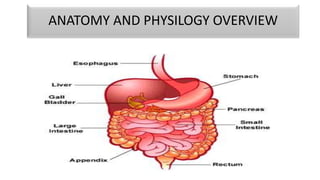
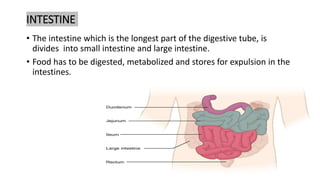
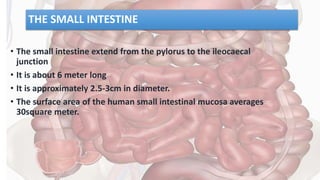
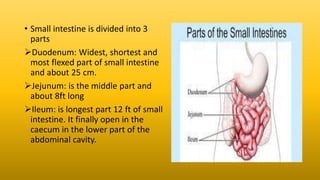
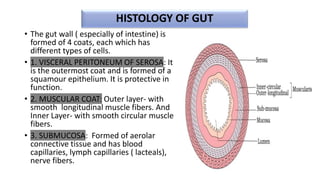
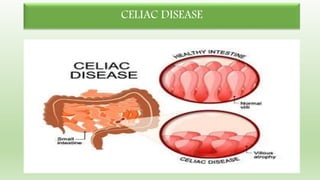
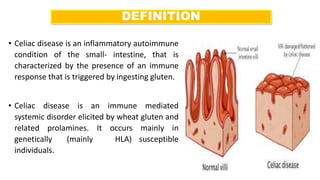
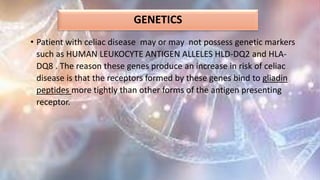
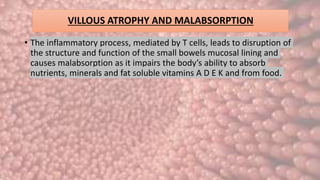
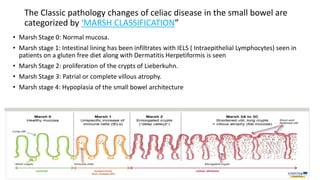
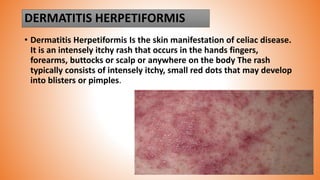
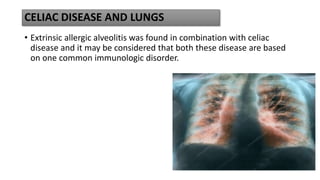
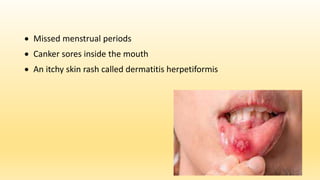
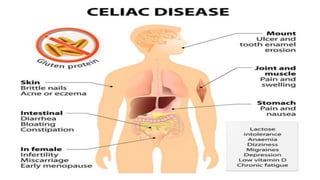
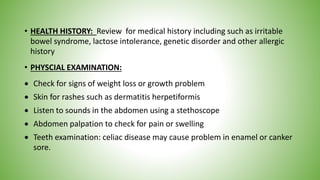
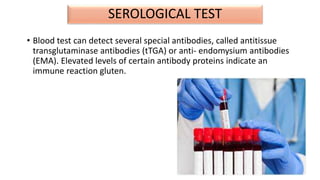
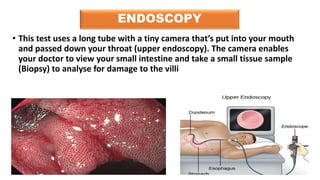
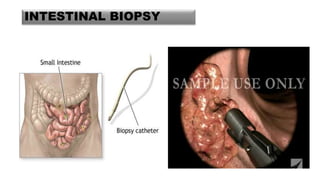
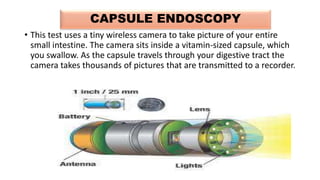
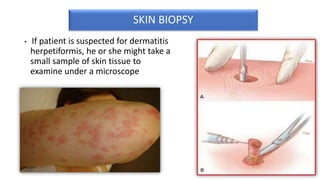
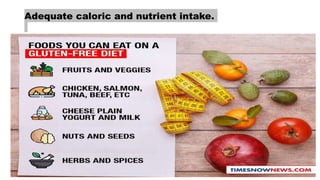
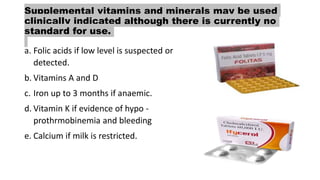
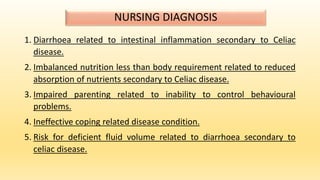
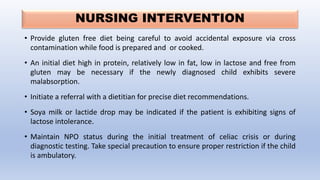
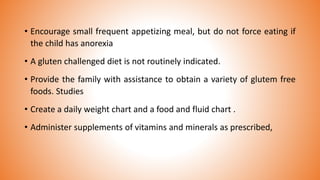
The document provides an overview of Celiac Disease presented by Bhavya Sharma. It discusses the anatomy and histology of the small intestine, causes and risk factors of Celiac Disease including genetics and prolamin proteins. The pathophysiology involves an immune response triggered by ingesting gluten that damages villi in the small intestine and interferes with nutrient absorption. Signs and symptoms along with diagnostic tests are described, including blood tests, endoscopy and biopsy of the small intestine. Treatment involves maintaining a strict lifelong gluten-free diet.