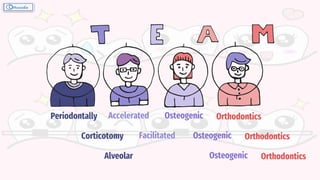
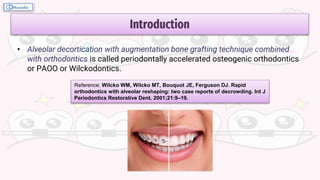
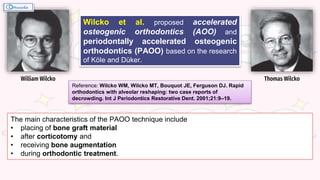
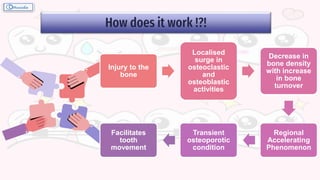
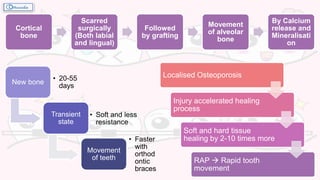
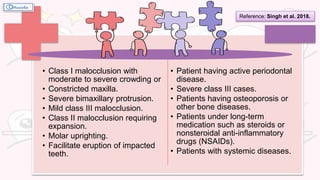
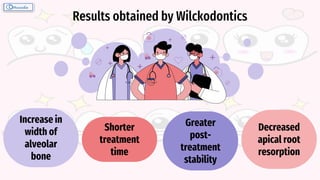
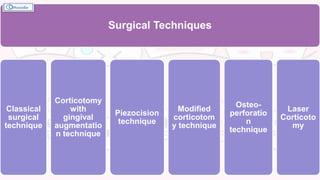
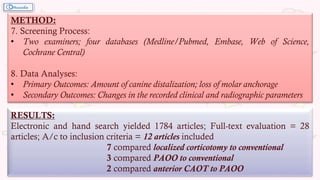
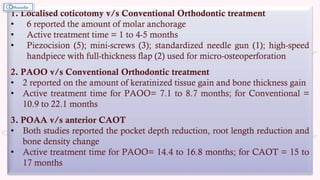
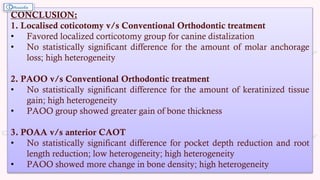
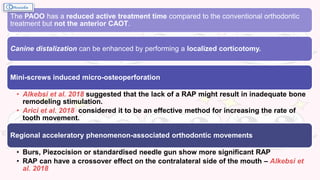
This document summarizes the key aspects and findings of a systematic review and meta-analysis comparing the clinical and radiographic outcomes of orthodontic treatment with corticotomy procedures (localized corticotomy, anterior corticotomy-assisted orthodontic treatment (CAOT), and periodontally accelerated osteogenic orthodontics (PAOO)) versus conventional orthodontic treatment. The review found that localized corticotomy may enhance canine distalization compared to conventional treatment, and that PAOO results in reduced active treatment time and greater alveolar bone thickness gain compared to conventional treatment. However, it also noted high heterogeneity across the included studies and a need for more well-standardized randomized controlled trials to draw definitive conclusions.