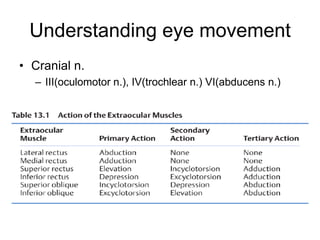
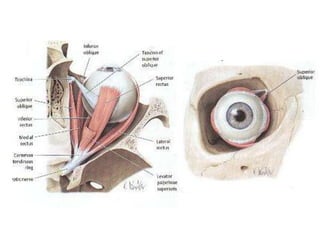
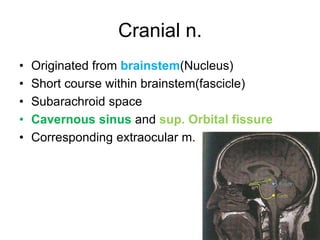
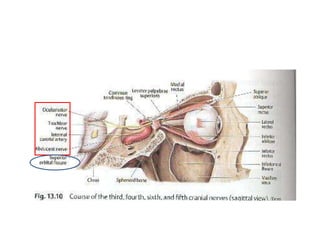
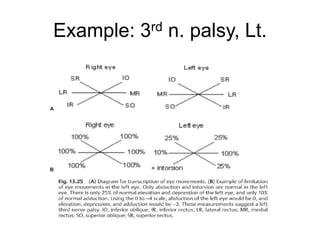
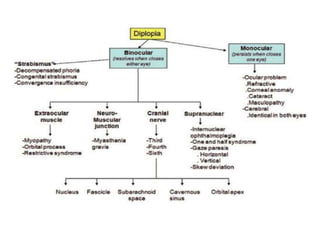
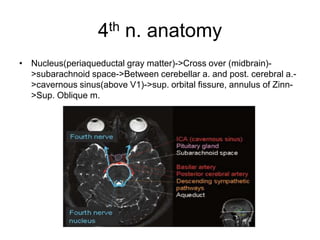
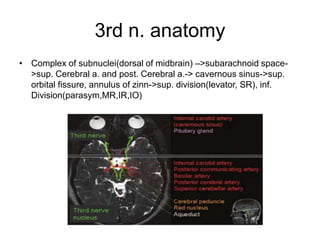
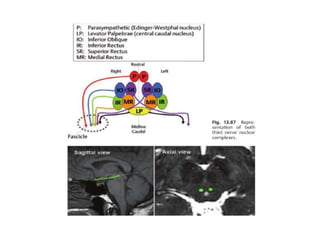
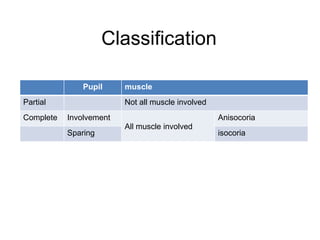
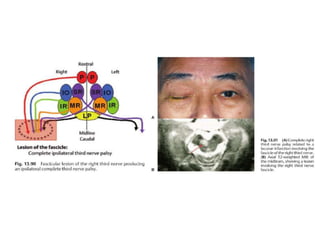
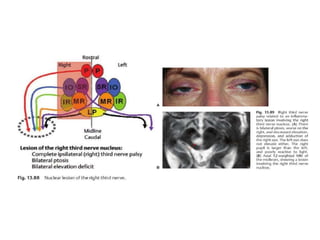
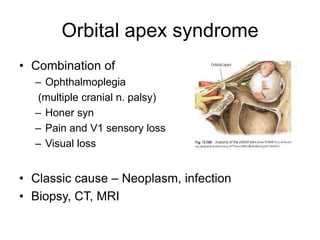
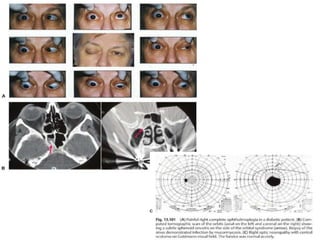
1) Cranial nerves III, IV, and VI are involved in eye movement control. A lesion in these cranial nerves can cause abnormalities like ophthalmoplegia or diplopia.
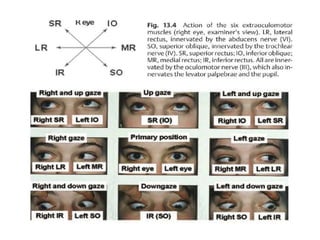
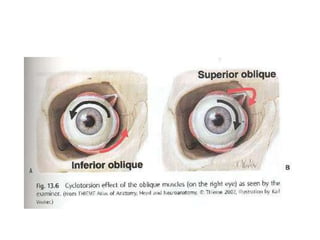
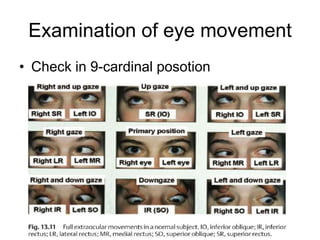
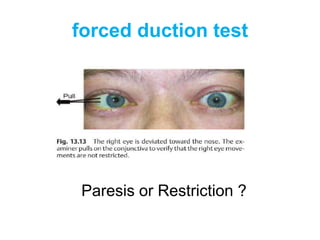
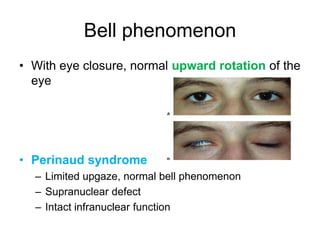
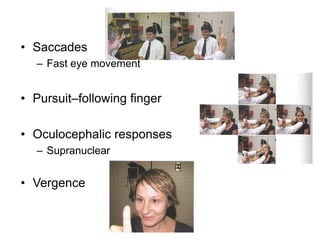
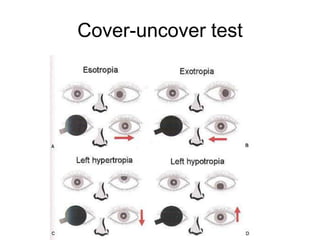
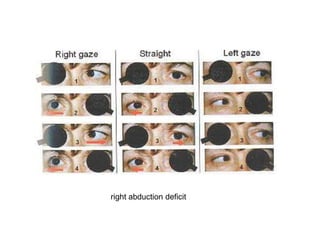
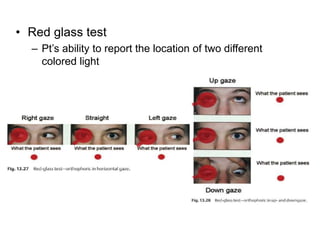
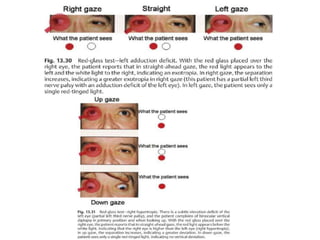
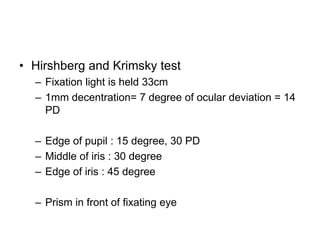
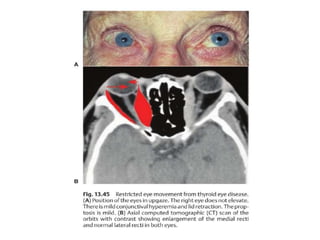
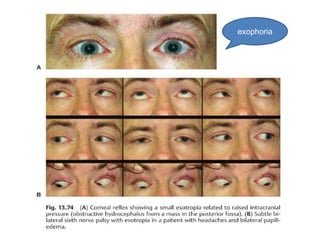
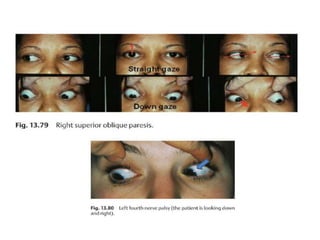
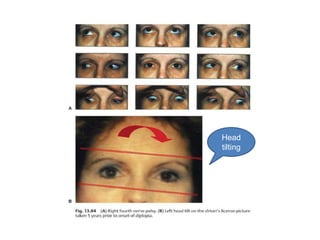
2) Examination of eye movements includes testing in 9 cardinal positions as well as tests like cover-uncover, forced duction, and versions to localize the lesion.
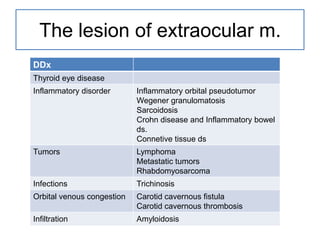
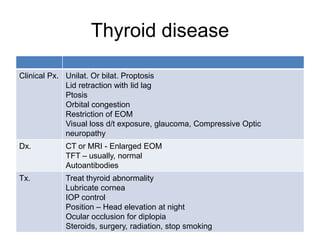
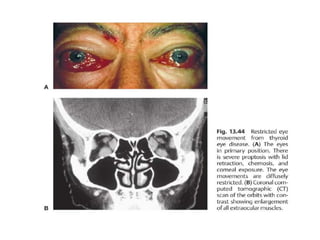
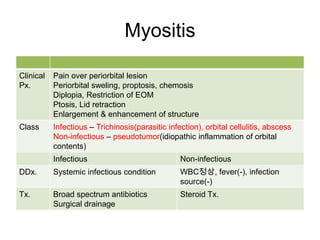
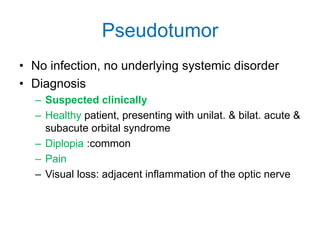
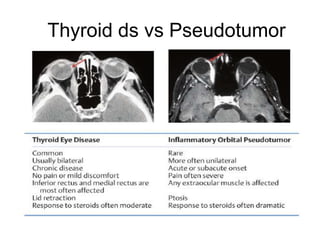
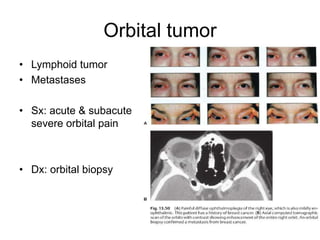
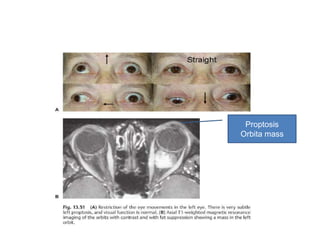
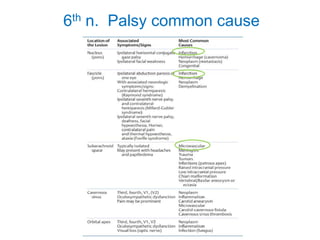
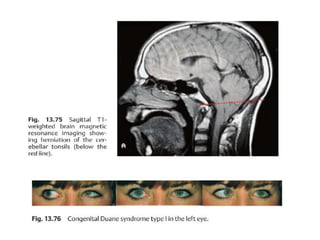
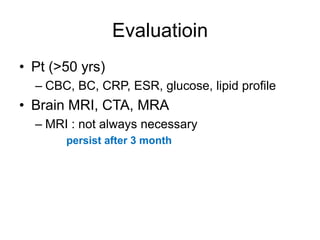
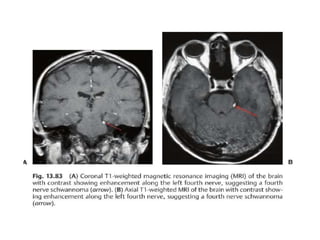
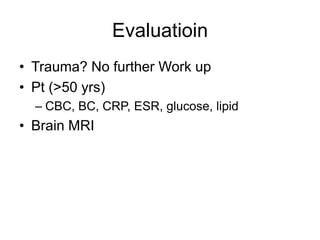
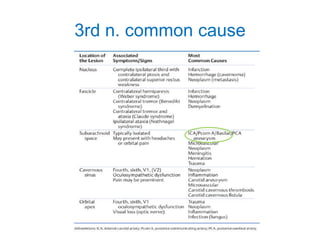
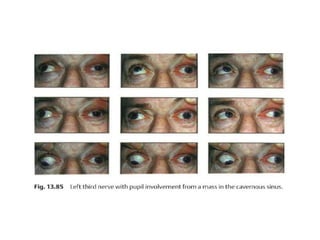
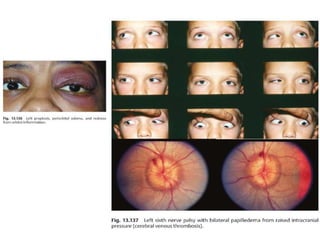
3) Common causes of eye movement abnormalities include thyroid eye disease, orbital pseudotumor, orbital tumors, and cranial nerve palsies. Accurate diagnosis relies on clinical history and examination findings.