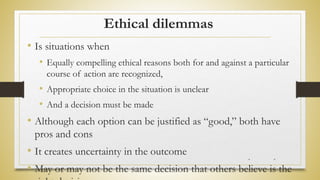
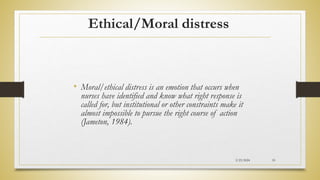
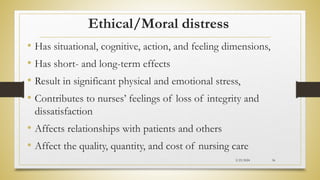
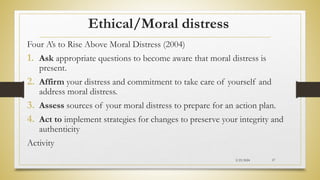
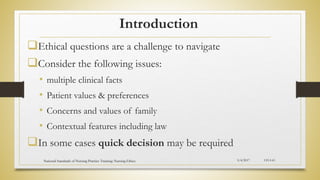
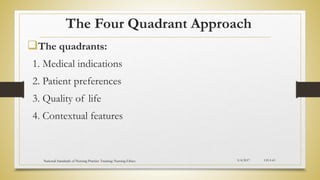
The document outlines an agenda for a national training on nursing ethics conducted by the Federal Ministry of Health. The 7-session training covers topics such as the introduction to nursing ethics, ethical principles, nursing values, ethical dilemmas, ethical decision-making, legal aspects of nursing practice, and the nursing code of ethics. Session 1 defines nursing ethics and describes theories of ethics. Session 2 identifies ethical principles like beneficence, non-maleficence, respect for autonomy, and others. Session 3 explains ideal nursing competencies such as moral integrity, communication skills, and concern for patients. Session 4 discusses ethical dilemmas and moral distress in nursing.