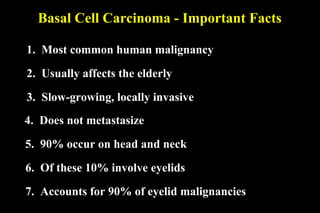
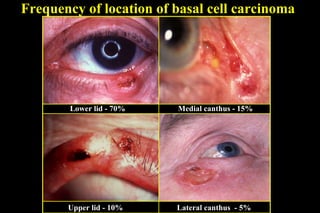
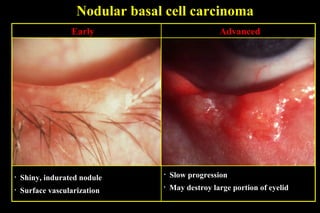
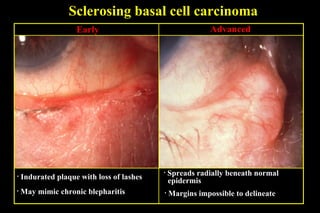
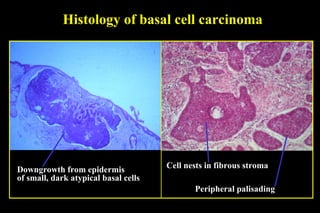
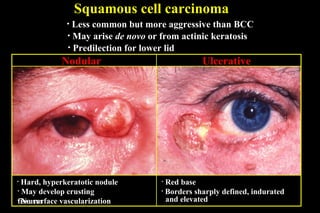
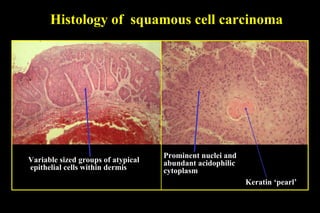
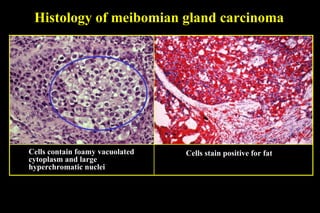
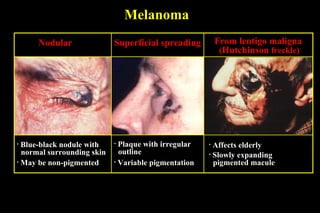
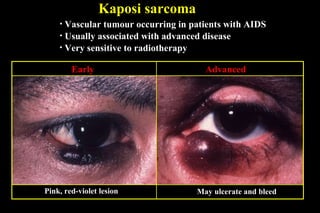
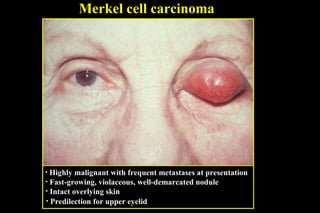
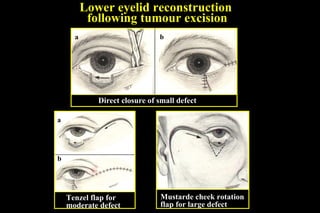
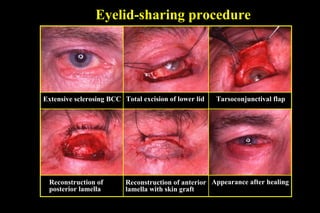
This document summarizes different types of malignant eyelid tumors including basal cell carcinoma, squamous cell carcinoma, meibomian gland carcinoma, melanoma, Kaposi sarcoma, and Merkel cell carcinoma. It describes characteristics such as appearance, location, histology, and treatment options for each type of tumor. The most common is basal cell carcinoma, which typically affects the elderly on the head and neck region, grows slowly, and has a low risk of metastasis. Surgical excision is the primary treatment but other options include cryotherapy and radiotherapy. Reconstruction of the eyelid may require various flap procedures depending on the size of the defect.