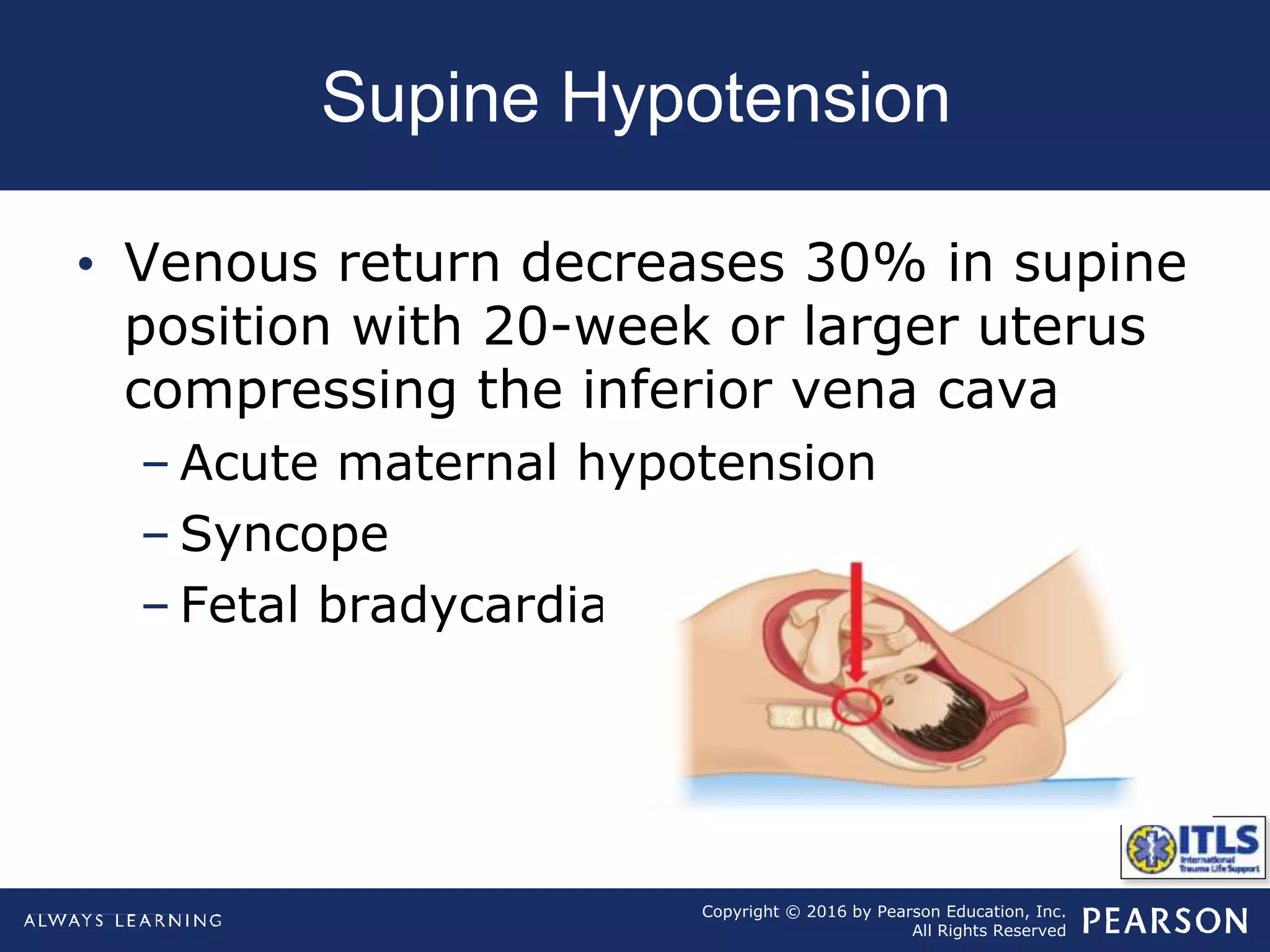
Trauma in pregnancy presents unique challenges as providers must care for both the mother and unborn child. Physiological changes in pregnancy like increased blood volume and an elevated diaphragm can obscure signs of shock. Rapid evaluation and aggressive oxygen and fluid administration are critical to stabilize both patients. Positioning to prevent supine hypotension is also important. Motor vehicle collisions are the leading cause of trauma. Relatively minor abdominal trauma can cause fetal death while maternal death is the most common cause of fetal demise.