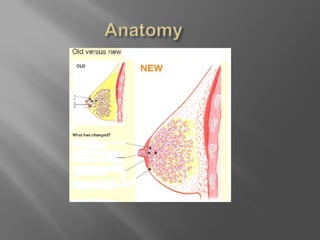
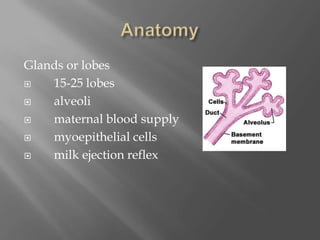
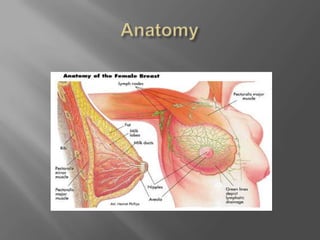
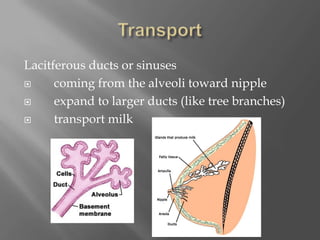
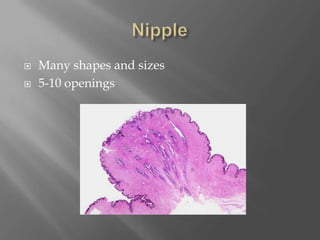
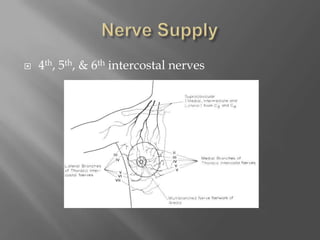
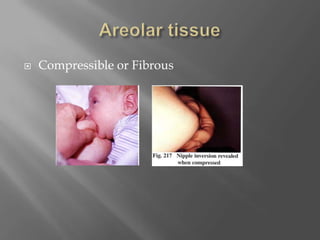
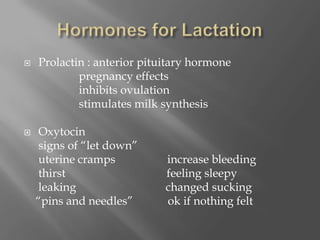
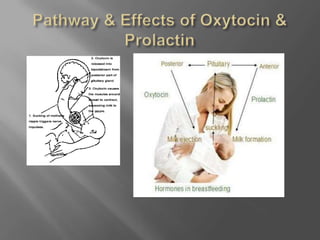
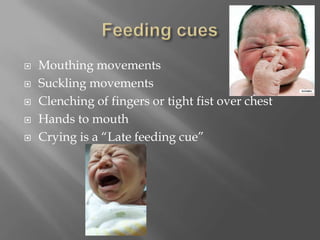
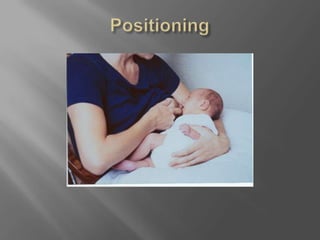
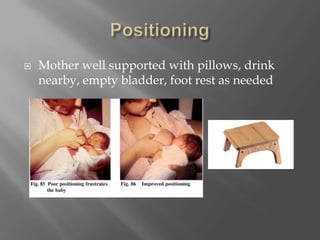
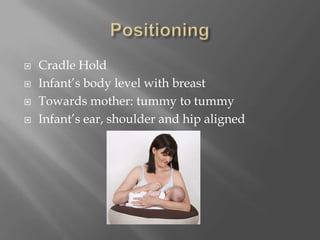
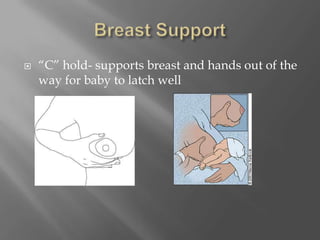
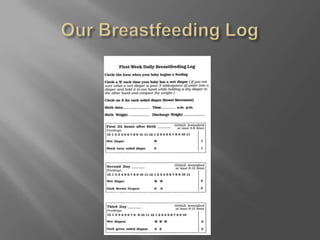
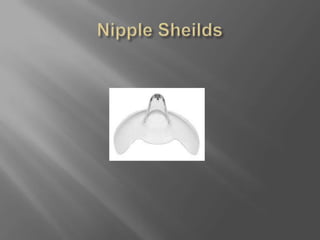
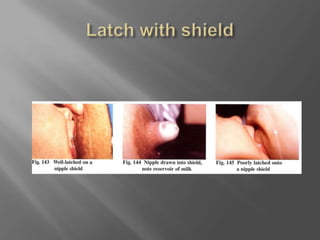
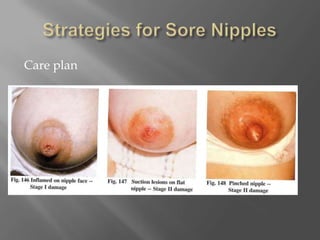
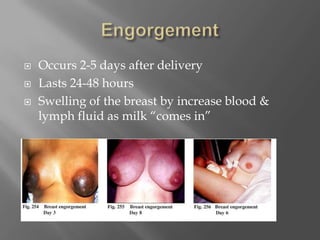
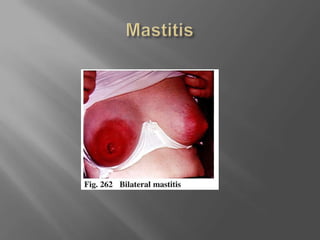
This document provides information on breastfeeding basics including breast anatomy, milk production, positioning and latching, common issues, and benefits. It describes the lobes, ducts, areola, and hormones involved in lactation. Milk composition changes from colostrum to mature milk. Optimal positioning supports the baby's mouth on the breast and lower jaw. Common issues like engorgement, plugged ducts, and mastitis are explained with treatment plans. The document emphasizes the nutritional, developmental and health benefits of breastfeeding for both mother and baby.