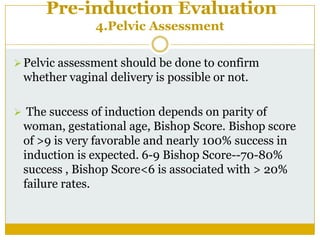
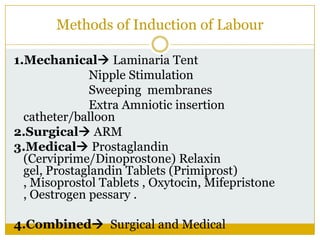
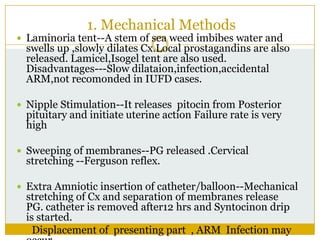
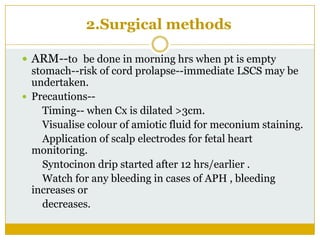
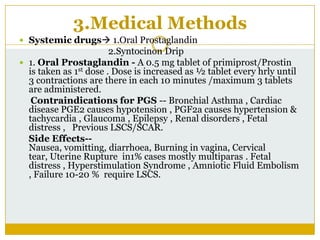
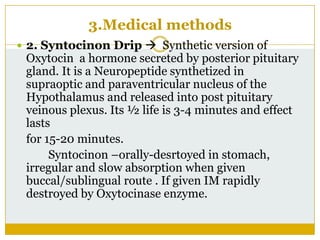
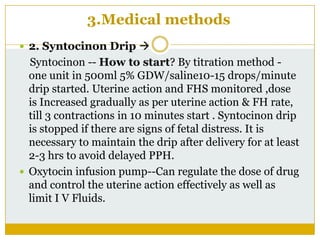
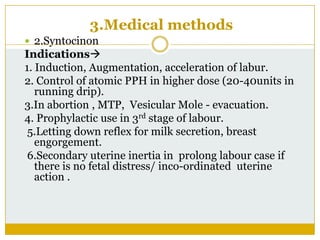
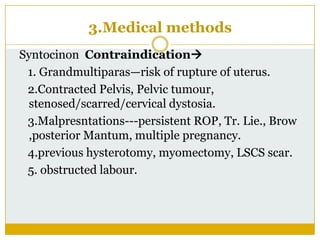
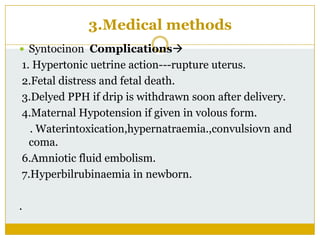
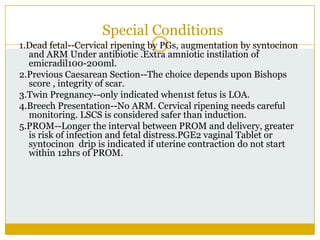
Induction of labour is defined as inducing labour after 28 weeks of gestation but before spontaneous onset of labour, with the aim of vaginal delivery. Common indications for induction include post-term pregnancy, hypertensive disorders, diabetes, and premature rupture of membranes. Methods for induction include mechanical methods like laminaria tents, surgical methods like artificial rupture of membranes, and medical methods using prostaglandins or oxytocin drips.