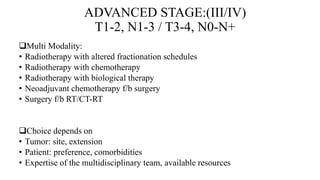
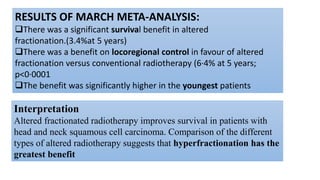
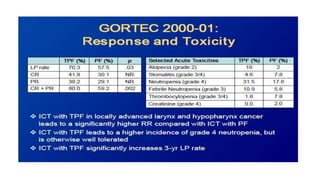
This document summarizes guidelines for the management of carcinoma of the hypopharynx and larynx. It covers topics like NCCN guidelines, treatment options including surgery, radiotherapy, chemotherapy and biological therapy. It describes TNM staging according to AJCC 7th edition and provides general treatment recommendations based on tumor stage. It discusses the benefits of radiotherapy over surgery and indications for primary radiotherapy. It also summarizes various studies comparing altered fractionation radiotherapy with or without chemotherapy to conventional radiotherapy for improved survival outcomes in advanced stage disease.




























































![ Accelerated radiotherapy-chemotherapy offered no PFS benefit compared with conventional
chemoradiotherapy or very accelerated radiotherapy
conventional chemoradiotherapy improved PFS compared with very accelerated chemoradiotherapy
More patients in the very accelerated radiotherapy group had RTOG grade 3-4 acute mucosal
toxicity (226 [84%] of 268 patients) compared with accelerated radiotherapy-chemotherapy (205
[76%] of 271 patients) or conventional chemoradiotherapy (180 [69%] of 262; p=0·0001).
(60%) of patients in the conventional chemoradiotherapy group, (64%) of patients in the
accelerated radiotherapy-chemotherapy group, and (70%) of patients in the very accelerated
radiotherapy group were intubated with feeding tubes during treatment (p=0·045).
Results of GORTEC 9902](https://image.slidesharecdn.com/jqbmjhyqbsx1iuy5ckc1-signature-eaf12d6eca54dc17cb0f861df5438b7d6558073f64c8818c45af2f13932cdafa-poli-180401072641/85/Hypopharynxmanagement-67-320.jpg)