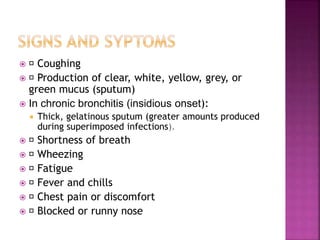
Bronchitis is inflammation of the bronchial tubes caused by viruses, bacteria, or other irritants. It is characterized by coughing and mucus production. Risk factors include smoking, exposure to secondhand smoke, air pollution, and weakened immune systems. Treatment involves antibiotics for bacterial infections, bronchodilators, expectorants, and lifestyle changes like smoking cessation. Nursing care focuses on airway clearance, breathing exercises, hydration, and preventing exacerbations.