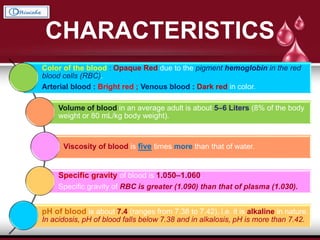
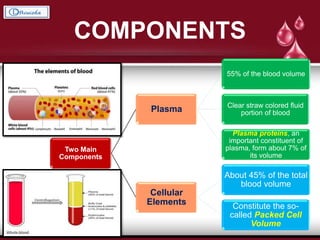
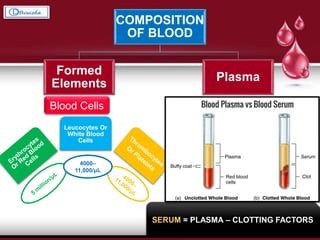
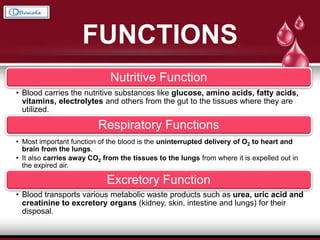
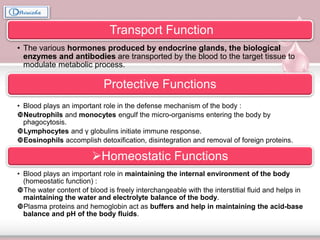
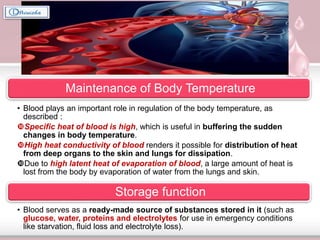
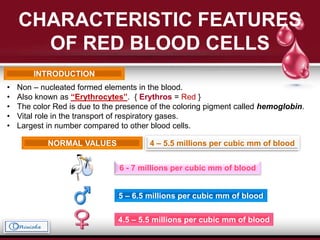
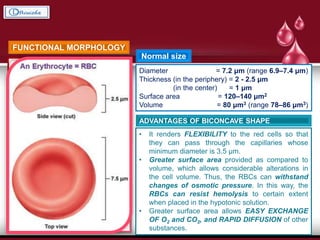
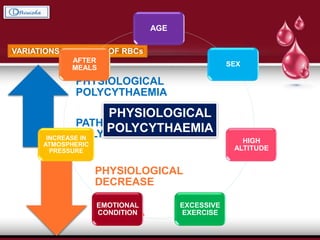
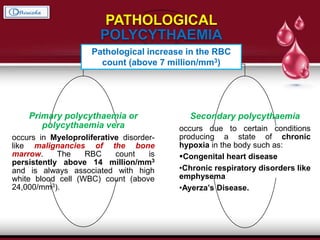
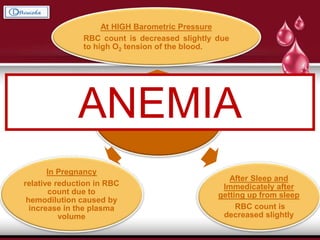
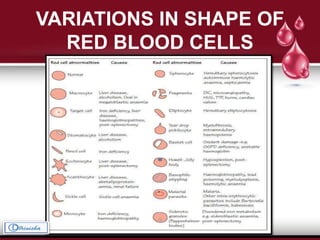
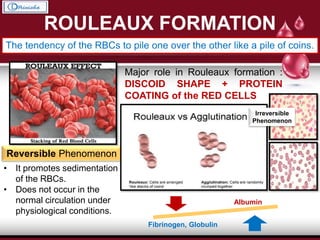
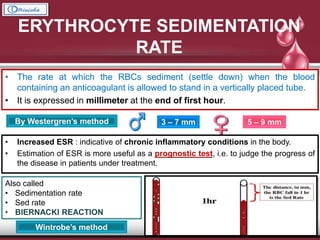
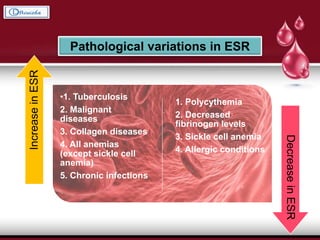
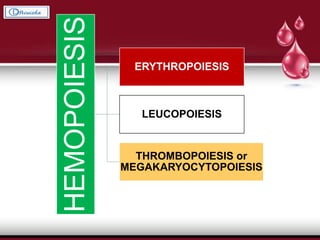
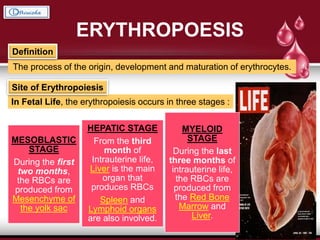
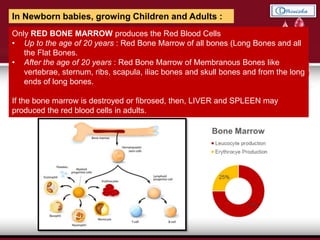
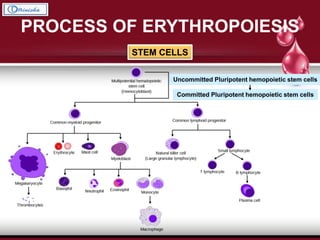
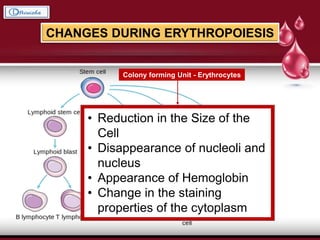
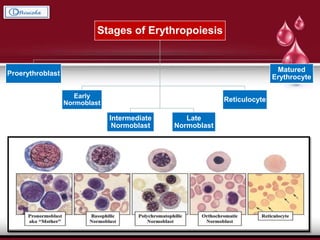
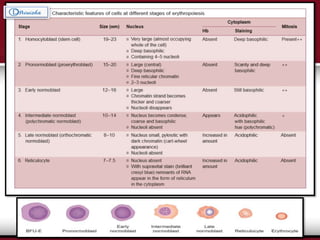
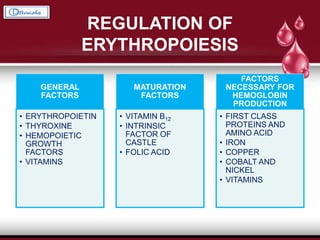
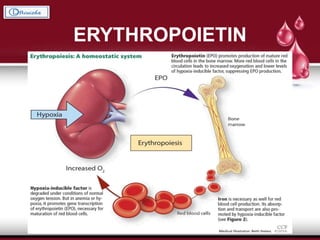
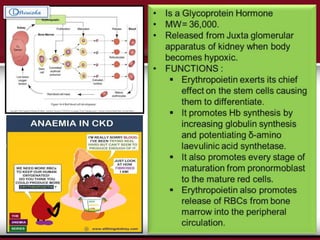
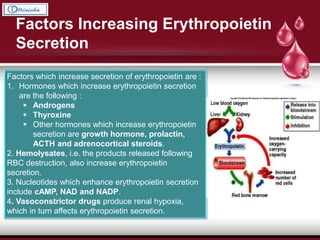
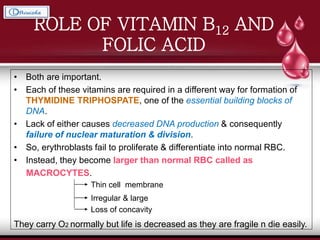
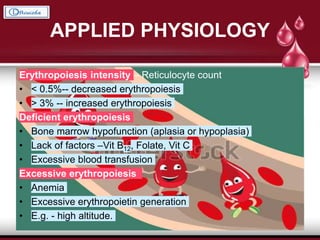
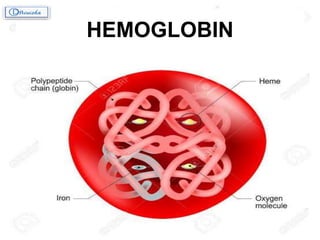
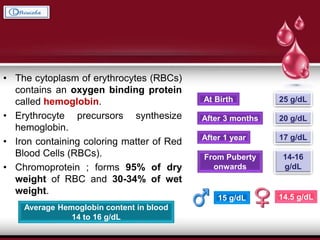
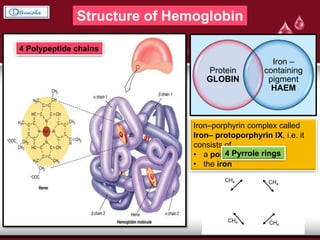
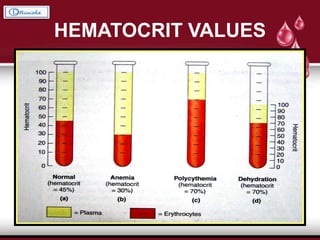
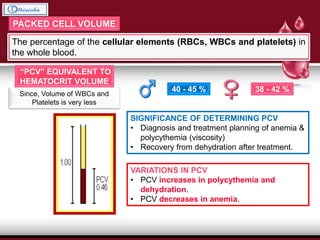
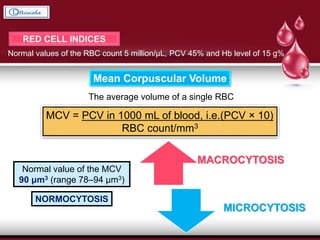
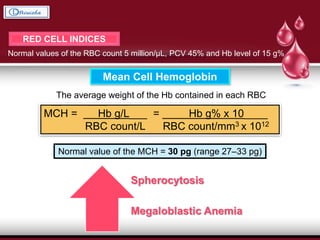
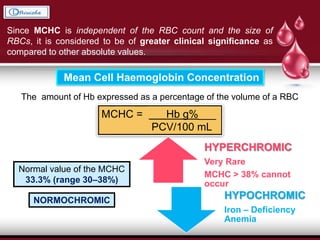
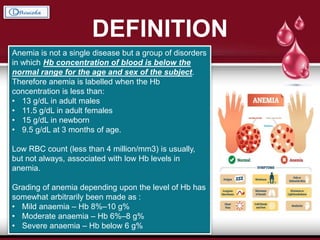
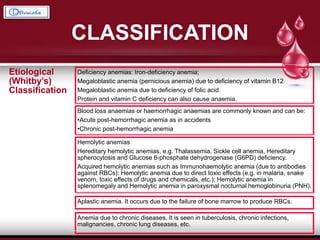
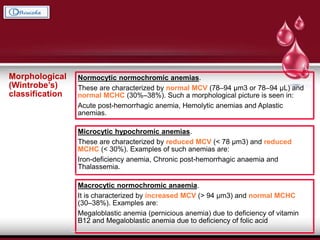
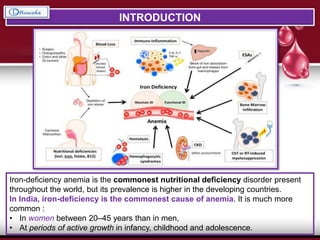
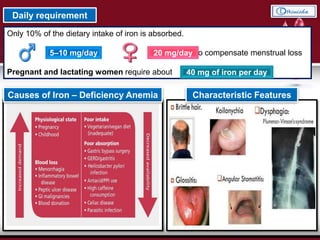
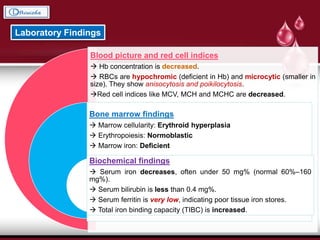
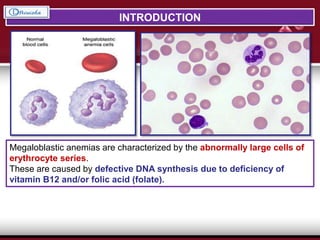
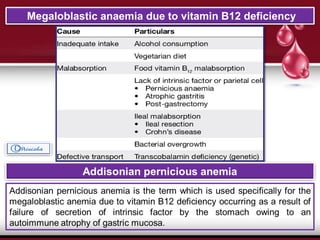
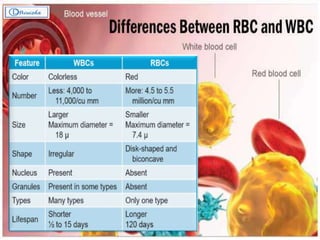
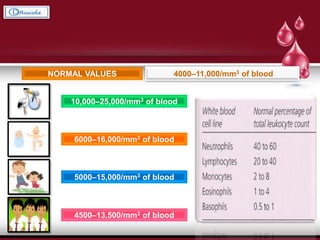
This document provides an overview of blood and its components. It discusses the characteristics of blood, including its color, volume, viscosity, and pH. It describes the two main components of blood: plasma and cellular elements. It then covers the functions of blood in nutrition, respiration, excretion, transport, protection, and homeostasis. Specific components of blood like red blood cells, hemoglobin, hematocrit values, and anemia are explained in detail. The process of erythropoiesis and factors regulating it are also summarized.