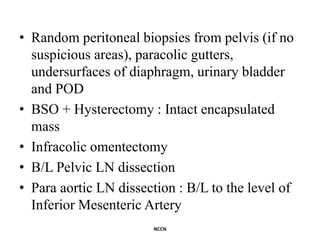
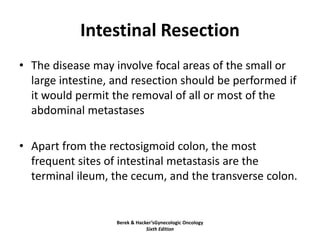
This document discusses the management of ovarian cancer. It covers risk-reducing salpingo-oophorectomy (RRSO) for high-risk patients, surgical staging techniques including open and minimally invasive approaches, management of early-stage disease including adjuvant chemotherapy and radiation, cytoreductive surgery and goals for advanced-stage disease, and the role of interval debulking surgery after neoadjuvant chemotherapy. Complete resection of all tumor is the optimal outcome for advanced ovarian cancer to improve survival outcomes.