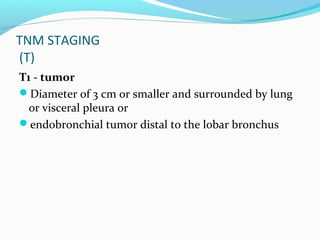
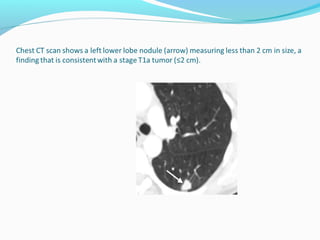
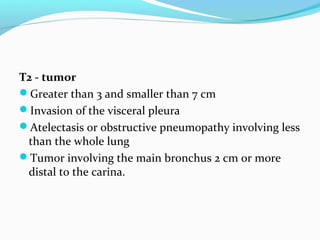
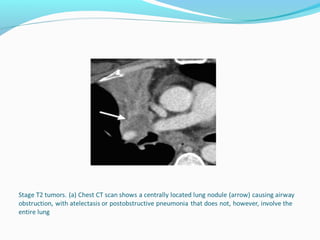
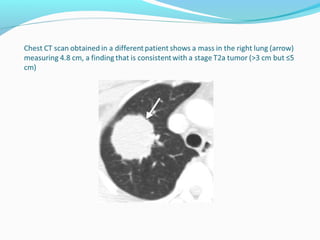
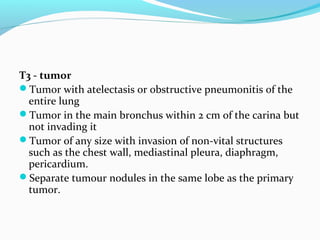
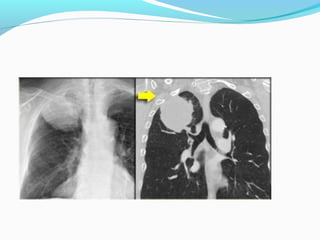
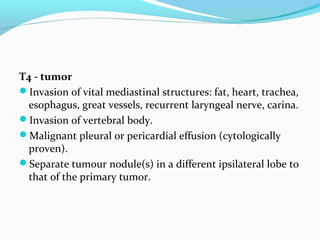
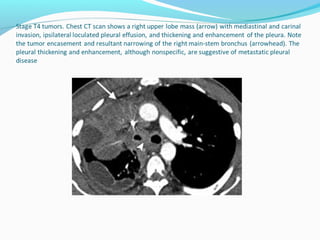
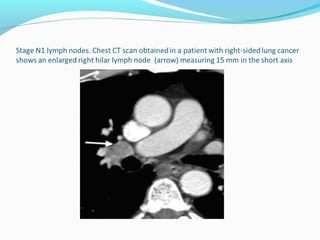
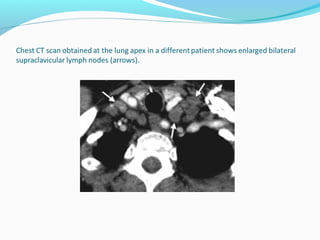
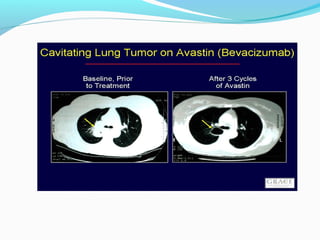
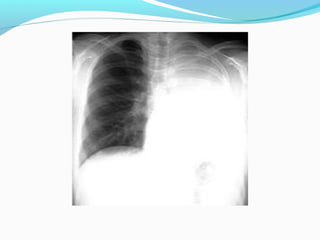
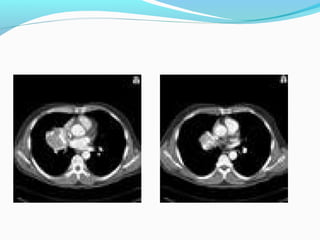
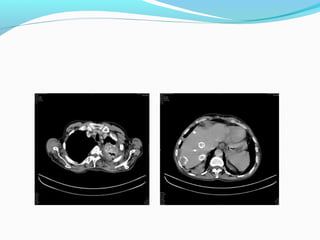
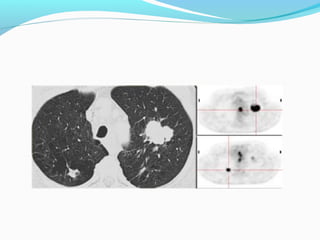
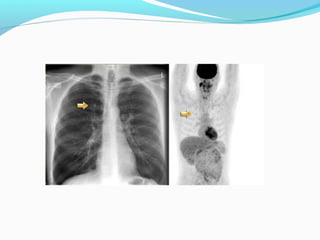
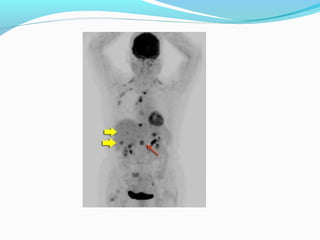
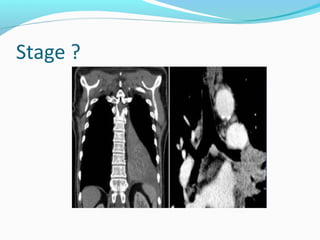
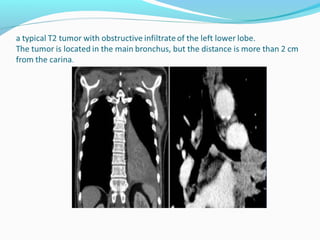
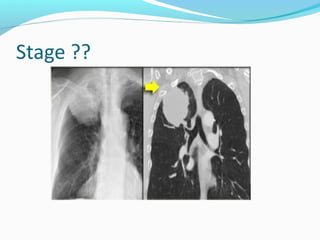
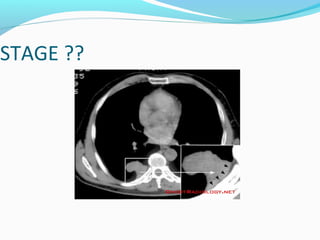
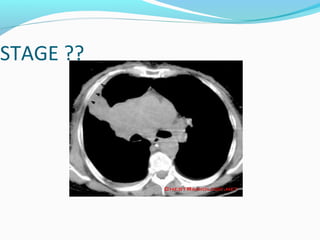
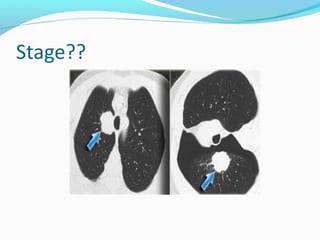
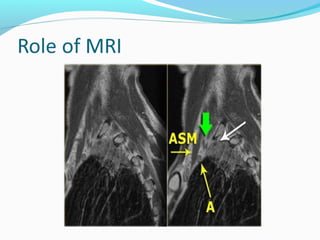
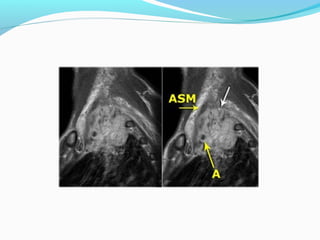
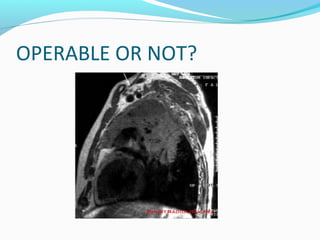
The document discusses the etiology, types, staging, and characteristics of bronchial carcinoma. The main causes are tobacco smoking, asbestos exposure, irradiation, and toxic metals. The four main types are squamous cell carcinoma, adenocarcinoma, small cell carcinoma, and alveolar cell carcinoma. Staging involves assessing the tumor size (T stage), lymph node involvement (N stage), and presence of distant metastasis (M stage). Later sections provide more details on lymph node classification, calcification, FDG uptake, operability in certain cases like Pancoast tumors.