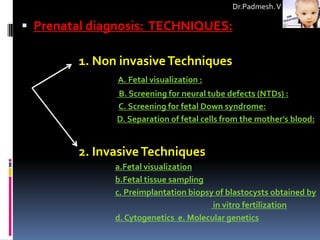
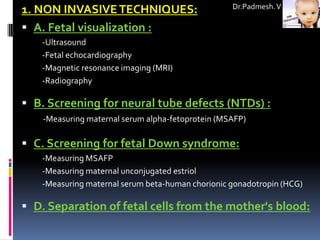
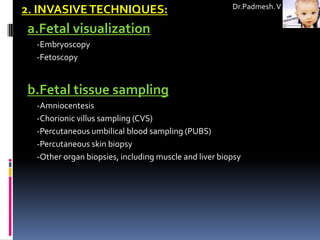
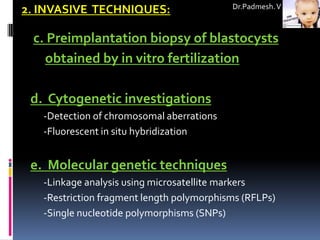
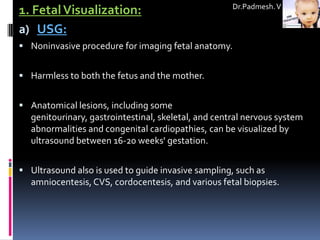
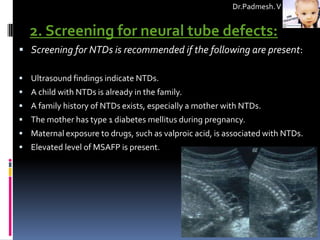
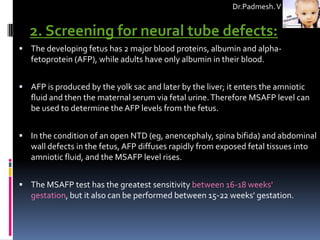
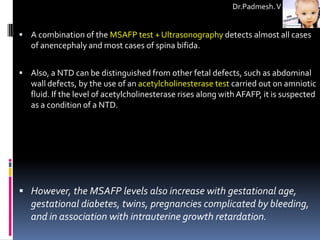
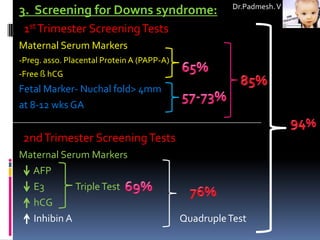
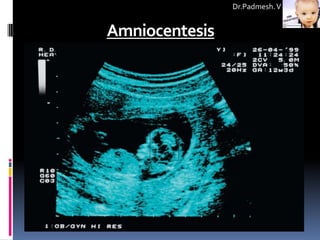
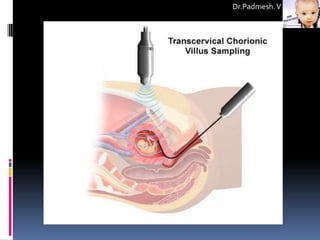
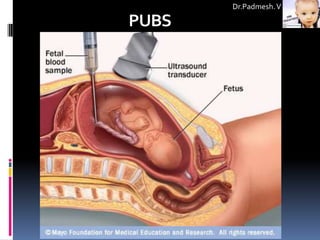
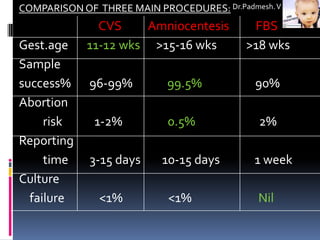
Noninvasive techniques are used for prenatal screening and diagnosis. These include fetal ultrasound imaging to visualize anatomy, measuring maternal serum markers like alpha-fetoprotein to screen for neural tube defects, and separating fetal cells from the mother's bloodstream for genetic analysis. More invasive techniques provide tissue samples through procedures like amniocentesis and chorionic villus sampling for cytogenetic or molecular testing to confirm or diagnose genetic disorders.