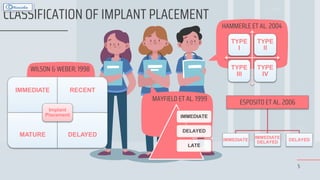
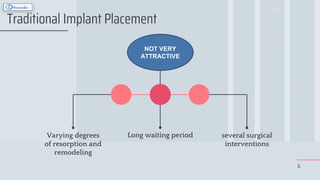
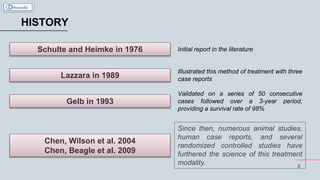
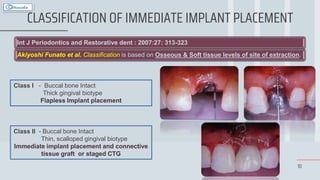
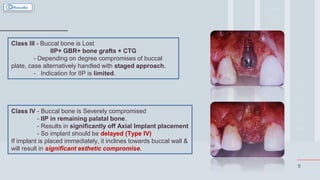
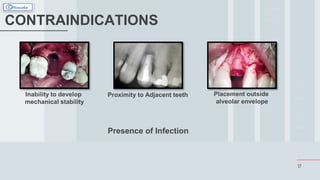
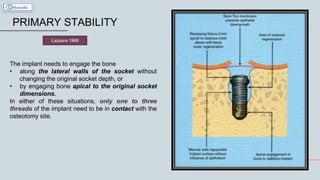
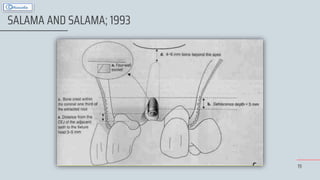
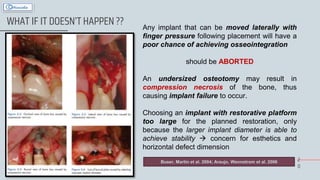
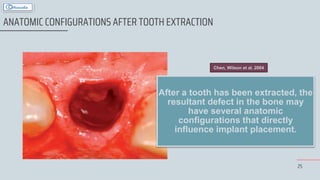
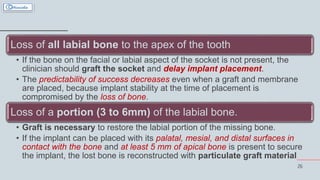
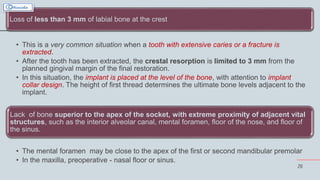
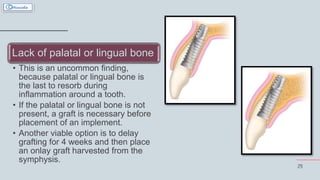
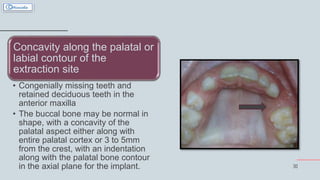
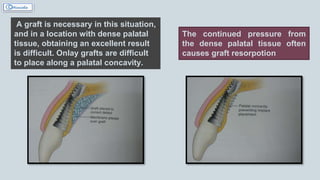
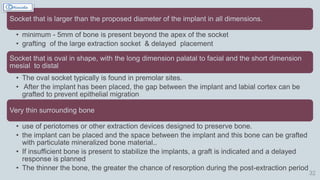
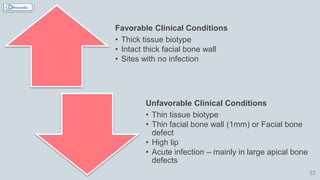
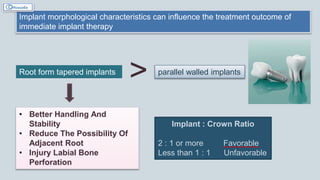
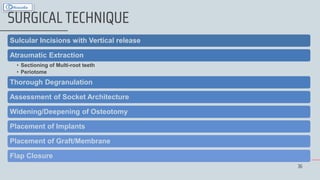
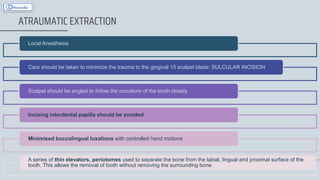
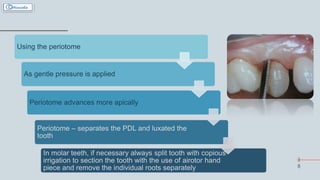
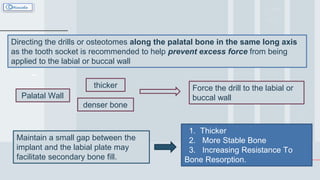
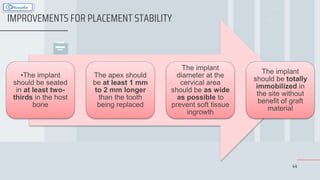
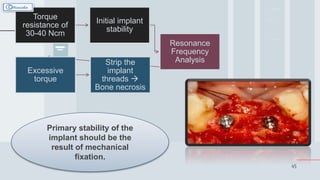
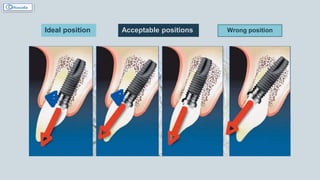
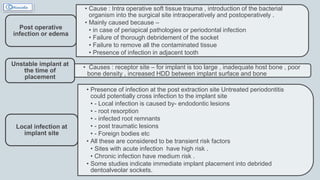
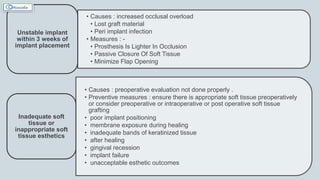
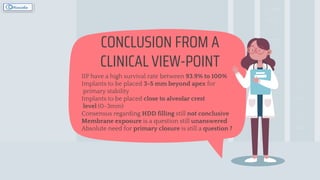
Immediate implant placement involves placing a dental implant immediately following tooth extraction to preserve alveolar bone and reduce treatment time. While traditional protocols recommend 6-12 months of healing before implant placement, immediate placement has been shown to successfully integrate implants when primary stability is achieved. Factors such as infection risk, soft and hard tissue deficiencies, implant positioning, and technique sensitivity must be considered. Studies support immediate placement outcomes when protocols are followed, though buccal bone resorption may still occur depending on initial bone levels. Careful patient evaluation and clinical requirements are needed for success.