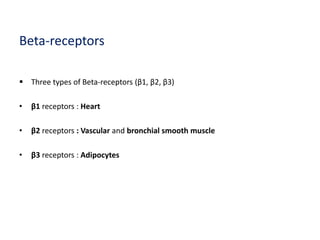
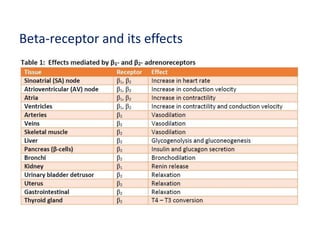
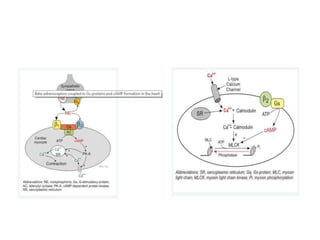
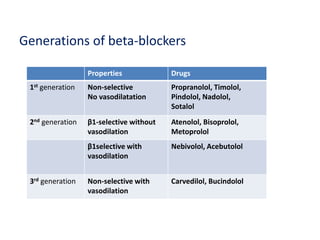
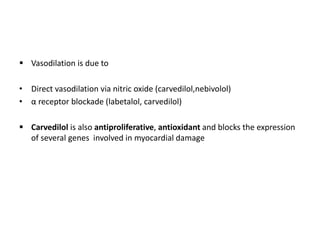
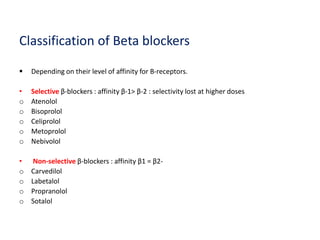
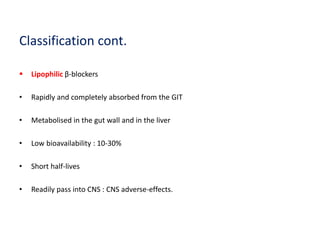
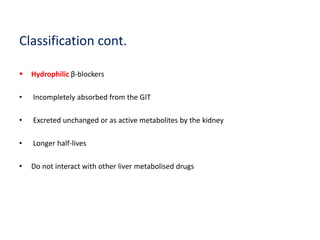
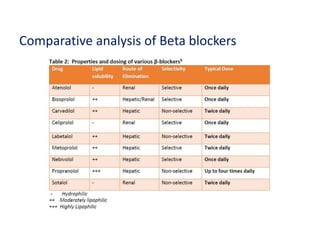
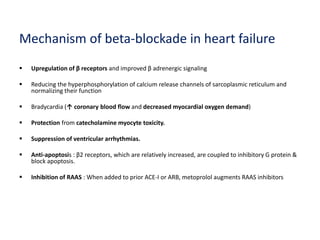
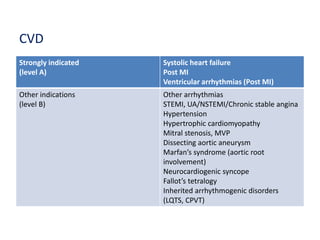
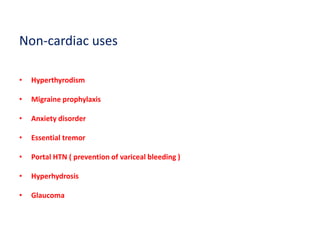
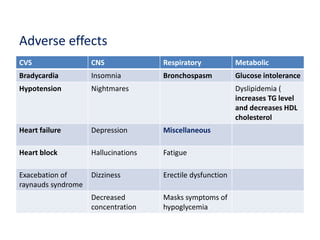
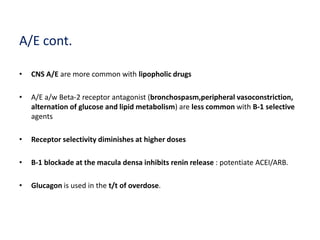
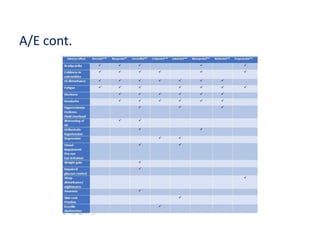
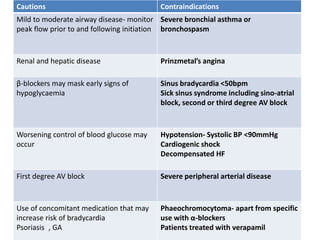
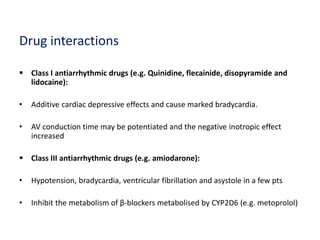
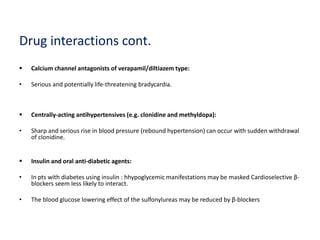
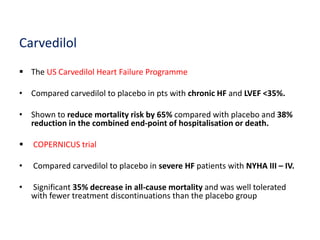
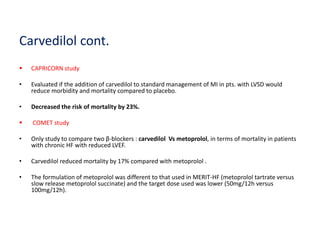
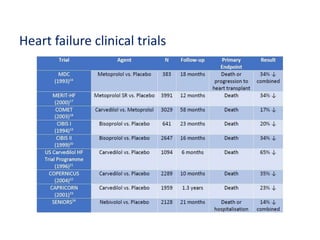
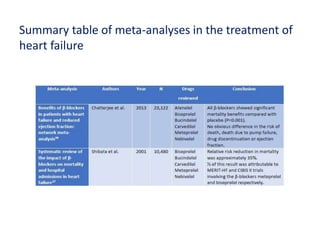
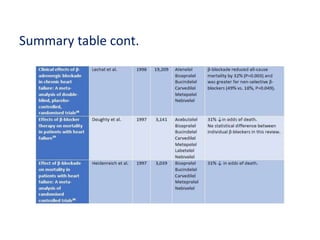
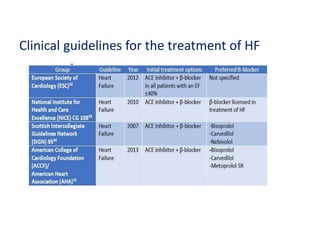
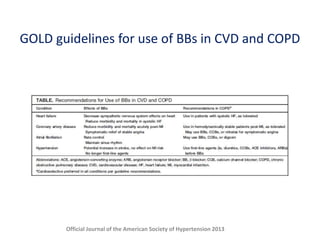
The document provides an extensive overview of beta blockers, emphasizing their classifications, mechanisms, and uses in treating heart failure and cardiovascular diseases. It discusses different generations of beta blockers, their effects on heart receptors, and highlights the significance of beta blockers like metoprolol, bisoprolol, and carvedilol in reducing mortality and improving heart function. It also addresses controversies regarding their use in patients with comorbid conditions such as COPD and outlines cautions, contraindications, and potential drug interactions associated with beta blocker therapy.