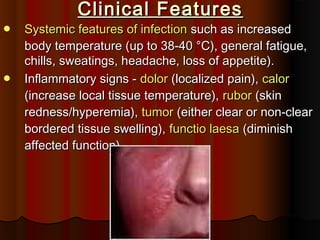
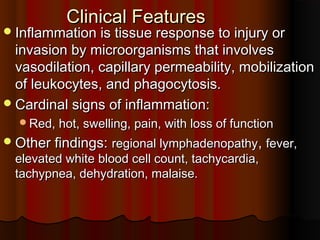
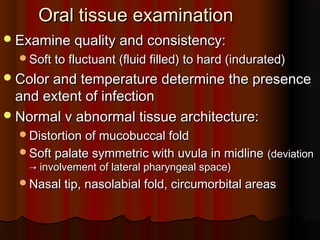
1. The document discusses cellulitis, a bacterial skin infection causing inflammation. It defines cellulitis and describes its symptoms such as red, swollen, tender skin.
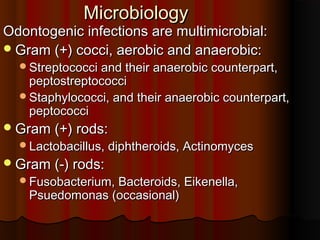
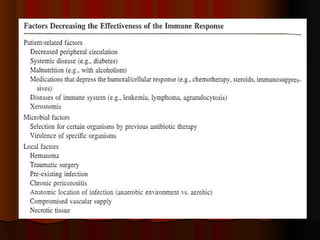
2. Common causes are bacteria like streptococcus and staphylococcus entering through breaks in the skin. Risk factors include injuries, conditions like eczema or diabetes.
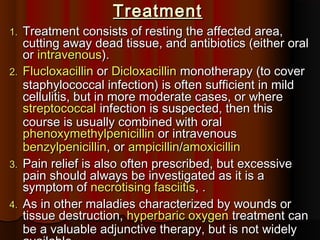
3. Diagnosis involves examination of the affected area and sometimes tests. Treatment focuses on antibiotics, wound care, and rest.
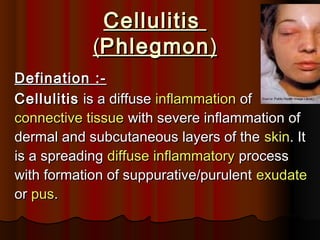
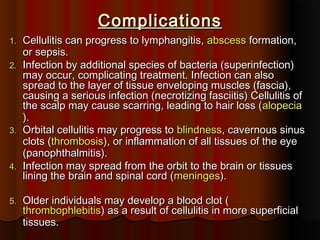
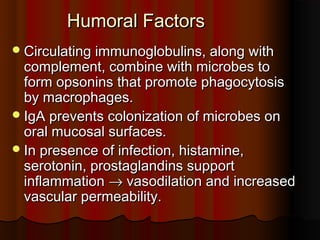
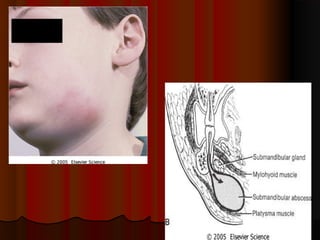
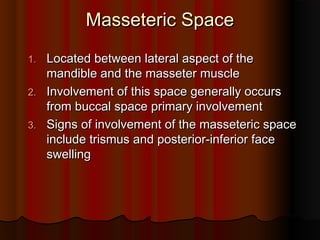
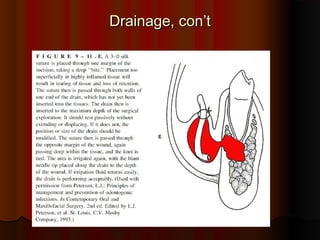
![1.1. Cellulitis can be caused by normalCellulitis can be caused by normal skin floraskin flora or byor by
exogenous bacteriaexogenous bacteria[[streptococcus and/orstreptococcus and/or
staphylococcus bacteria]staphylococcus bacteria]..
2.2. Often occurs where the skin has previously beenOften occurs where the skin has previously been
broken: cracks in the skin, cuts,broken: cracks in the skin, cuts, blistersblisters,, burnsburns,,
insect bitesinsect bites,, surgical woundssurgical wounds, or sites of, or sites of
intravenousintravenous cathetercatheter insertion.insertion.
3.3. Skin on the face is most commonly affected bySkin on the face is most commonly affected by
this infection, though cellulitis can occur on anythis infection, though cellulitis can occur on any
part of the body.part of the body.
4.4. The mainstay of therapy remains treatment withThe mainstay of therapy remains treatment with
appropriateappropriate antibioticsantibiotics, and recovery periods can, and recovery periods can
INTRODUCTION :-](https://image.slidesharecdn.com/cellulitis-110219224340-phpapp01-150326065939-conversion-gate01/85/Cellulitis-110219224340-phpapp01-3-320.jpg)









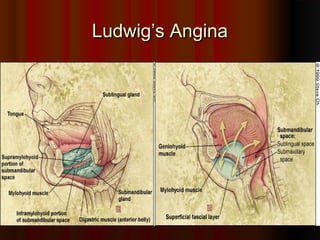
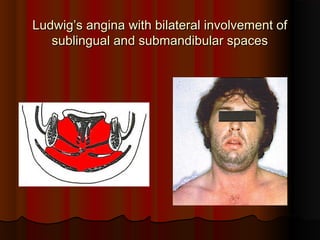
![DEFINATIONDEFINATION
Ludwig's angina, otherwise known as angina ludovici, is aLudwig's angina, otherwise known as angina ludovici, is a
serious, potentially life-threateningserious, potentially life-threatening cellulitiscellulitis[1][1], or, or
connective tissue infection, of the floor of the mouth,connective tissue infection, of the floor of the mouth,
usually occurring in adults with concomitant dentalusually occurring in adults with concomitant dental
infections. It is named after the German physician,infections. It is named after the German physician,
Wilhelm Friedrich von LudwigWilhelm Friedrich von Ludwig who first described thiswho first described this
condition in 1836.condition in 1836.[2][2][3][3] Other names include "anginaOther names include "angina
Maligna" and "Morbus Strangularis".Maligna" and "Morbus Strangularis".
Ludwig's angina should not be confused withLudwig's angina should not be confused with
angina pectorisangina pectoris, which is also otherwise commonly known, which is also otherwise commonly known
as "as "anginaangina". The word "". The word "anginaangina" comes from the" comes from the GreekGreek
wordword ankhonankhon, meaning "strangling", so in this case,, meaning "strangling", so in this case,
Ludwig's angina refers to the feeling of strangling, not theLudwig's angina refers to the feeling of strangling, not the
feeling of chest pain, though there may be chest pain infeeling of chest pain, though there may be chest pain in
Ludwig's angina if the infection spreads into theLudwig's angina if the infection spreads into the](https://image.slidesharecdn.com/cellulitis-110219224340-phpapp01-150326065939-conversion-gate01/85/Cellulitis-110219224340-phpapp01-82-320.jpg)