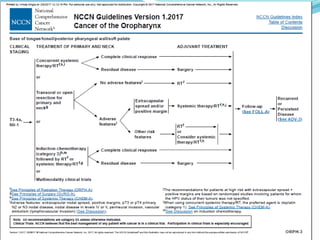
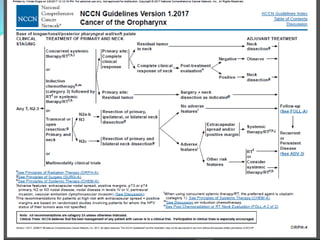
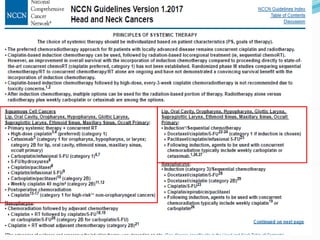
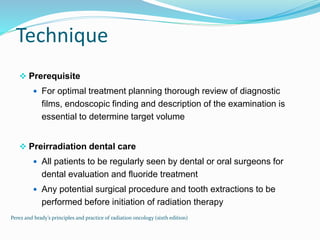
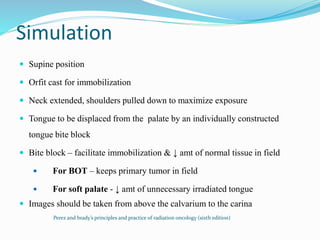
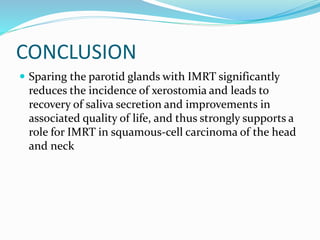
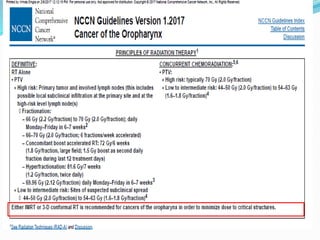
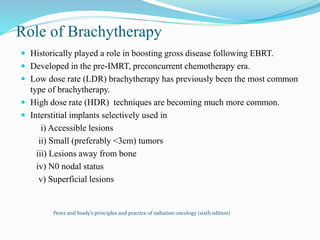
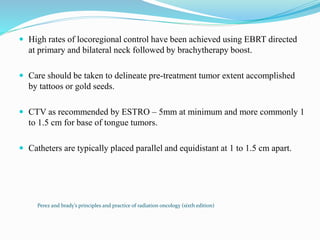
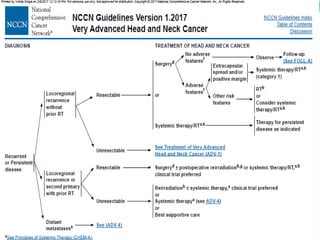
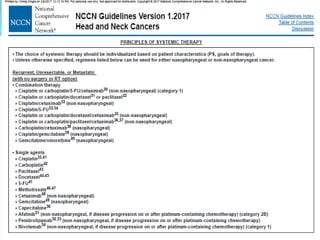
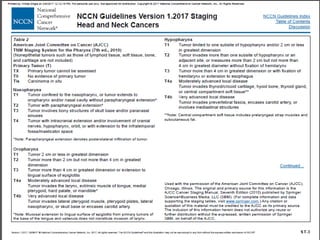
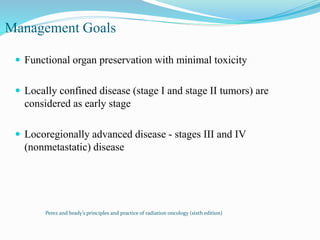
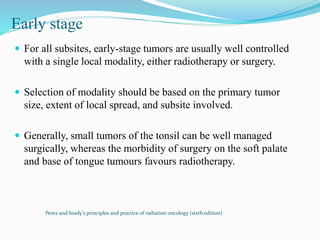
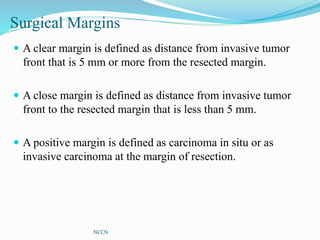
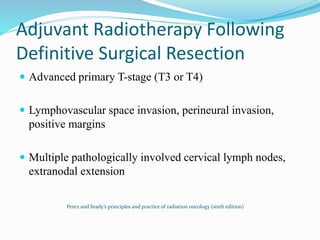
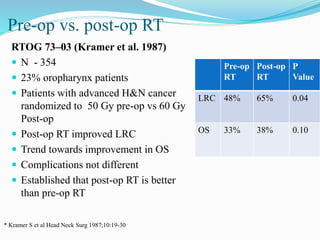
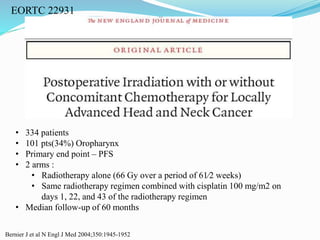
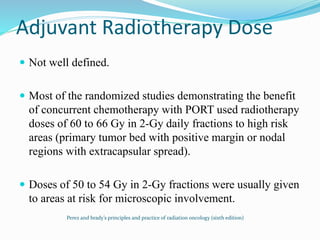
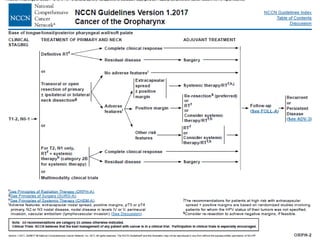
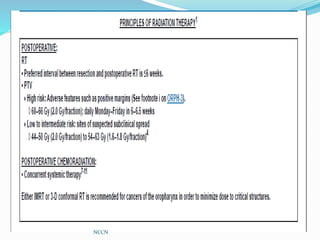
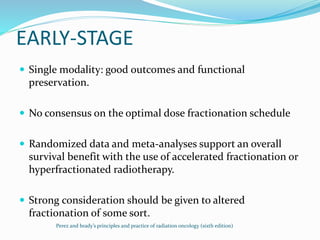
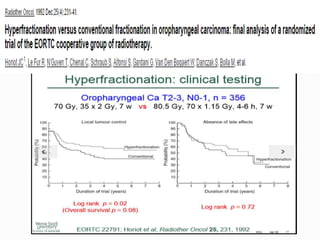
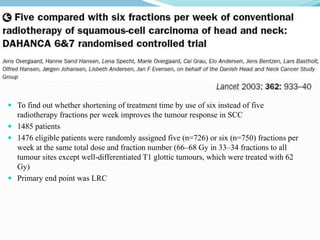
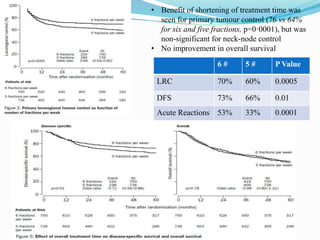
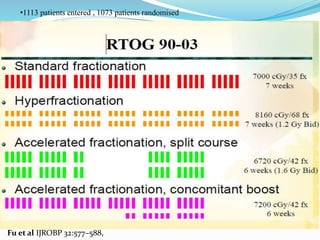
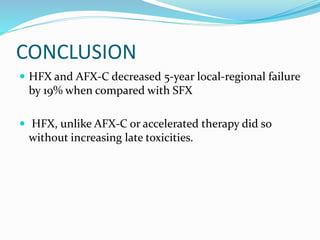
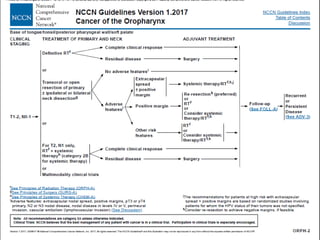
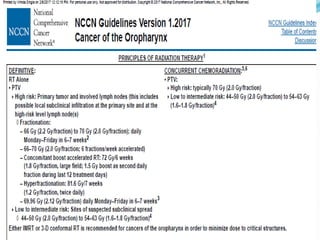
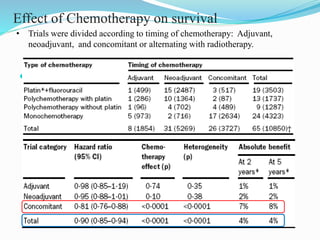
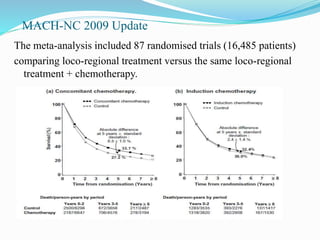
The document discusses management of head and neck cancers, including oropharyngeal cancer. It covers treatment goals, staging, treatment modalities including surgery, radiotherapy and chemotherapy. For early stage disease, single modality treatment with radiotherapy or surgery is usually sufficient. For locally advanced disease, concurrent chemoradiotherapy is the standard. Post-operative chemoradiotherapy may be indicated for patients with high risk features following surgery such as positive margins. Intensity-modulated radiotherapy is now commonly used to reduce toxicity.

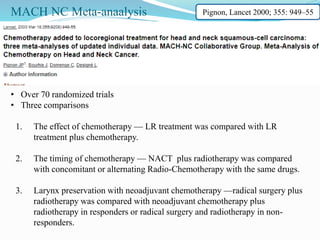
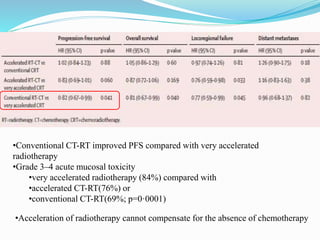
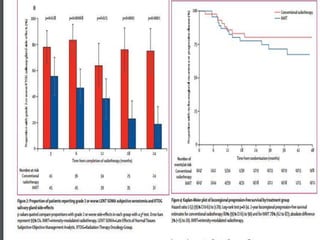
![ Locally advanced head and neck squamous-cell carcinoma
840 patients (66% oropharynx pts)
3 arms
Conventional CT-RT(70 Gy/35# + 3 cycles concomitant carboplatin-fluorouracil)
Accelerated CT-RT(70 Gy in 6 weeks +2 cycles of 5 days concomitant carboplatin-
fluorouracil)
Very accelerated radiotherapy alone (64·8 Gy [1·8 Gy twice daily] in 3·5 weeks)
Median follow-up was 5·2 years
Primary endpoint - PFS](https://image.slidesharecdn.com/newmicrosoftofficepowerpointpresentation-180705085842/85/ca-oropharynx-52-320.jpg)