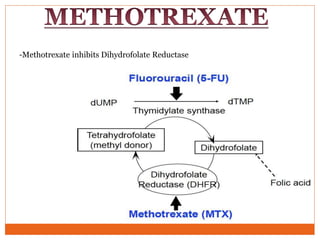
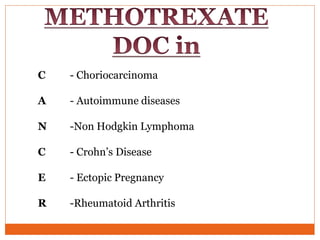
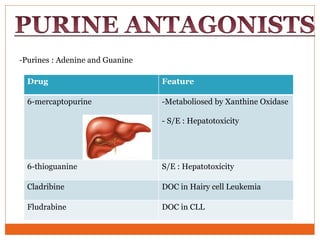
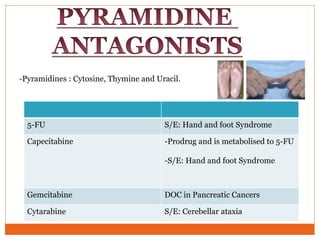
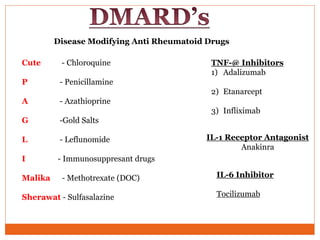
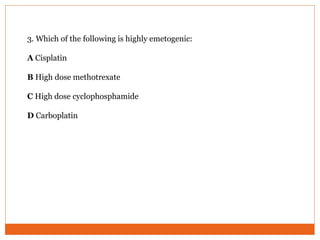
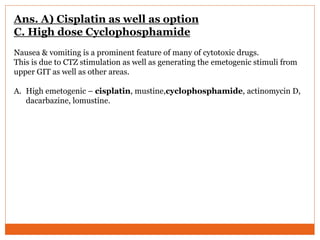
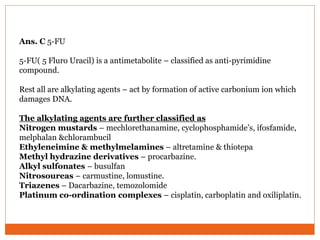
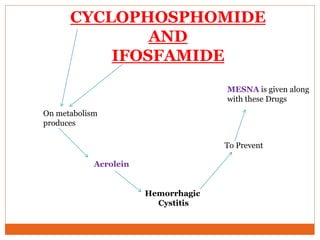
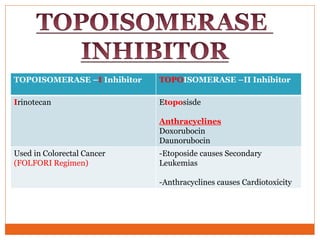
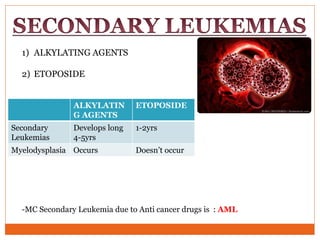
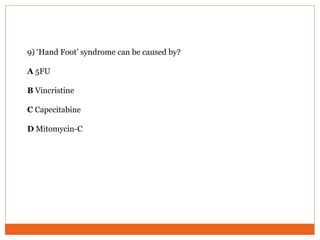
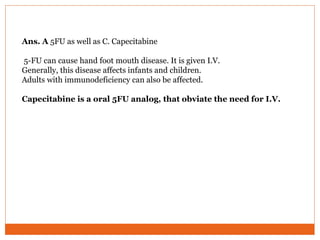
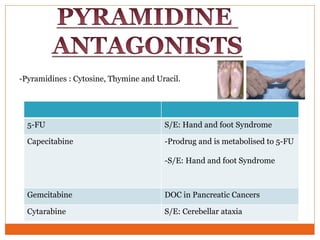
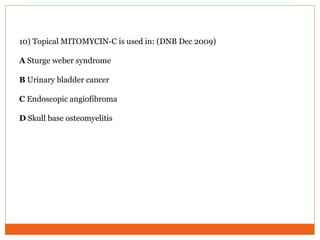
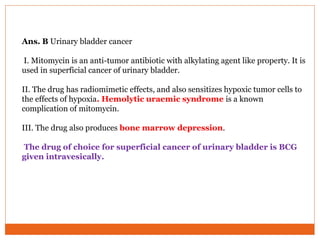
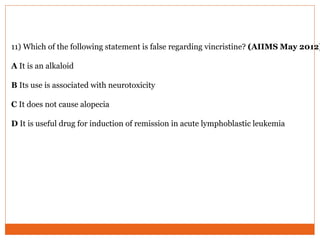
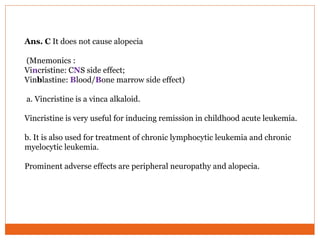
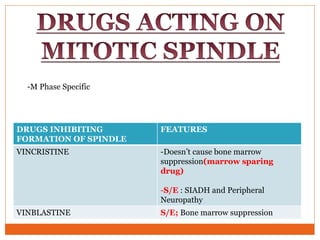
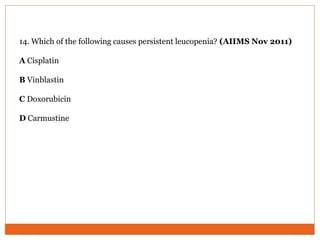
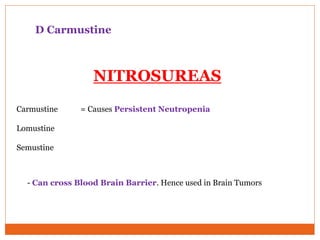
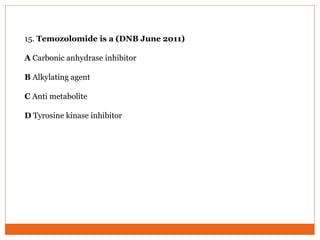
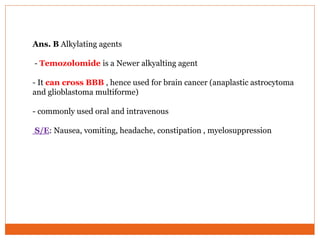
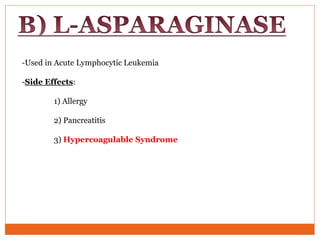
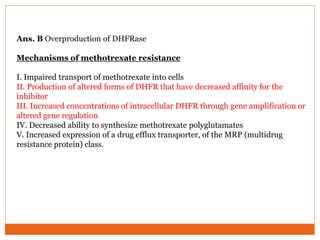
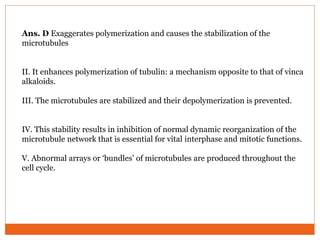
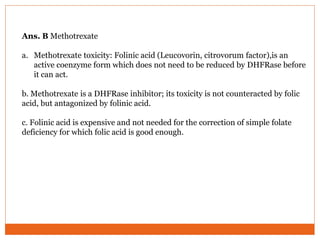
The document outlines various anticancer drugs, detailing their mechanisms of action, side effects, and specific uses in cancer treatment. It discusses alkylating agents, antimetabolites, and their associated toxicities, such as nephrotoxicity, myelosuppression, and gastrointestinal issues. Additionally, it highlights specific drug regimens and side effects for conditions like leukemia and lymphomas.



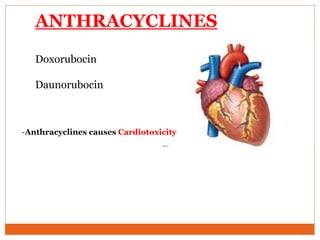

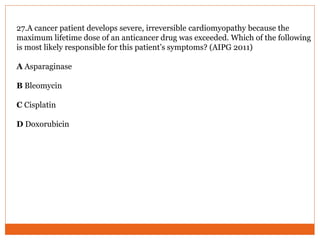
![Ans. D Doxorubicin
I. Doxorubicin, an antitumor antibiotic, is cardiotoxic, and the risk for and
severity of cardiomyopathy is dose-related.
II. [There is a maximum recommended lifetime (cumulative) dose for this
drug, and if it exceed the risk of cardiac damage rises significantly]](https://image.slidesharecdn.com/chemotherapy-170328041010/85/Chemotherapy-96-320.jpg)