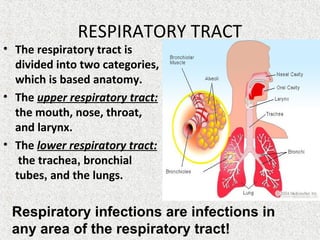
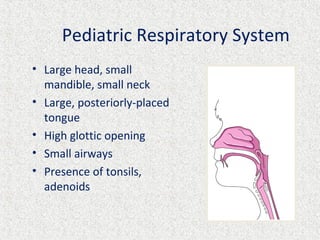
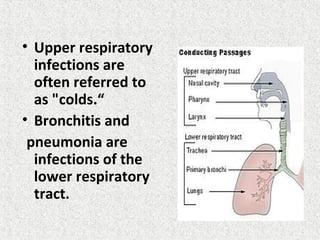
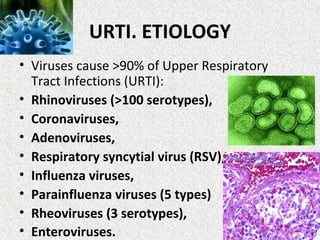
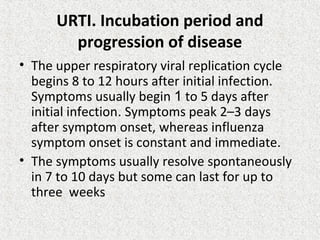
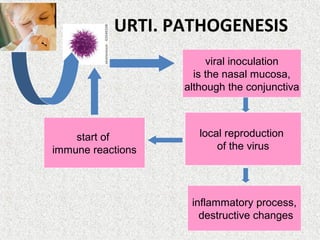
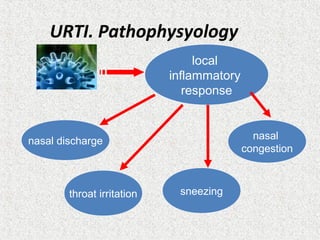
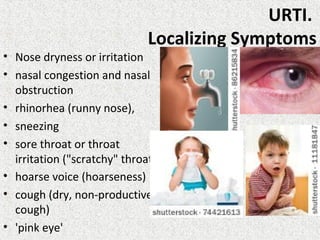
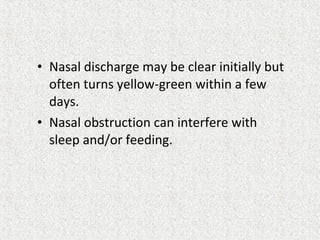
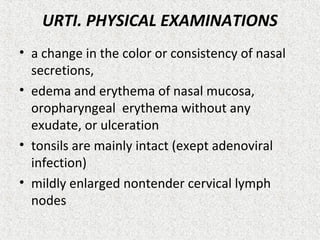
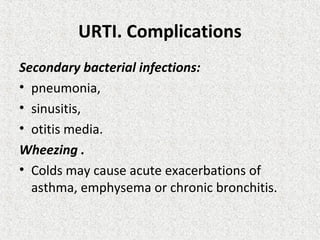
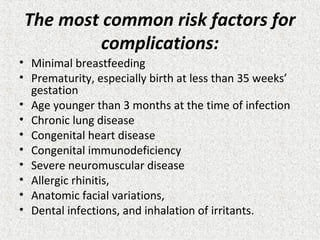
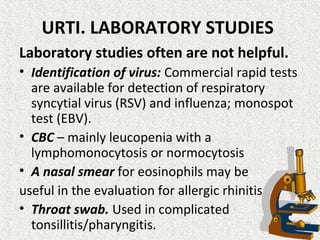
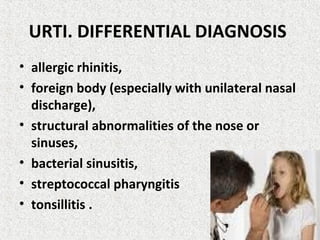
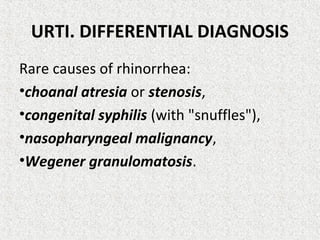
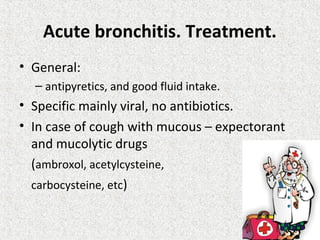
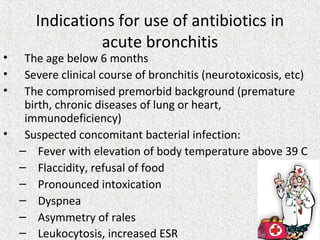
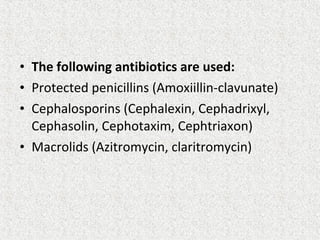
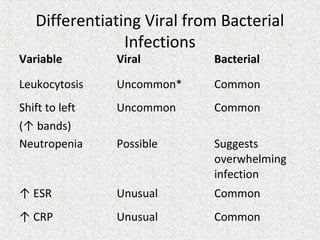
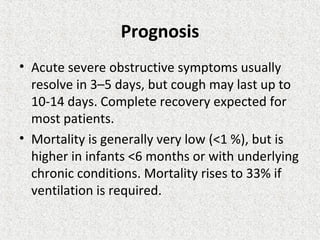
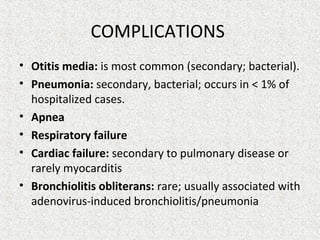
The document discusses acute upper respiratory infections in children. It defines acute upper respiratory infections and lists common causes like viruses. It describes the symptoms, signs, and typical progression of a common cold. Diagnosis is usually made clinically based on symptoms. Treatment focuses on relieving symptoms like fever, nasal congestion, and cough through rest, hydration, nasal saline, and over-the-counter medications. Complications can include secondary bacterial infections.