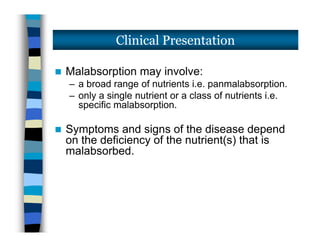
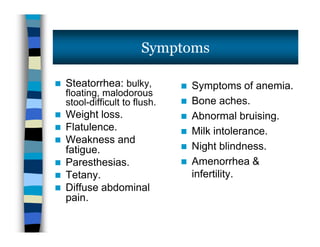
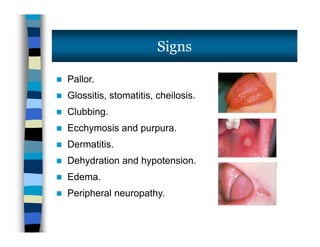
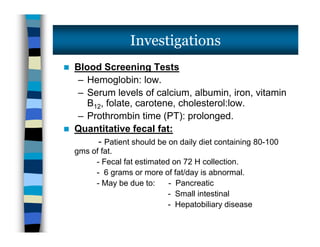
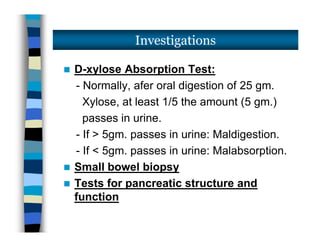
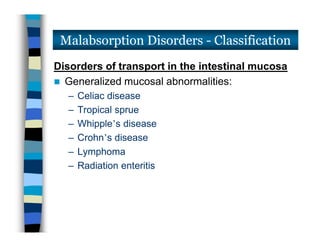
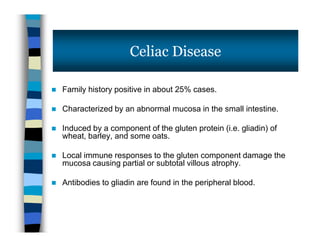
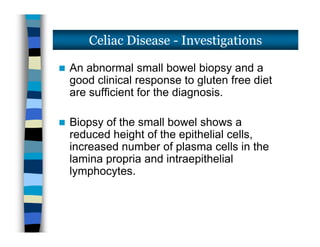
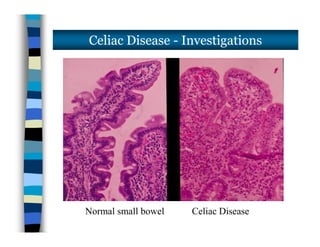
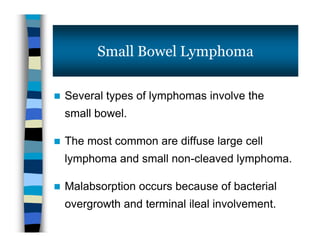
The document discusses malabsorption syndromes and provides details about celiac disease. It defines celiac disease as an immune-mediated disorder caused by ingestion of gluten, which damages the small intestine mucosa. Key points include that celiac disease is diagnosed by small bowel biopsy showing villous atrophy and response to gluten-free diet, and that complications can include lymphoma, ulcerative jejunoileitis and dermatitis herpetiformis.