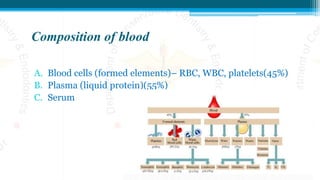
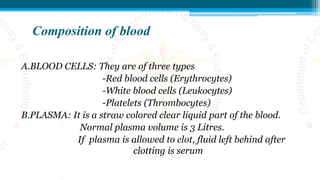
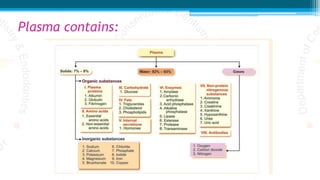
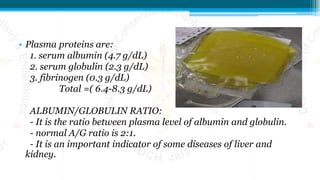
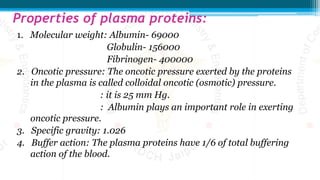
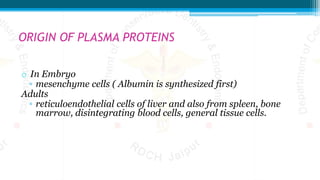
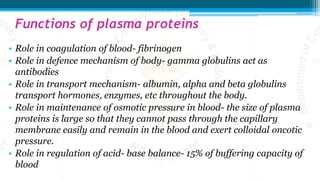
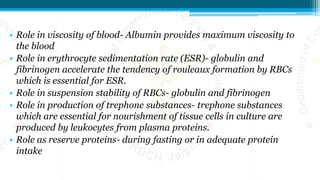
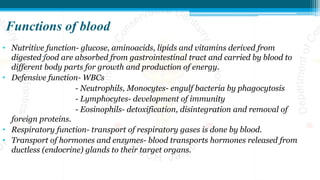
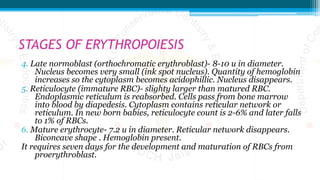
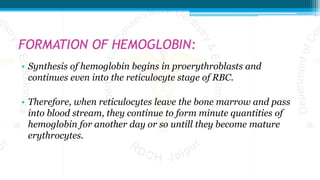
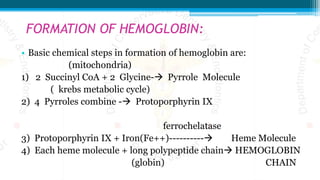
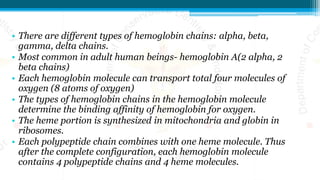
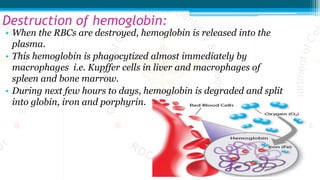
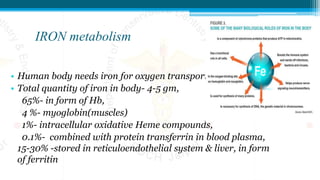
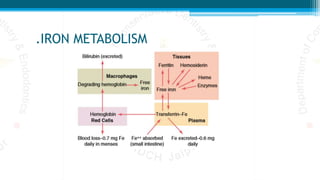
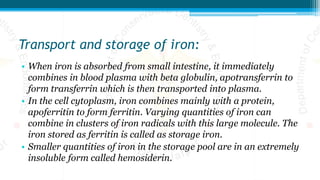
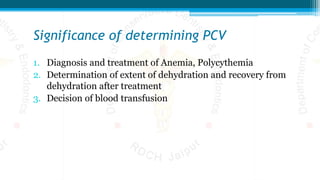
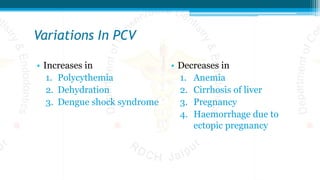
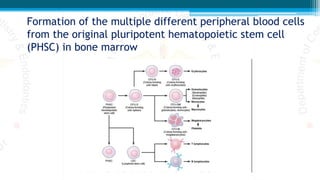
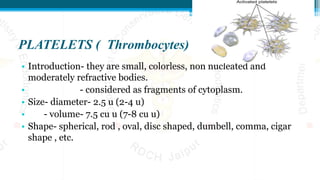
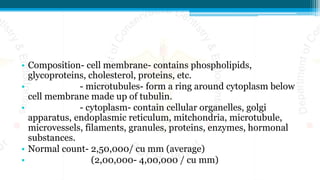
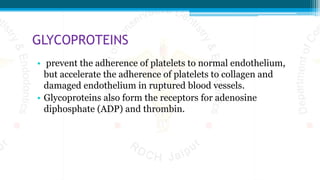
The document is a comprehensive overview of blood, detailing its properties, composition, and crucial functions, such as transporting oxygen, nutrients, and waste products. It elaborates on the genesis of blood cells, specifically erythropoiesis, and includes information on hemoglobin and iron metabolism, as well as various blood disorders like anemia and leukemia. Additionally, it covers the roles of plasma proteins and the physiological variations in blood components.

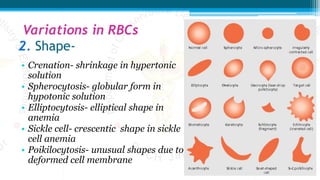


![• 1] sickle cell anemia:
• Sickle cell anemia is an inherited blood disorder
• characterized by sickleshaped red blood cells.
• It is also called hemoglobin SS disease or sickle cell disease.
• It is common in people of African origin.
• Sickle cell anemia is due to the abnormal hemoglobin called
hemoglobin S (sickle cell hemoglobin). In this, αchains are normal
and βchains are abnormal.
•](https://image.slidesharecdn.com/blood-200909103922/85/Blood-136-320.jpg)
![• 2] hereditary spherocytosis:
• the red cells are very small and spherical rather than being
biconcave discs.
• These cells cannot withstand compression forces because they do
not have the normal loose,baglike cell membrane structure of the
biconcave discs.
• On passing through the splenic pulp and some other tight vascular
beds, they are easily ruptured by even slight compression.](https://image.slidesharecdn.com/blood-200909103922/85/Blood-138-320.jpg)
![• 3] thalassemia:
• Thalassemia is an inherited disorder,
• characterized by abnormal hemoglobin.
• It is also known as Cooley’s anemia or Mediterranean anemia.
• It is more common in Thailand and to some extent in
Mediterranean countries.
• Thalassemia is of two types:
• i. αthalassemia
• ii. βthalassemia.](https://image.slidesharecdn.com/blood-200909103922/85/Blood-139-320.jpg)