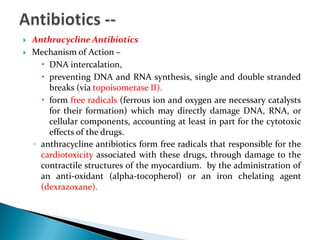
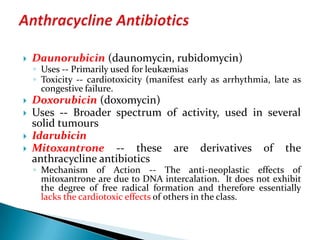
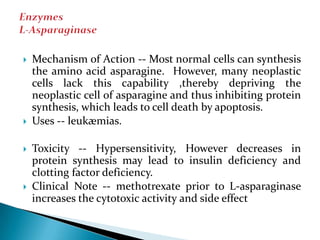
The document discusses various chemotherapeutic agents used to treat cancer and other conditions. It defines key terms related to chemotherapy and describes the mechanisms of action, uses, and toxicities of different classes of cytotoxic drugs including alkylating agents, antimetabolites, anti-mitotic agents, antibiotics, and enzymes. Common drug regimens and chemotherapy strategies such as combination, neoadjuvant, adjuvant, and maintenance chemotherapy are also outlined.