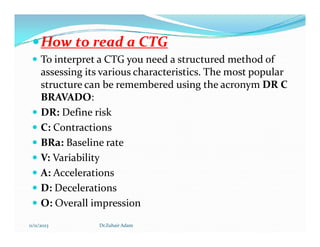
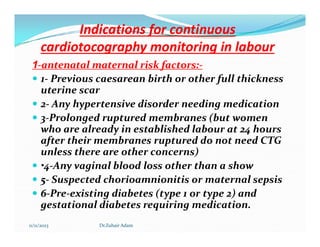
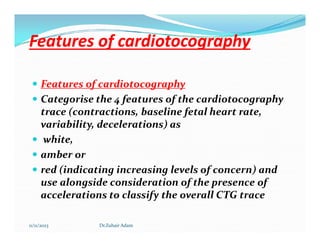
This document provides information about cardiotocography (CTG) monitoring during pregnancy and labor. It discusses what CTG is, how to interpret a CTG trace using the DR C BRAVADO method, indications for continuous CTG monitoring during labor based on maternal and fetal risk factors, features of the CTG trace categorized as white/normal, amber/suspicious, or red/pathological, and definitions of contractions, baseline fetal heart rate, variability, accelerations, and decelerations. The document aims to guide healthcare providers on how to properly conduct and interpret CTG monitoring to evaluate fetal well-being during pregnancy and labor.







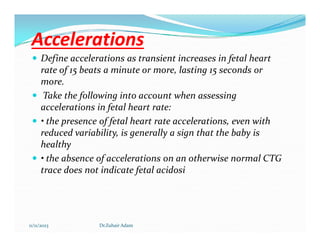



























![ In the second stage of labour:
if fetal heart rate accelerations are recorded, be aware that these
are most likely to be maternal pulse.
• if fetal heart rate decelerations are recorded, look for other
signs of hypoxia (for example, a rise in the baseline fetal heart
rate or a reduction in variability).
Take into account that onset of hypoxia is both more common
and more rapid in the active second stage of labour. Take an
increase in the baseline fetal heart rate of 20 beats a minute or
increase in the baseline fetal heart rate of 20 beats a minute or
more as a red feature in active second stage labour. [2022]
If CTG concerns arise in the active second stage of labour:
• obtain an obstetric review
• consider discouraging pushing and stopping any oxytocin
infusion to allow the baby to recover, unless birth is imminent
• agree and document a clear plan with time limits for the next
review.
11/11/2023 Dr.Zuhair Adam](https://image.slidesharecdn.com/ctginterpretationdrzuhair2023-231111150822-acd8f2c2/85/CTG-INTERPRETATION-Dr-zuhair-2023-pdf-44-320.jpg)