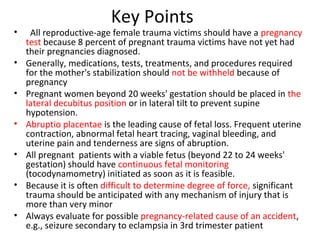
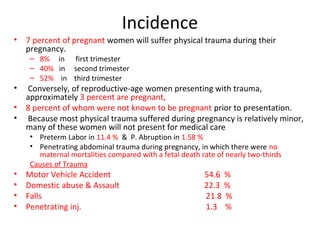
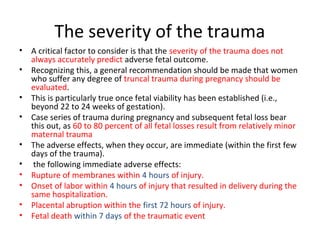
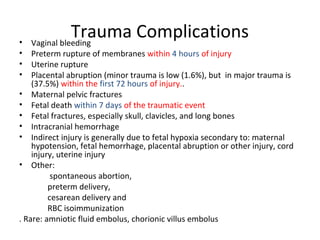
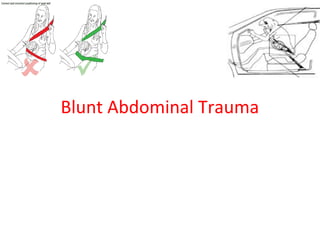
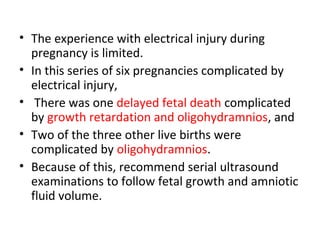
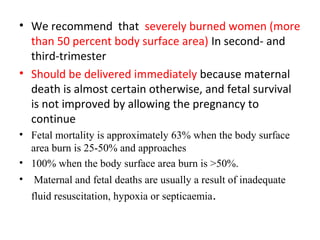
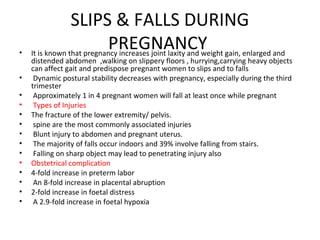
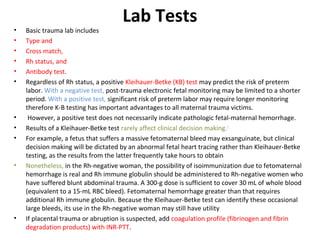
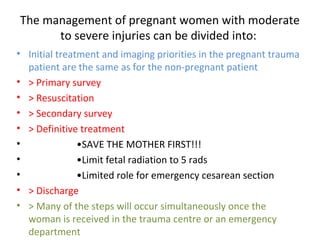
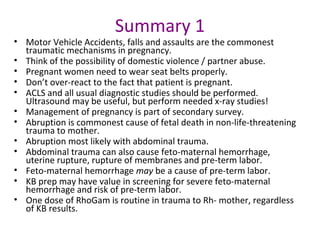
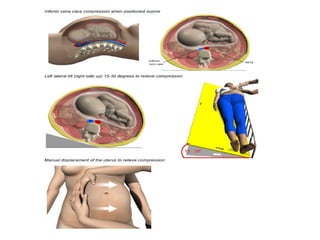
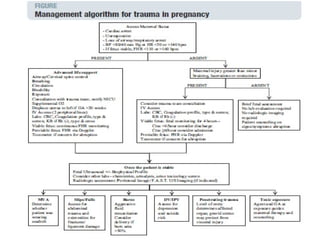
Pregnant women face unique challenges when experiencing trauma. Evaluation of a pregnant trauma patient requires consideration of both the mother and fetus as patients. Knowledge of anatomical and physiological pregnancy changes is important for proper evaluation and management. Minor trauma can still result in adverse fetal outcomes, so even seemingly minor injuries should be evaluated. The fetus is particularly at risk from placental abruption, preterm labor, and reduced blood flow resulting from maternal injury. Proper management of trauma in pregnancy aims to stabilize both patients.