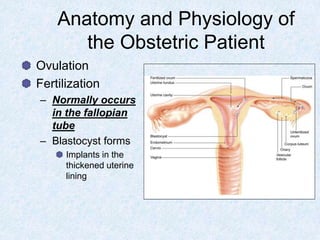
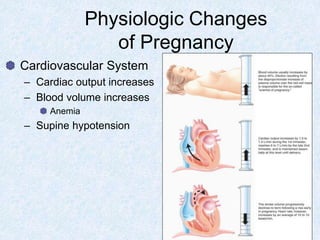
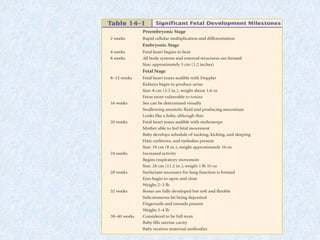
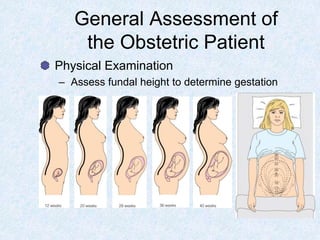
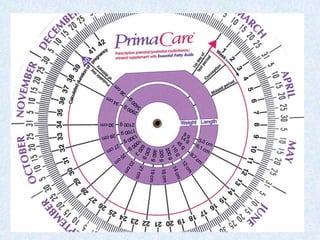
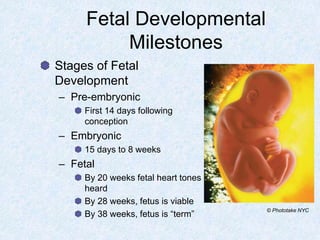
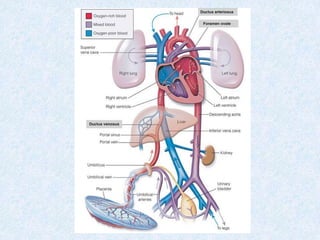
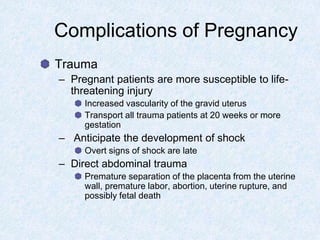
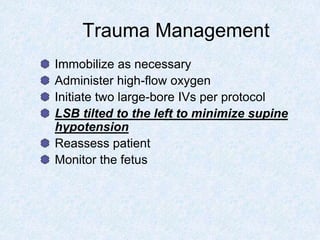
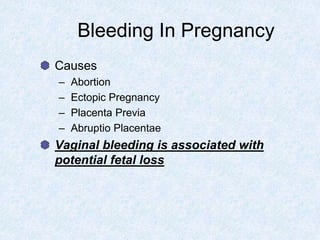
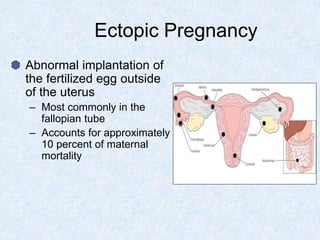
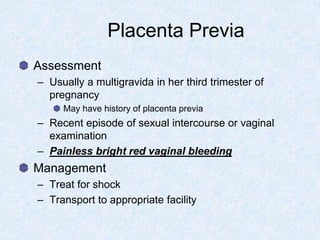
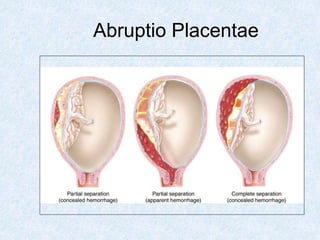
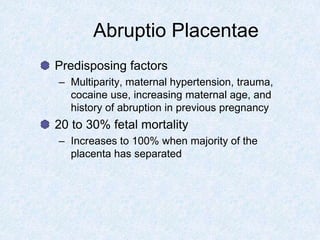
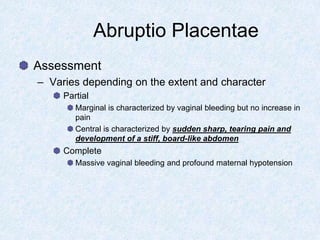
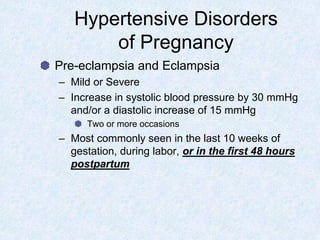
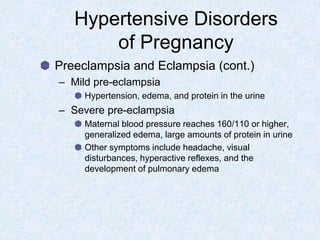
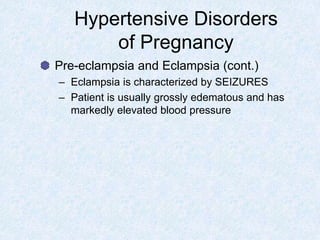
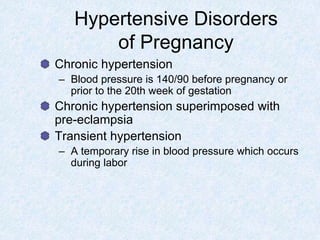
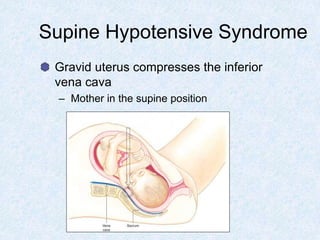
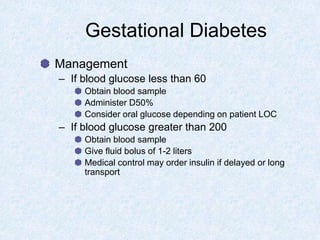
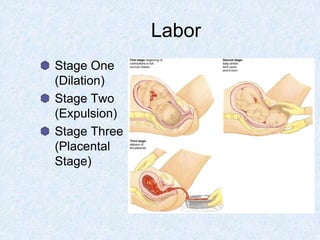
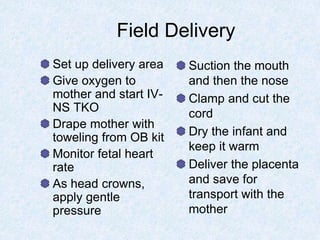
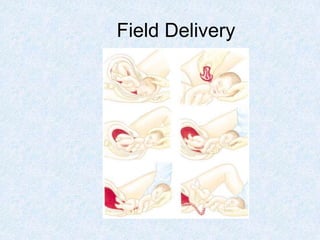
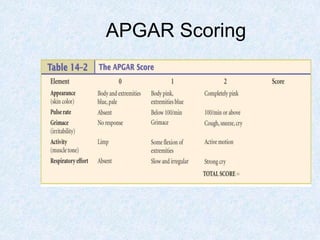
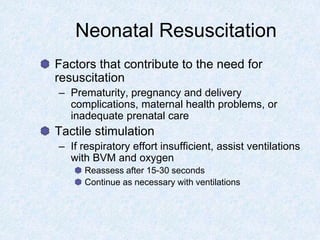
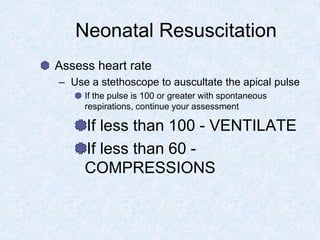
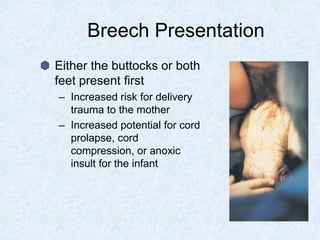
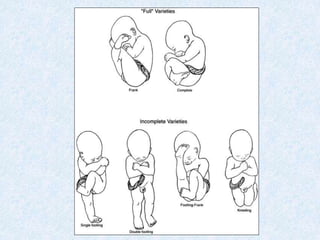
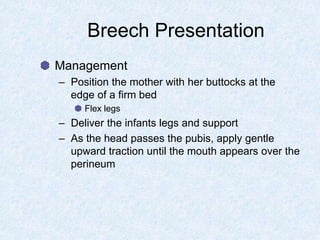
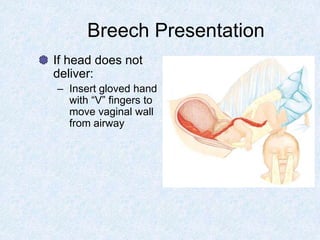
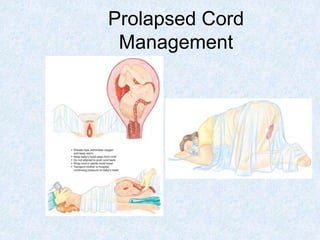
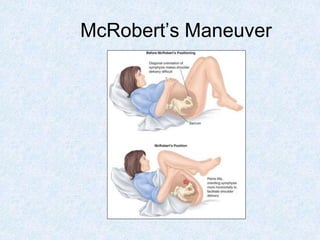
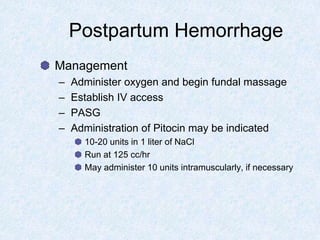
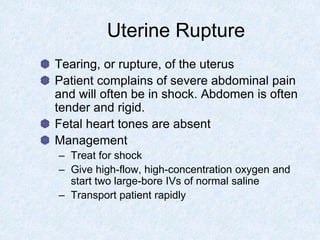
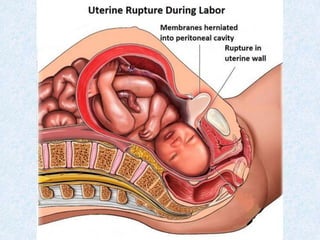
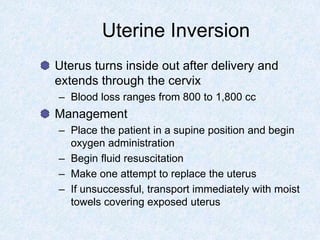
This document discusses paramedic care for obstetric emergencies. It covers topics such as the prenatal period, complications of pregnancy like preeclampsia and gestational diabetes, assessment of patients in labor, management of deliveries, and neonatal resuscitation. Abnormal delivery situations like breech presentation are also addressed. The goal is to provide paramedics with the information needed to properly assess and treat obstetric patients and newborns in the prehospital setting.