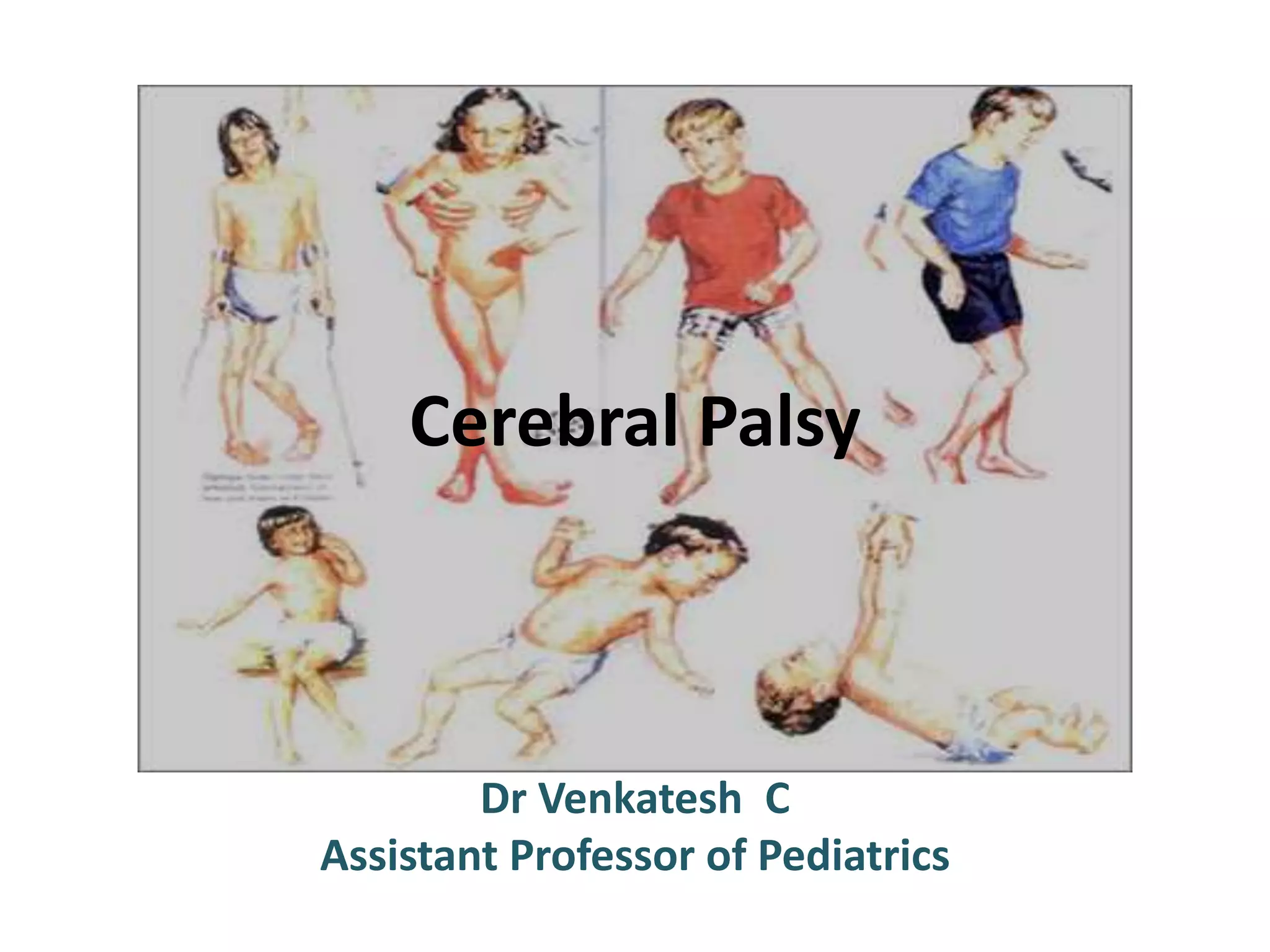
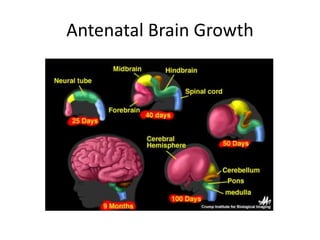
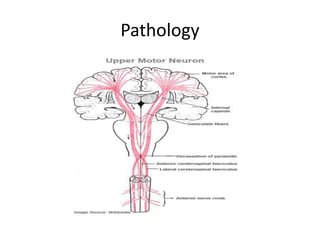
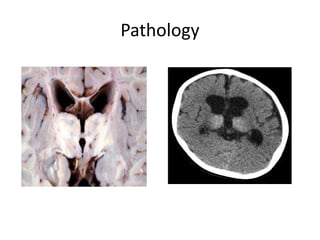
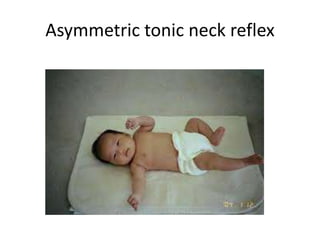
Cerebral palsy is a disorder of movement and posture caused by a non-progressive brain insult during fetal or infant development. It has an incidence of 1 in 500 births and is a major cause of childhood disability. The majority of cases are caused by prenatal factors. While there is no cure, prevention through proper antenatal care and fetal monitoring is key. Cerebral palsy manifests through increased muscle tone, involuntary movements, poor coordination, and other motor impairments depending on the type and severity. Treatment requires a multidisciplinary approach focusing on stimulation, nutrition, therapy, and managing comorbidities like seizures.