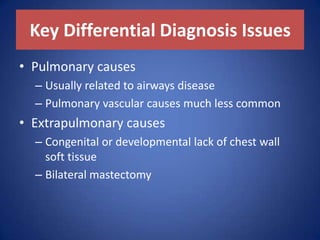
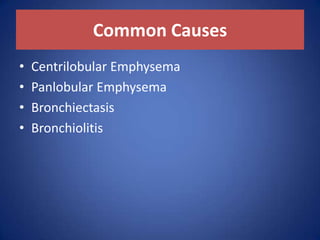
The document outlines key differential diagnoses for bilateral hyperlucent hemithorax, emphasizing both pulmonary and extrapulmonary causes, along with technical considerations. It details common conditions like centrilobular and panlobular emphysema, bronchiectasis, and bronchiolitis, while also addressing less common and rare conditions such as constrictive bronchiolitis and pulmonary atresia. Diagnostic imaging characteristics are provided for various conditions to aid in accurate identification.









![Panlobular Emphysema
– Most commonly associated with α-1-antitrypsin
deficiency
– Rarely associated with intravenous drug abuse
(e.g., methylphenidate [Ritalin])
– Predominates in basal portions of lungs](https://image.slidesharecdn.com/bilateralhyperlucenthemithorax-180125201217/85/Bilateral-hyperlucent-hemithorax-12-320.jpg)






























