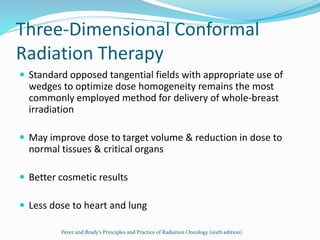
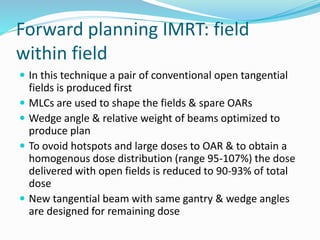
1) The document discusses various techniques for radiation therapy treatment planning and delivery for breast cancer, including tangential field planning, supraclavicular field matching, electron boosts, and accelerated partial breast irradiation.
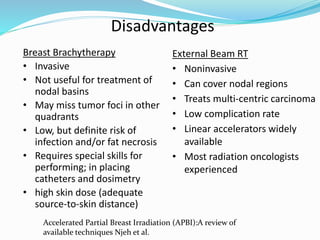
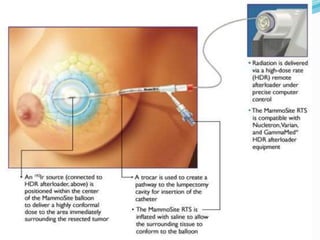
2) Techniques for accelerated partial breast irradiation discussed include multi-catheter interstitial brachytherapy, balloon-based brachytherapy using devices like Mammosite, and external beam radiation therapy.
3) Factors that determine suitability for accelerated partial breast irradiation include patient age, tumor size and characteristics, and nodal involvement. Dosage schedules and advantages and disadvantages of different techniques are also reviewed.



































































![Radiotherapy toxicity was lower in the targeted intraoperative radiotherapy
group (6 patients [0·5%]) than in the external beam radiotherapy group (23
patients [2·1%]; p=0·002).](https://image.slidesharecdn.com/rtbreastapbi-180705090522/85/RT-breast-apbi-74-320.jpg)















