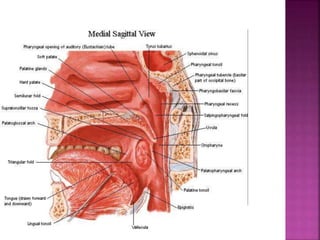
The document discusses the anatomy and functions of the soft palate, including its role in separating the nasopharynx from the oropharynx and in speech, swallowing, and respiratory functions. It then provides statistics on the annual incidence of oral cancer worldwide and risk factors such as tobacco, alcohol, HPV infection, and poor oral hygiene. The stages of oral cancer are described based on tumor size and spread.