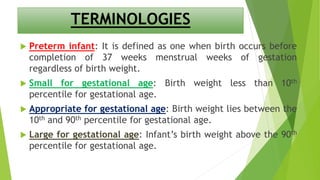
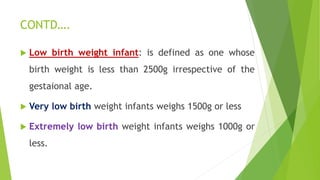
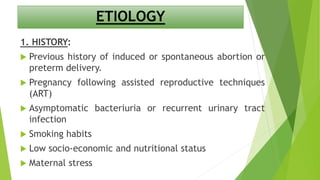
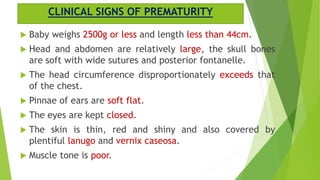
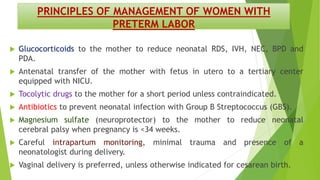
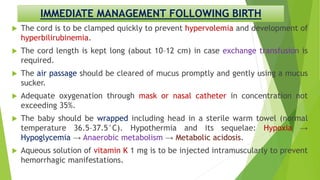
The document provides an overview of pre-term, small for gestational age, and post-mature infants, including definitions, causes, complications, and management strategies. It covers the risk factors and clinical signs of prematurity, as well as intensive care protocols for management and treatment of these infants. Additionally, it discusses complications associated with premature birth, such as respiratory distress syndrome and intraventricular hemorrhage.