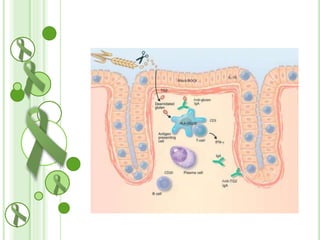
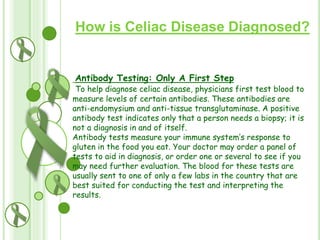
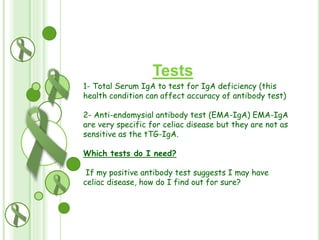
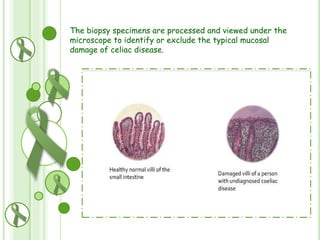
Celiac disease is an autoimmune disorder triggered by ingesting gluten, which damages the small intestine's lining. It affects about 1 in 100 people worldwide. The disease is caused by an interaction between gluten and the small intestine in genetically predisposed individuals. There is no cure, but following a strict gluten-free diet can help manage symptoms and prevent complications like osteoporosis and intestinal cancer. A biopsy of the small intestine is required for diagnosis to confirm the characteristic damage to intestinal villi.