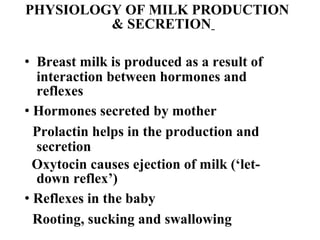
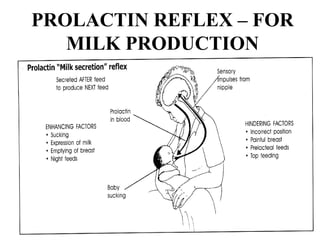
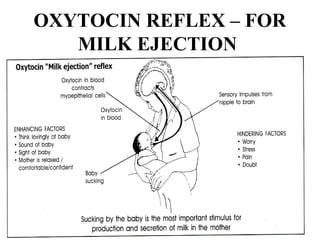
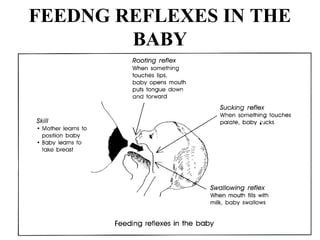
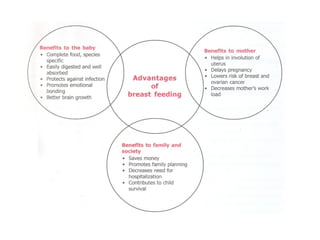
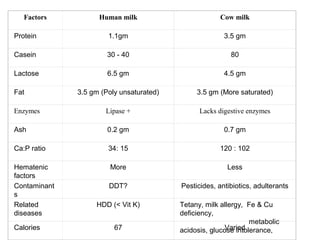
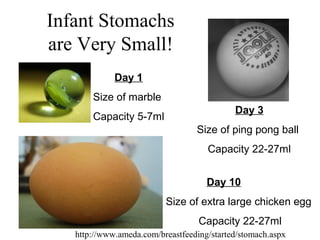
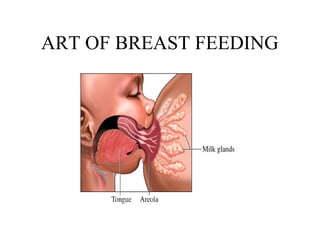
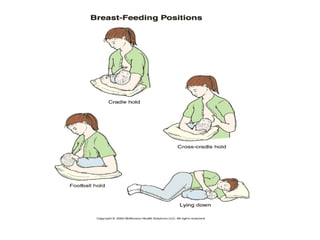
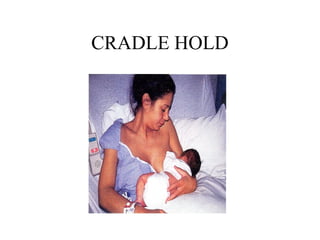
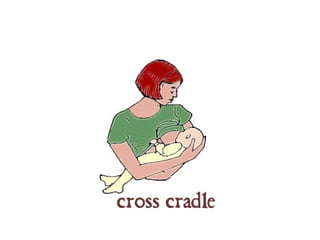
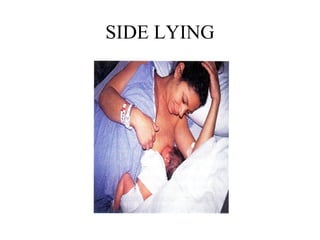
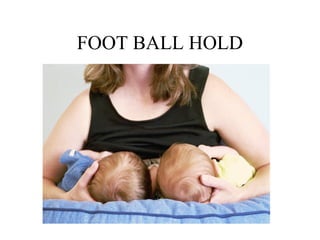
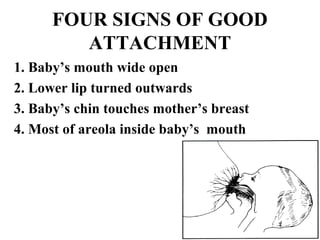
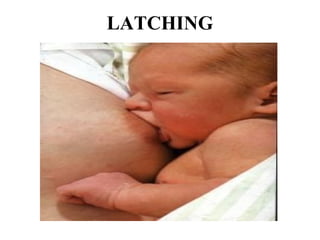
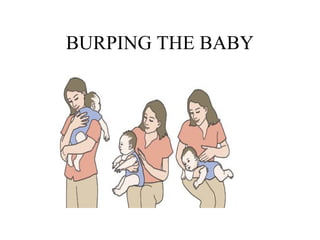
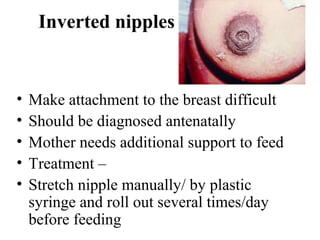
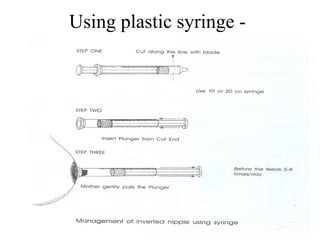
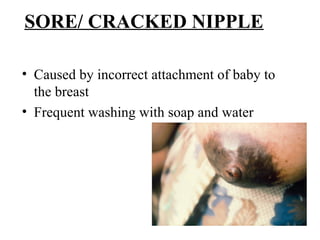
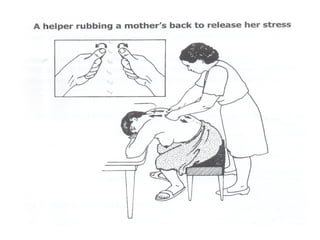
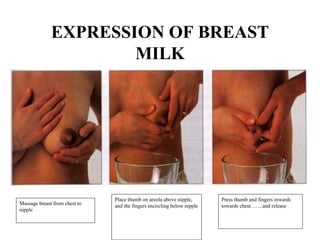
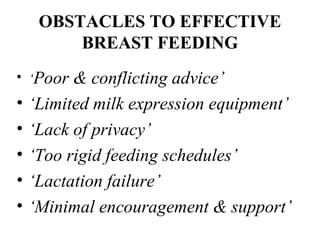
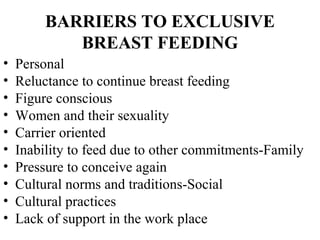
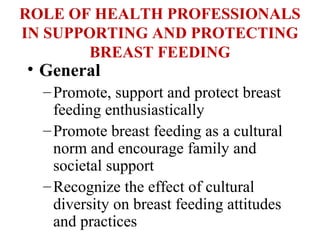
Breastfeeding provides complete nutrition for infants and is the physiologic norm. Breast milk is produced through interactions between hormones like prolactin and oxytocin, and infant feeding reflexes. It contains antibodies and factors that protect against infection. Proper positioning and latch are important for breastfeeding success. Common issues include engorgement, sore nipples, and perceived low milk supply, which can often be addressed by ensuring frequent, proper feeding. Health professionals should promote, educate, and support breastfeeding through clinical practices, encouraging policies, and community outreach.