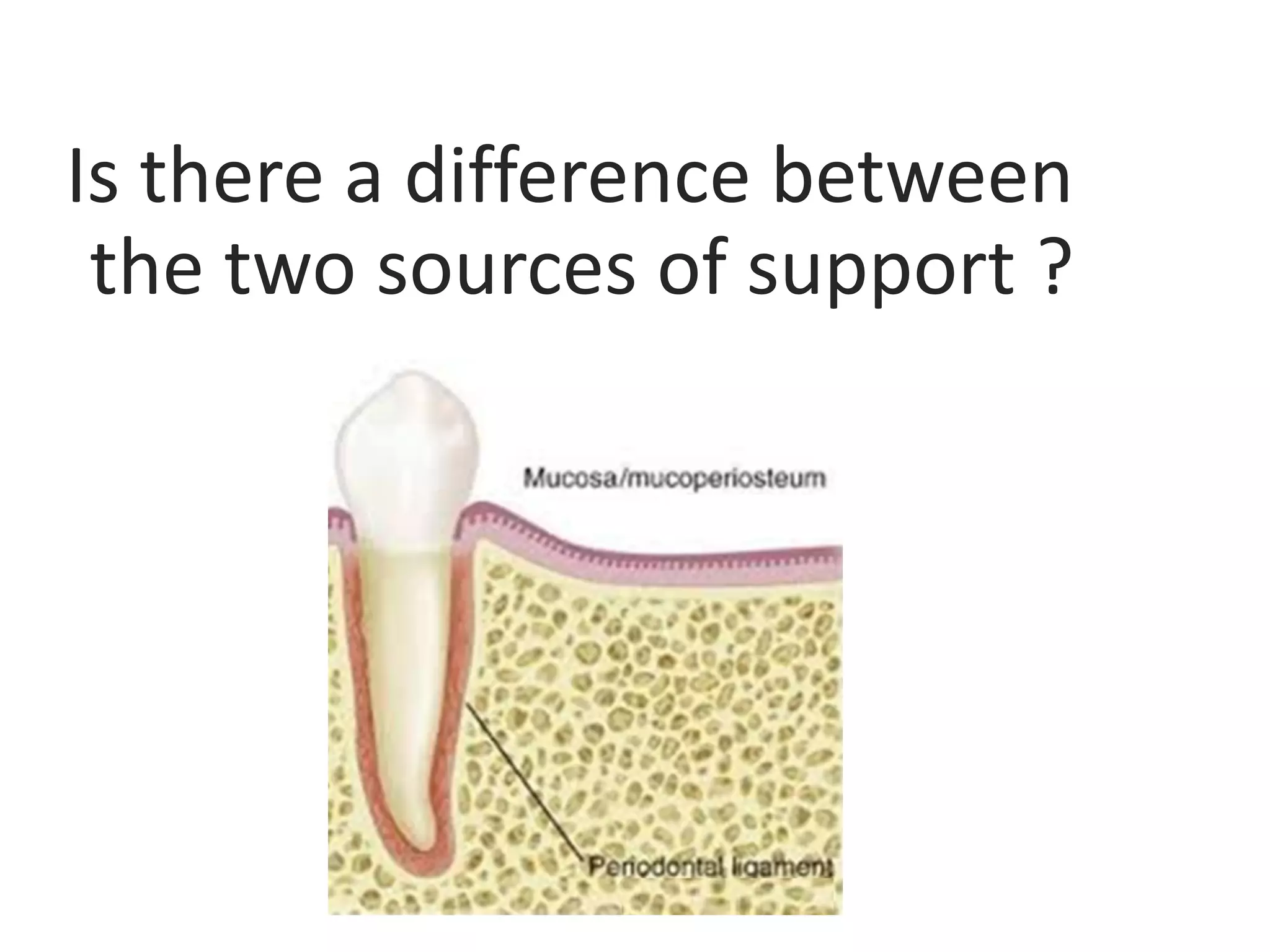
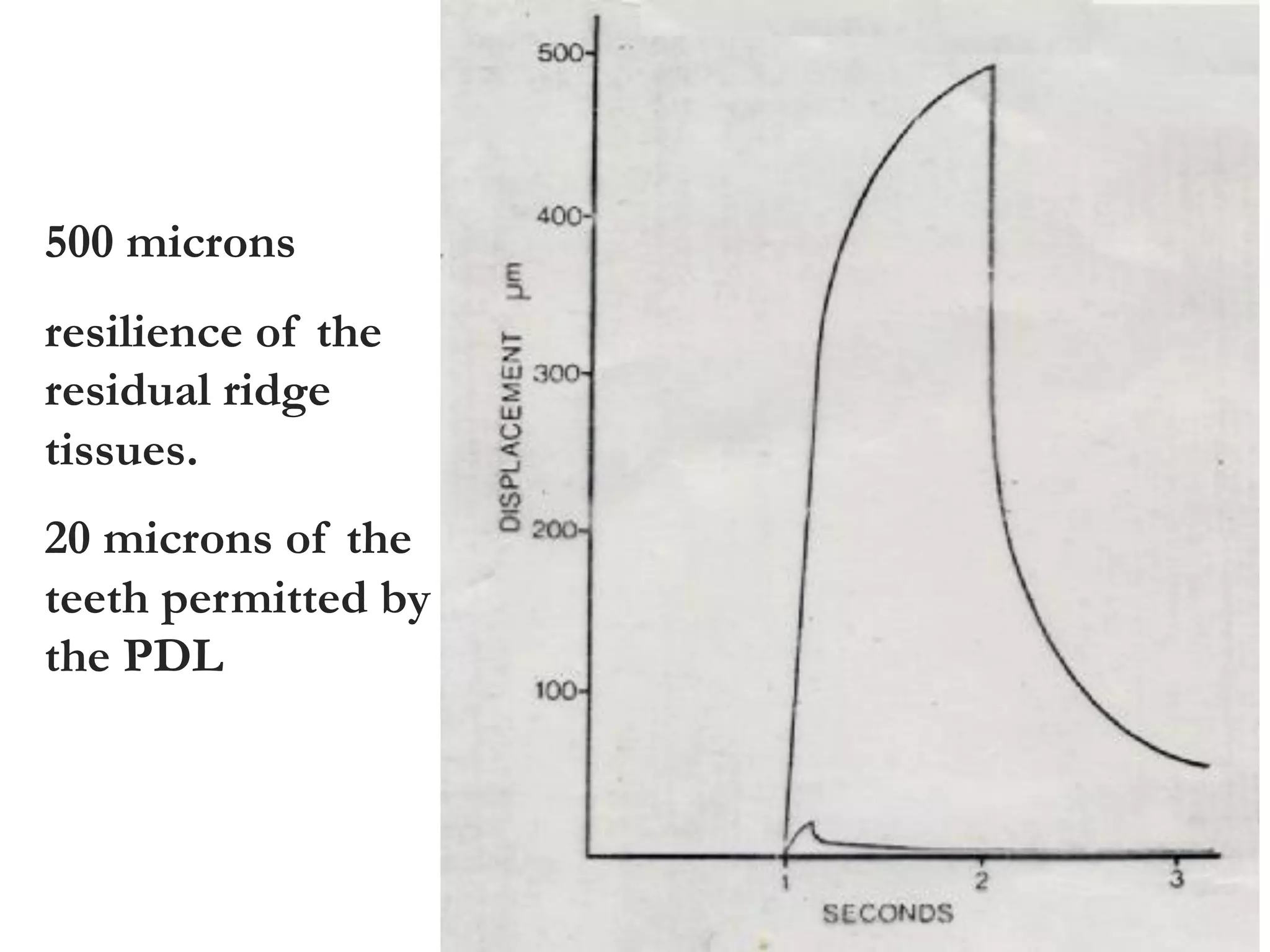
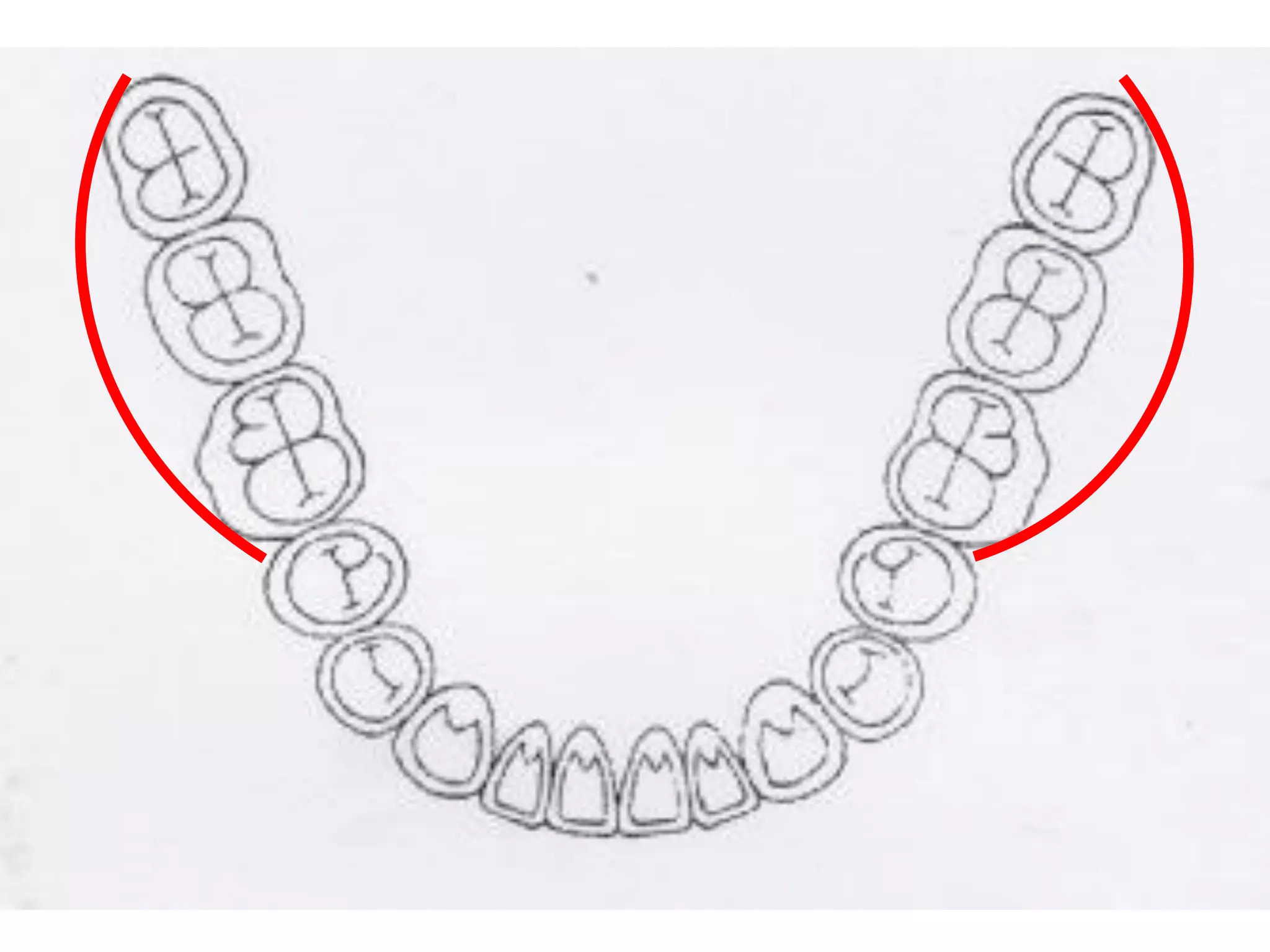
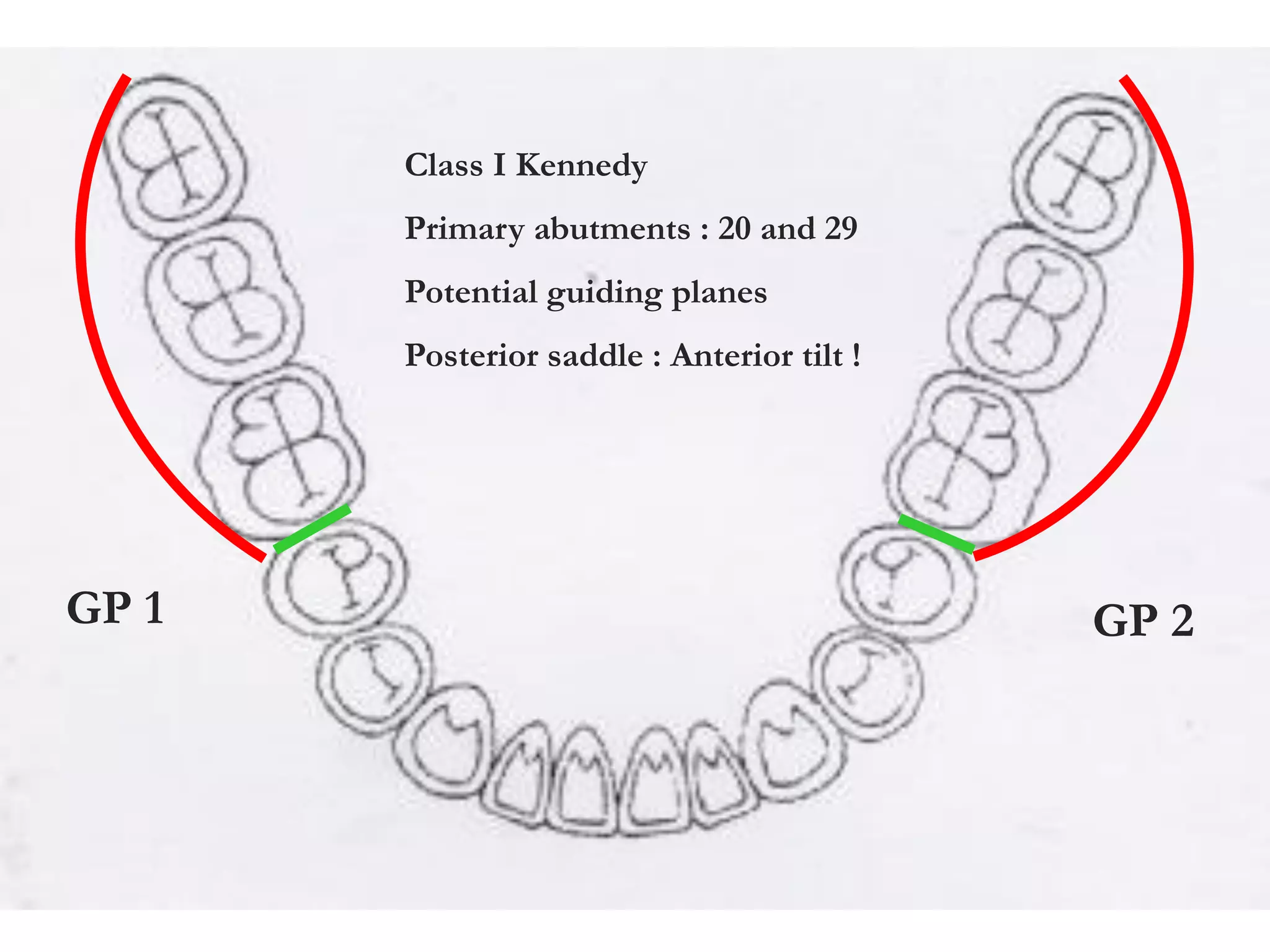
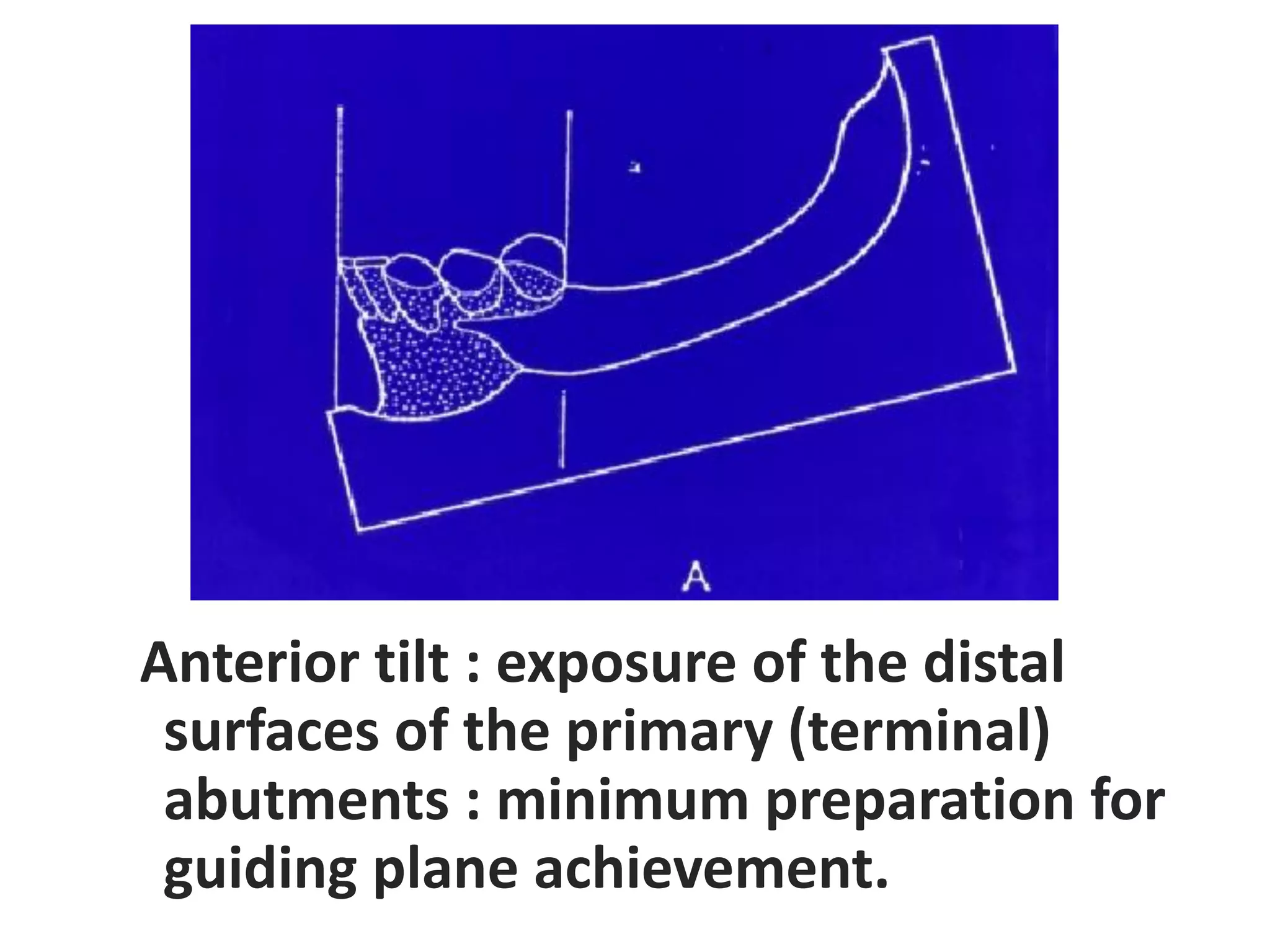
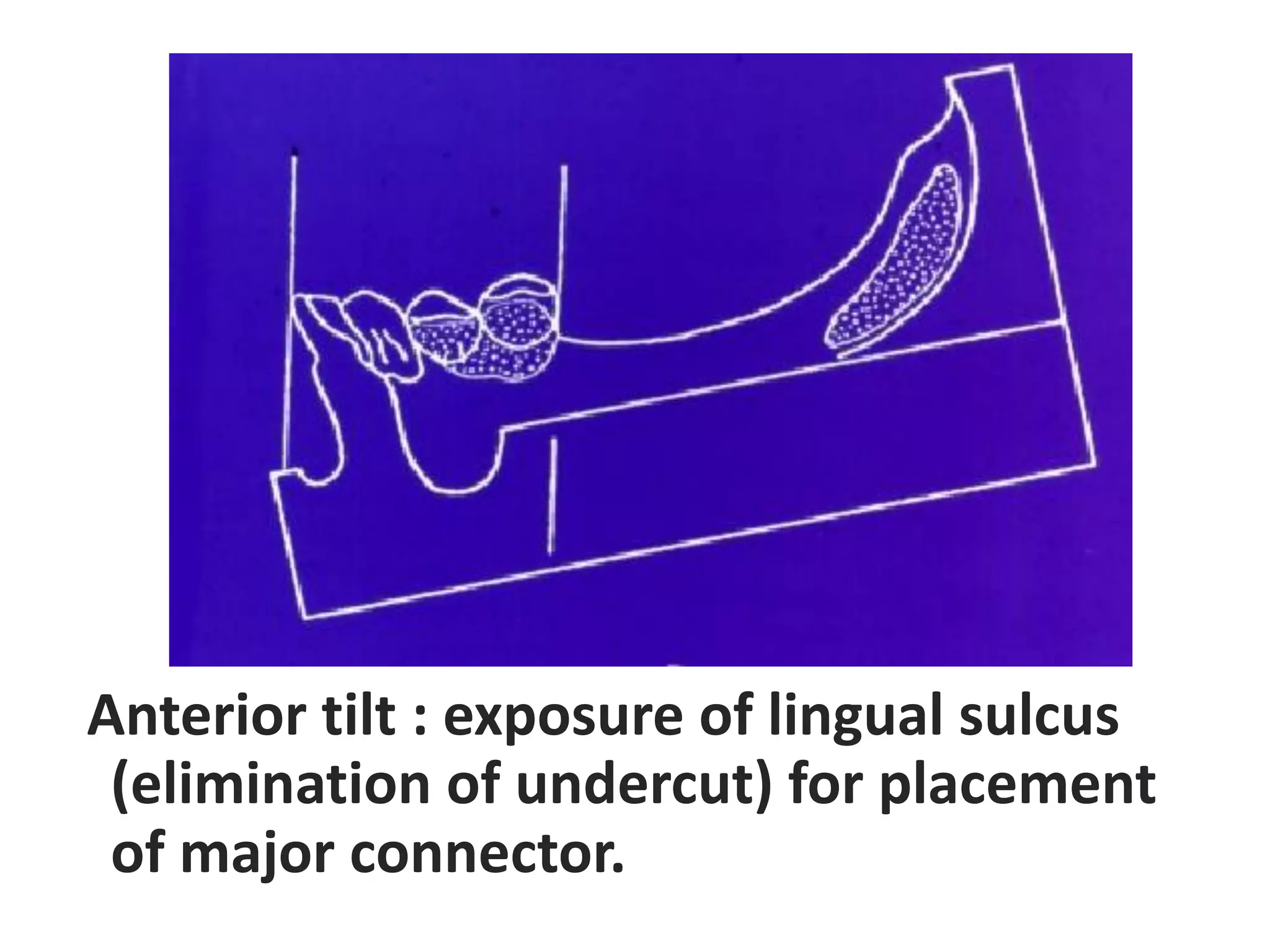
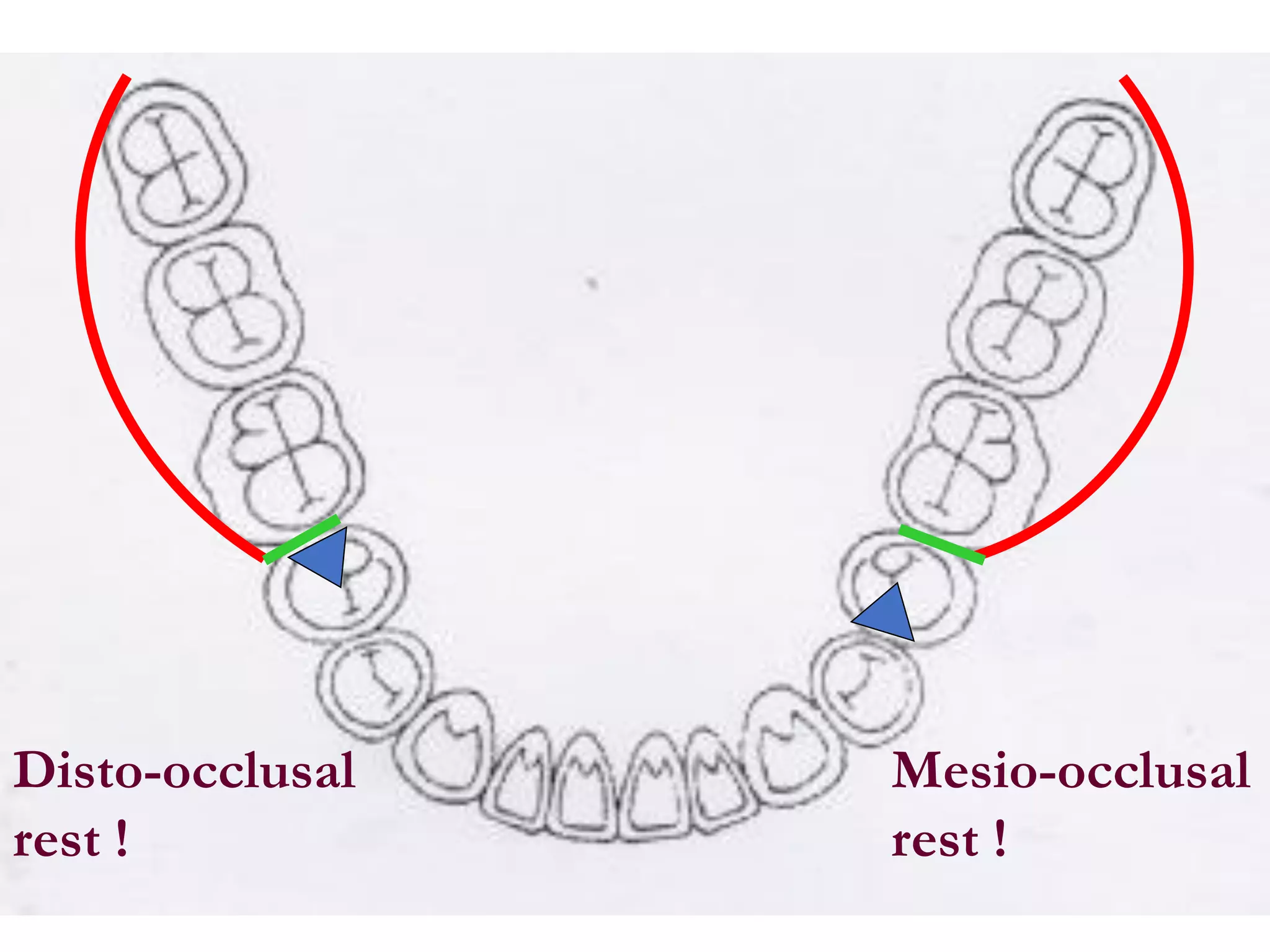
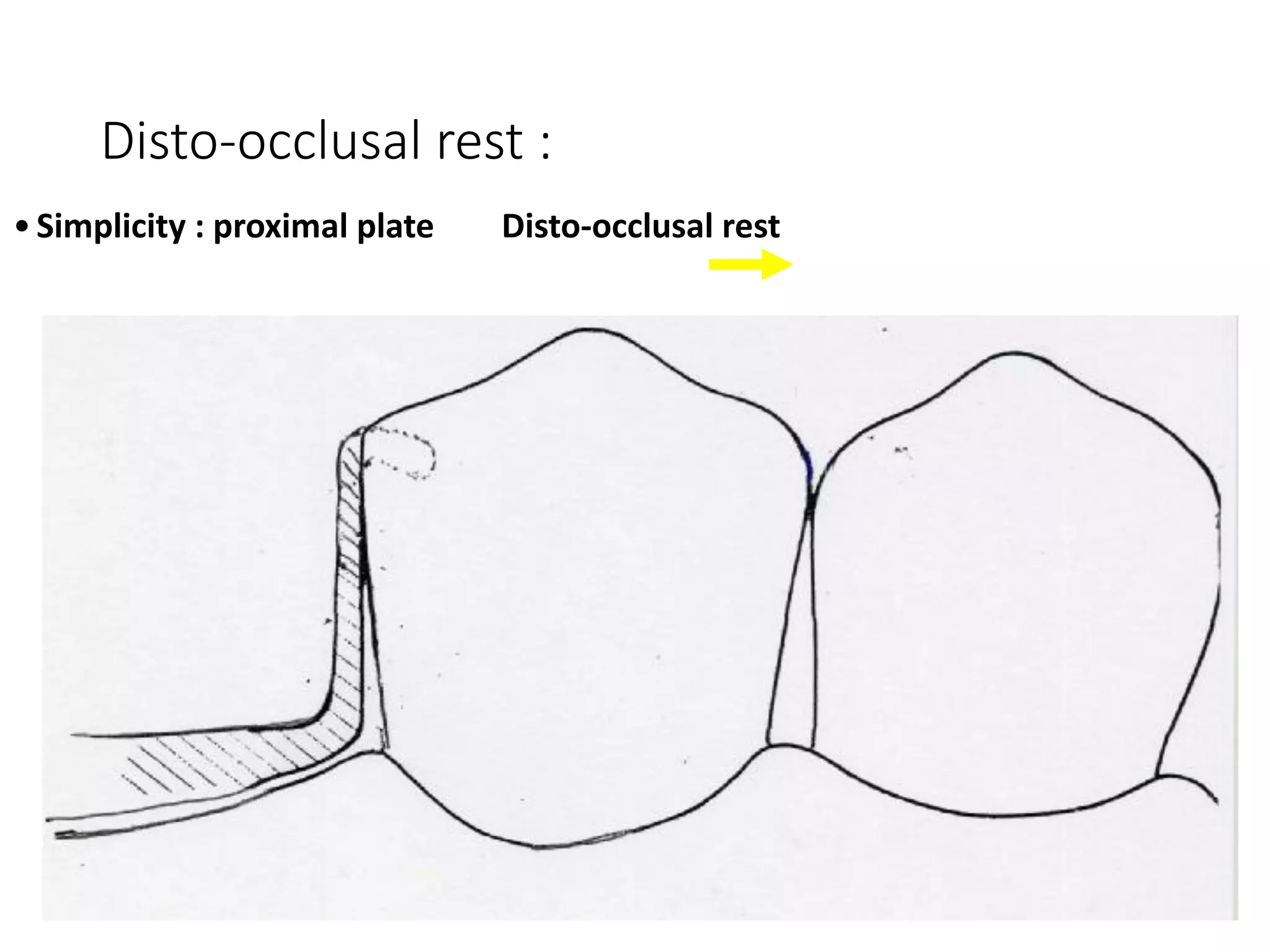
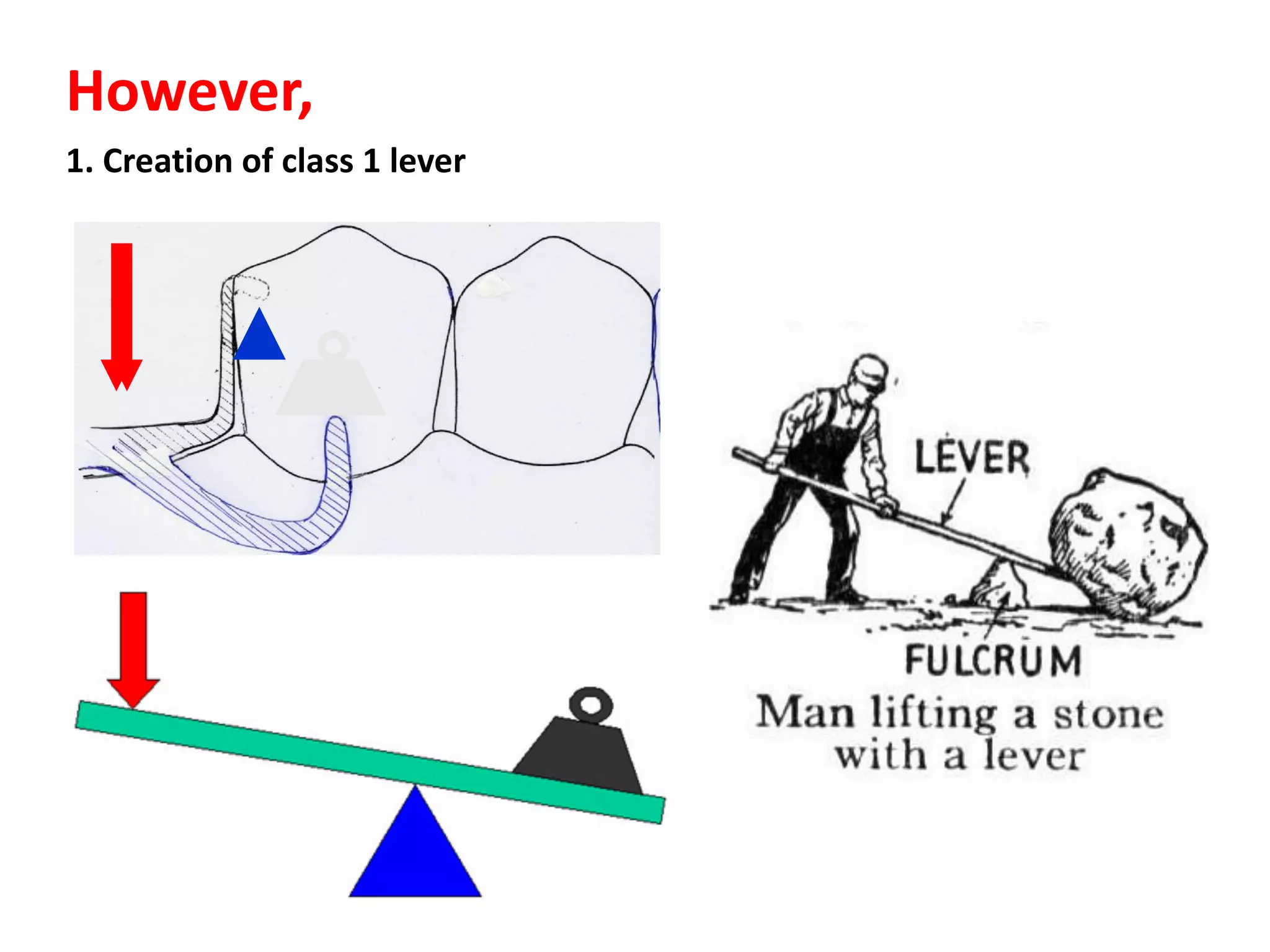
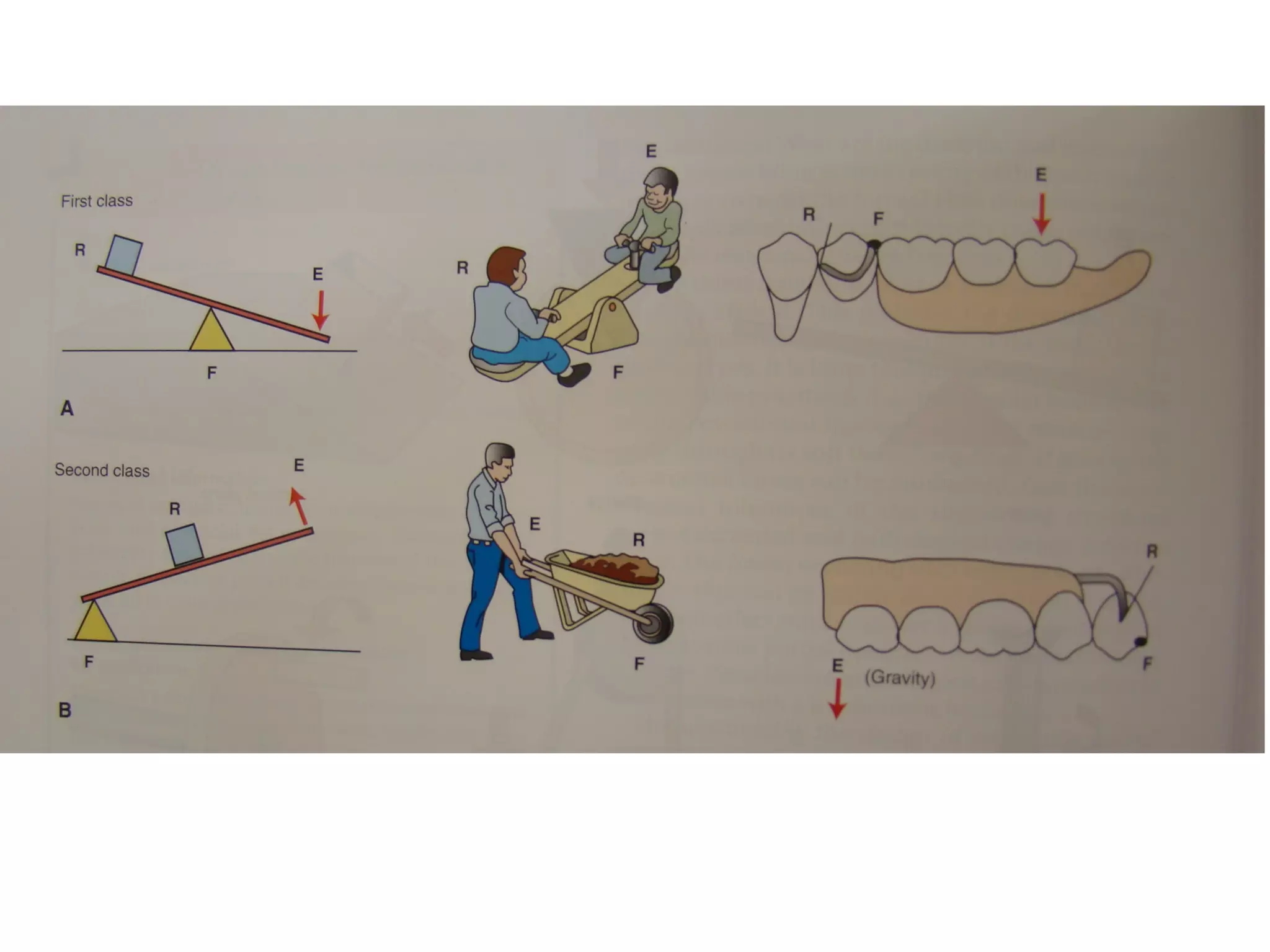
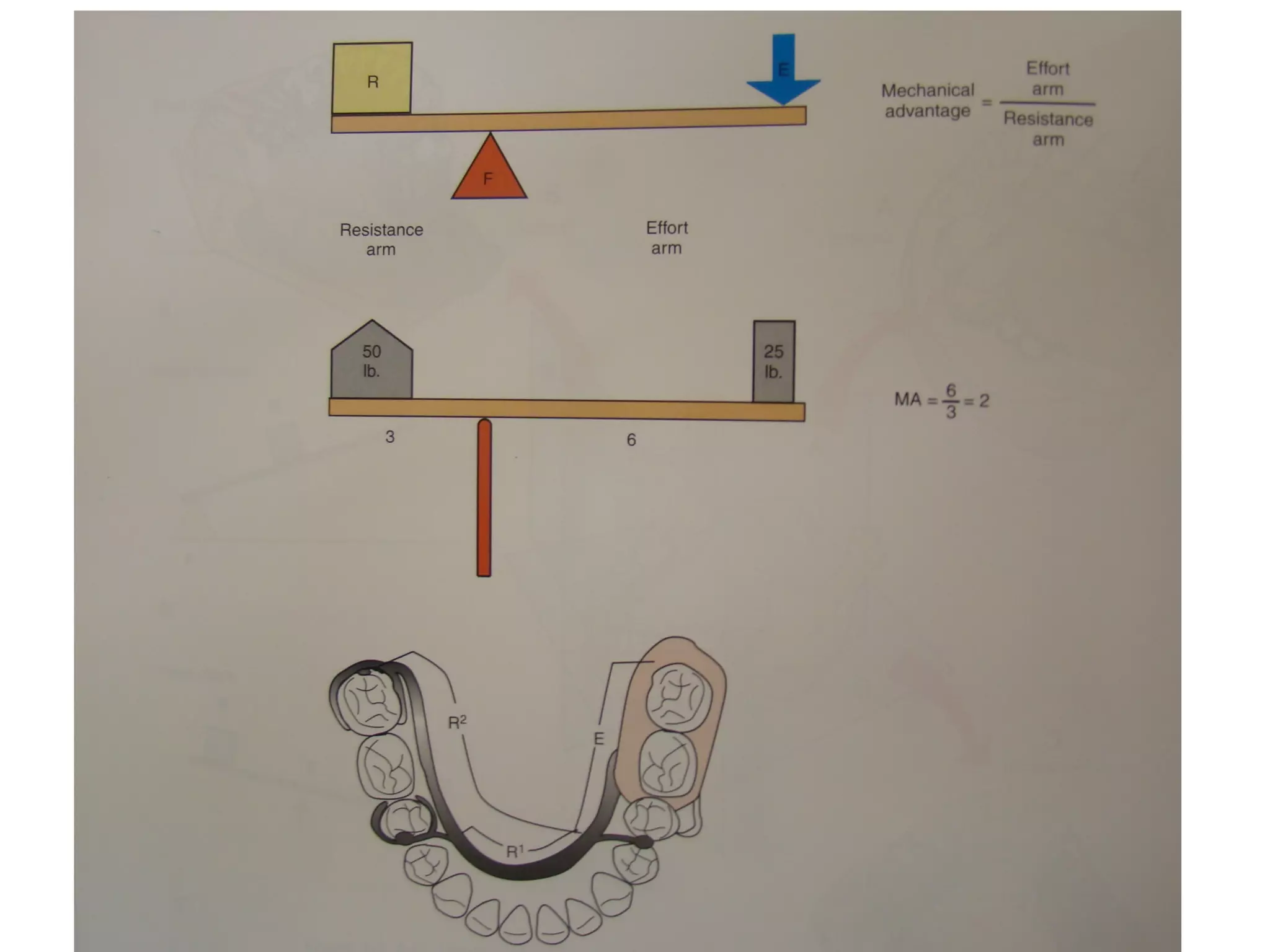
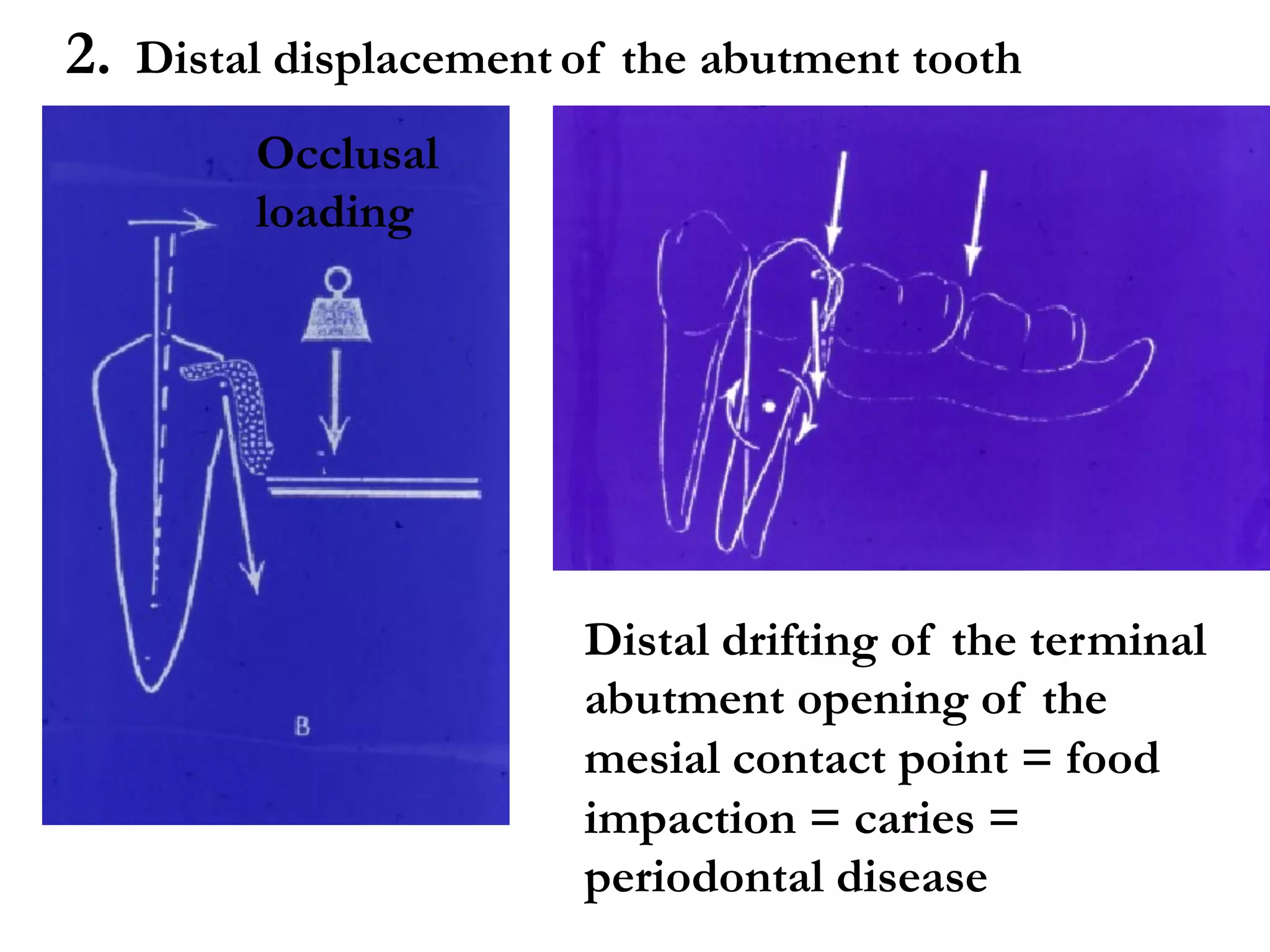
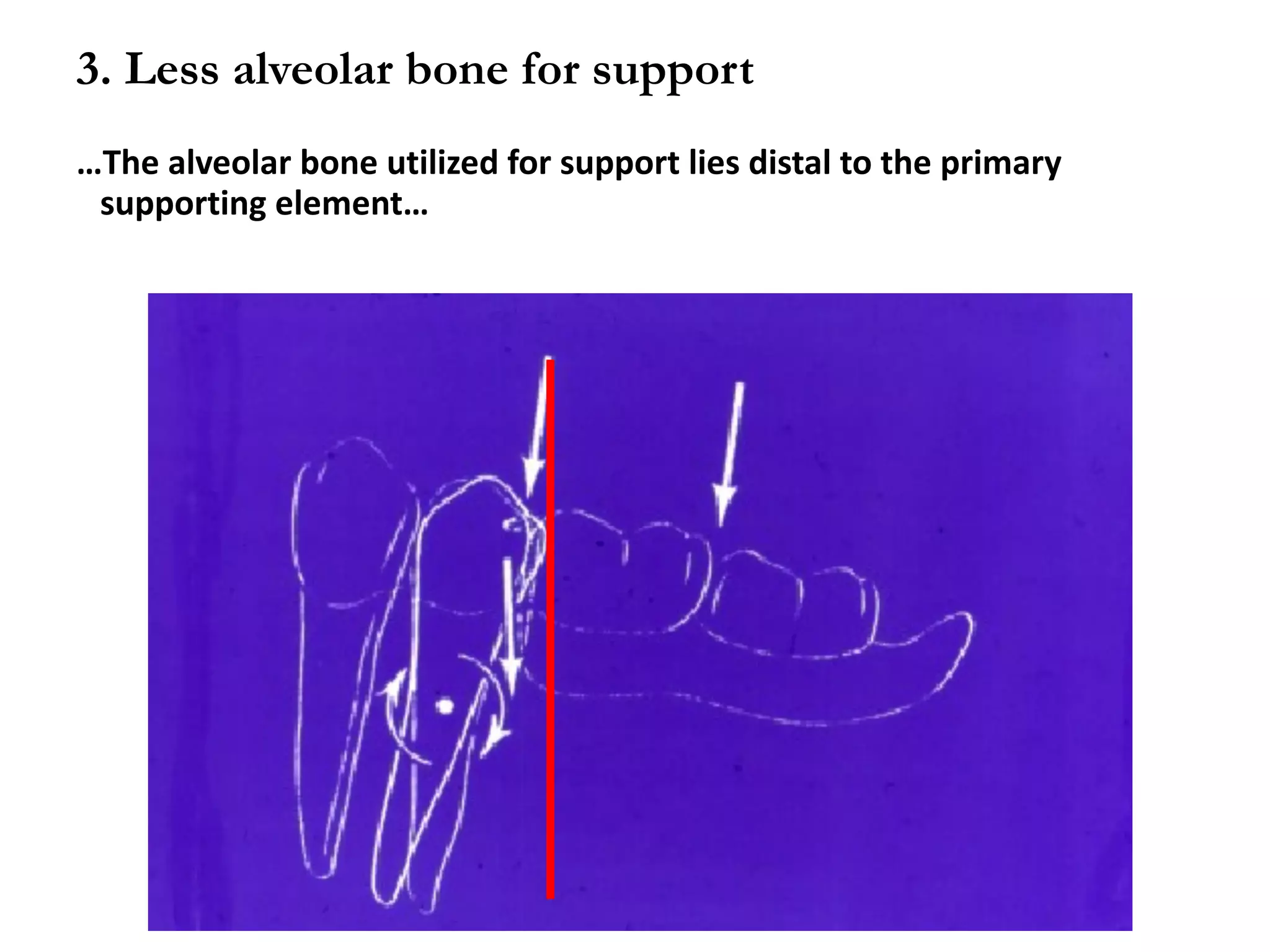
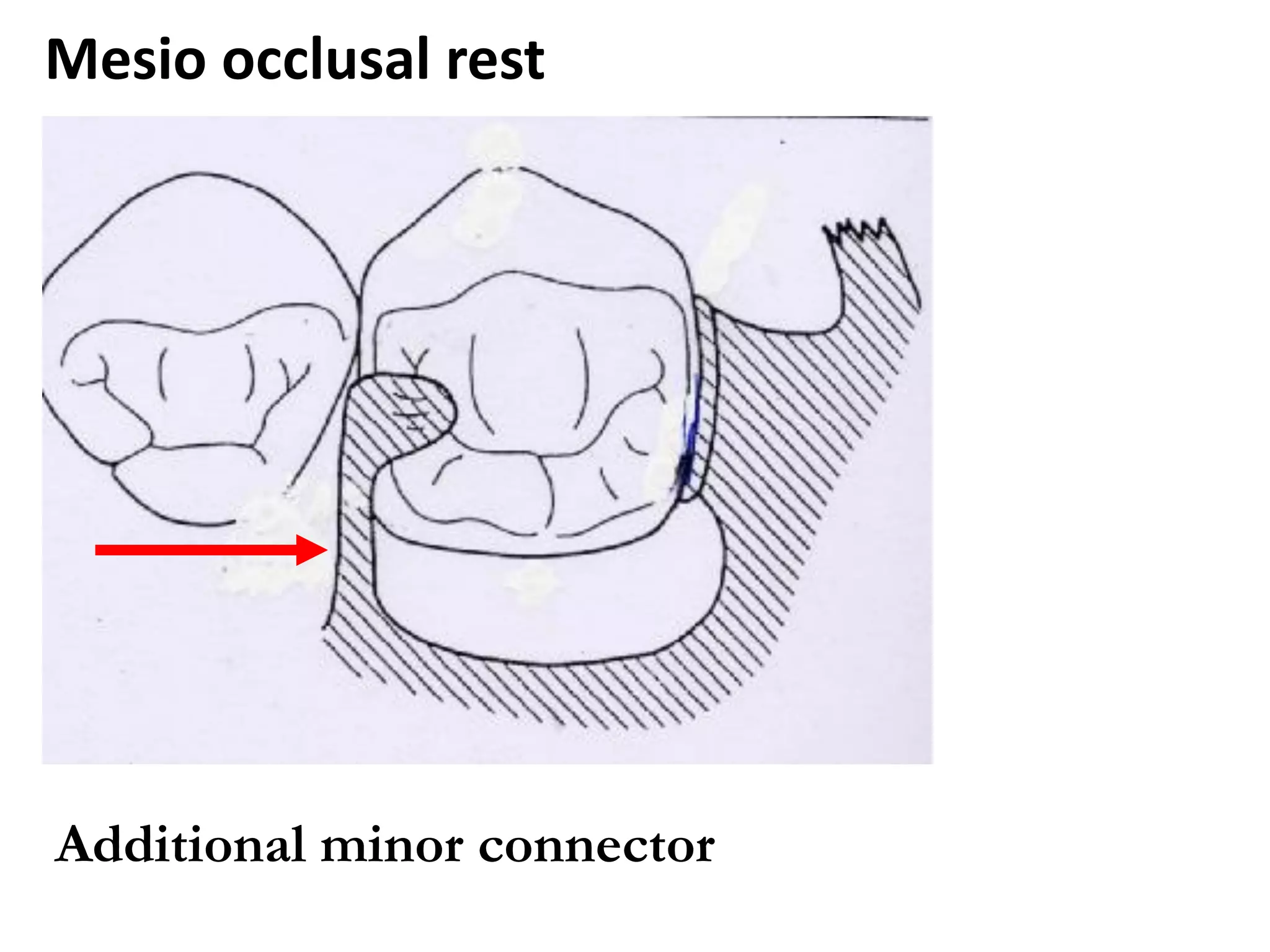
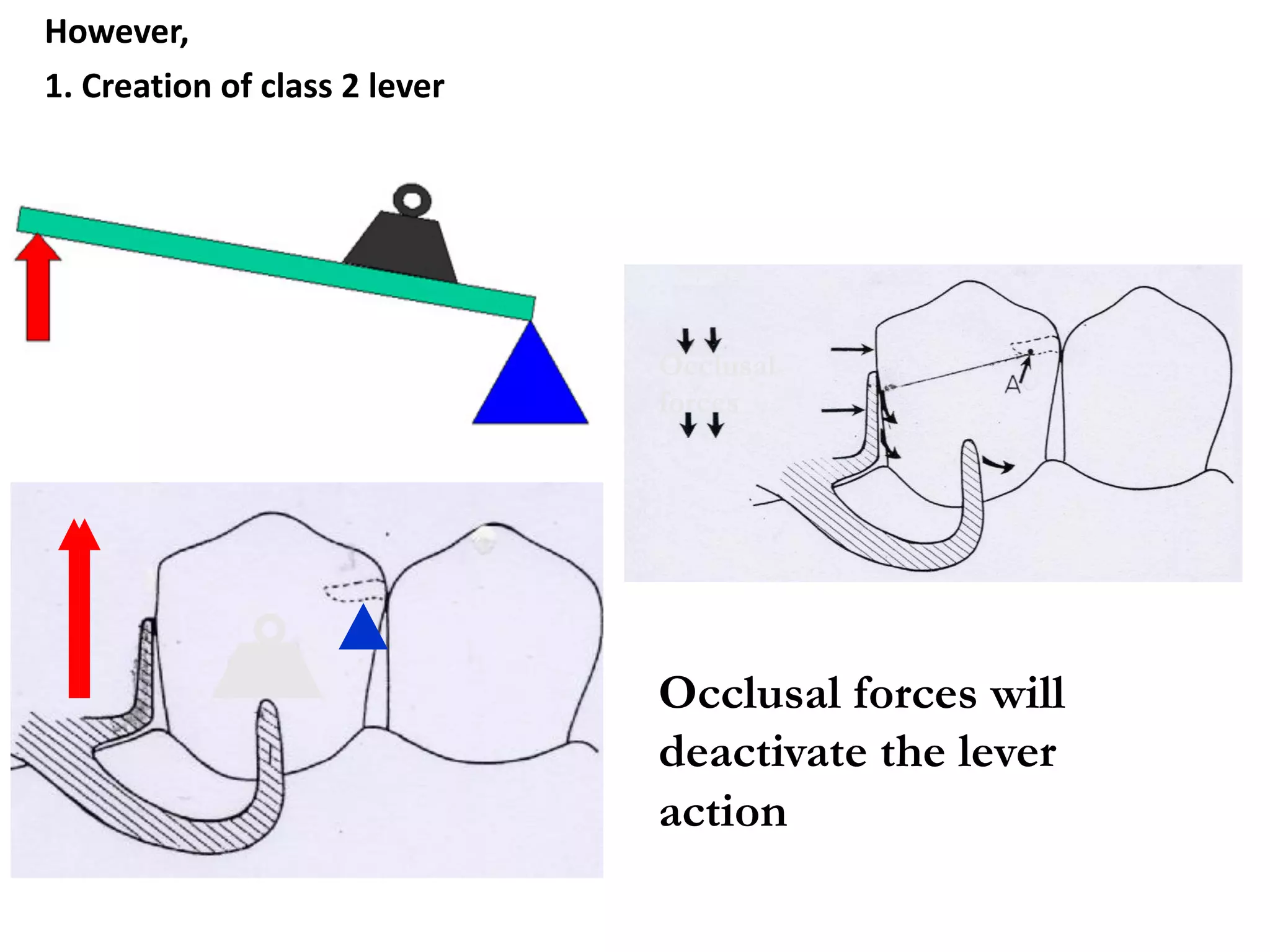
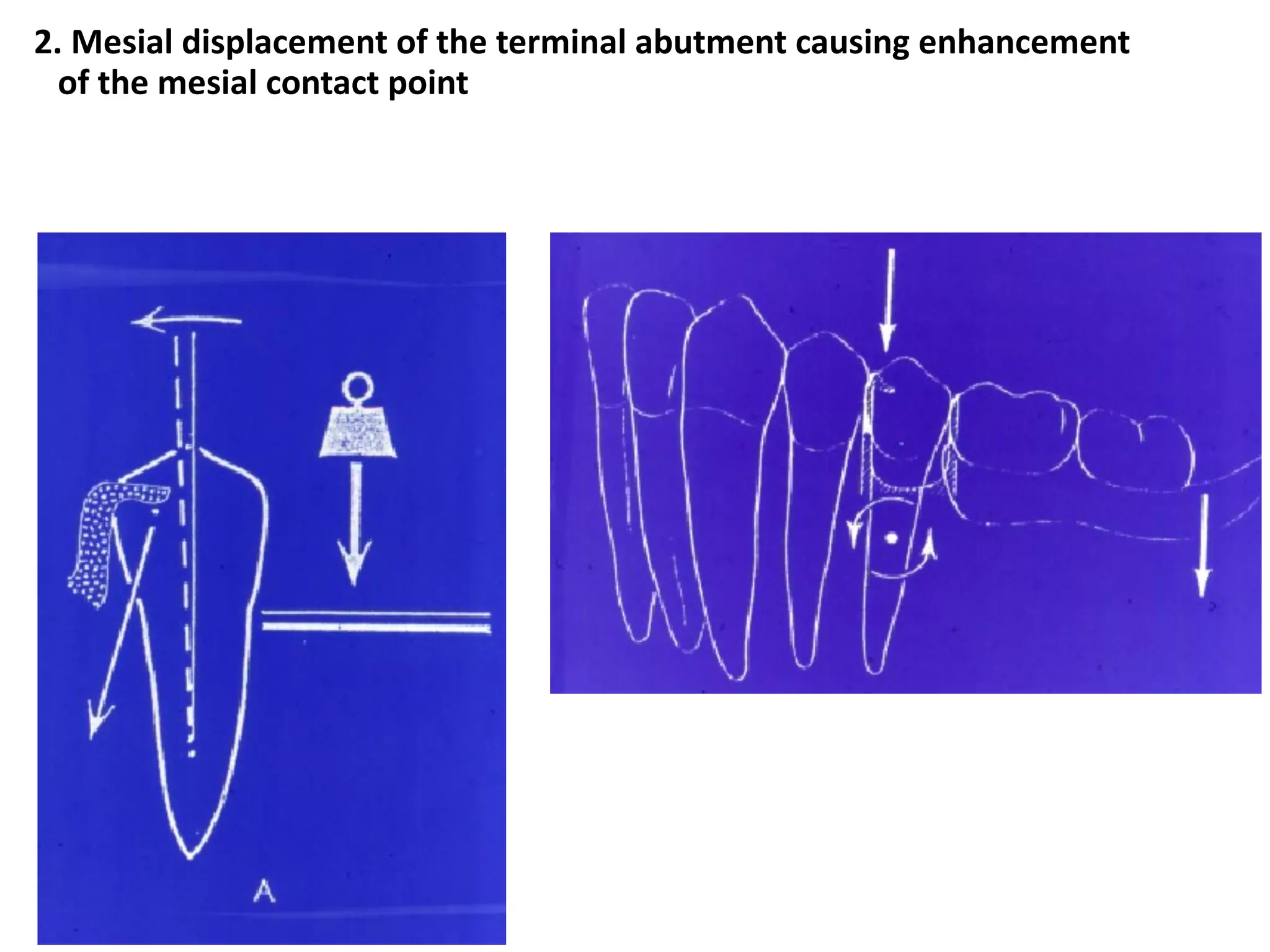
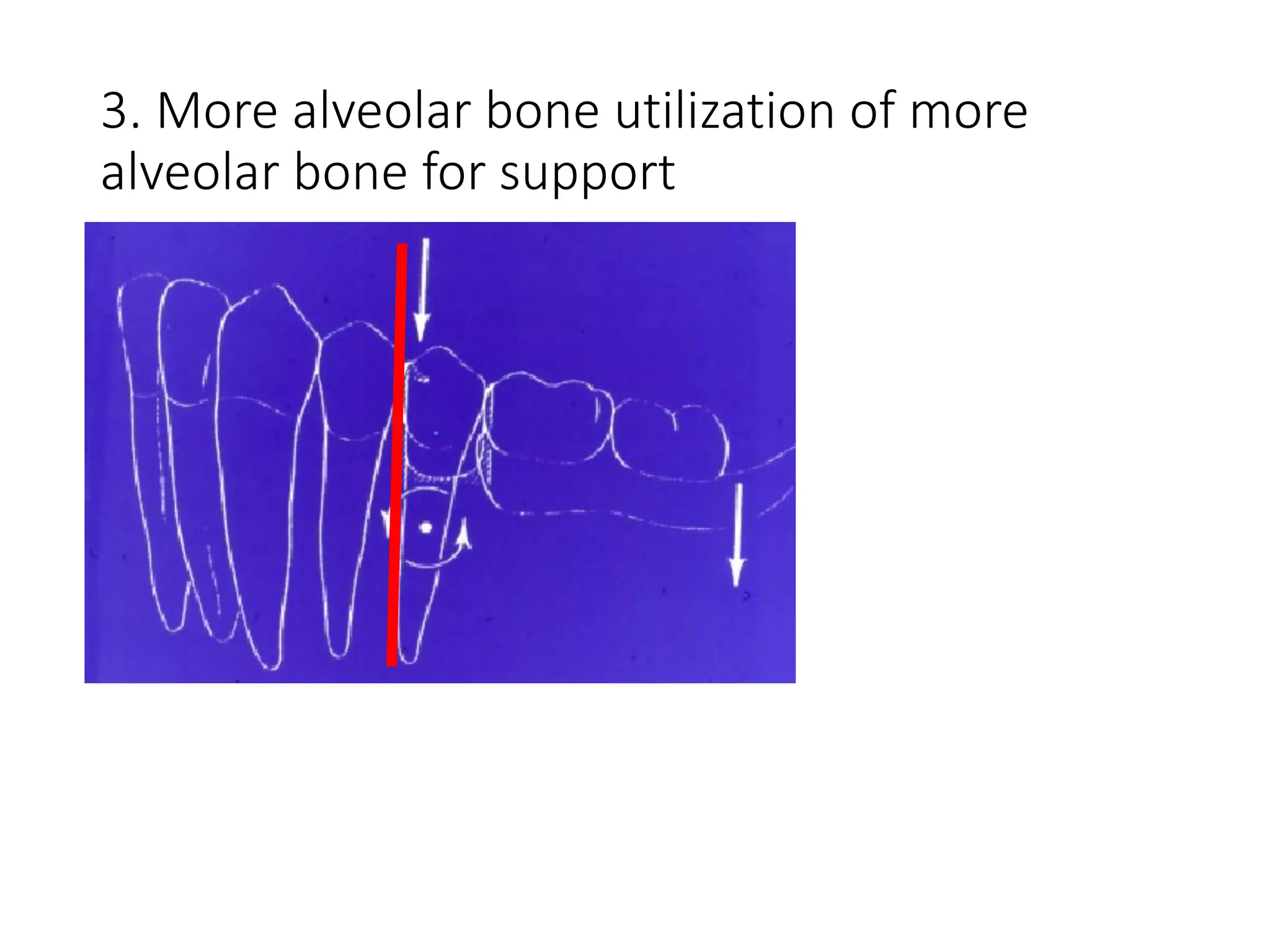
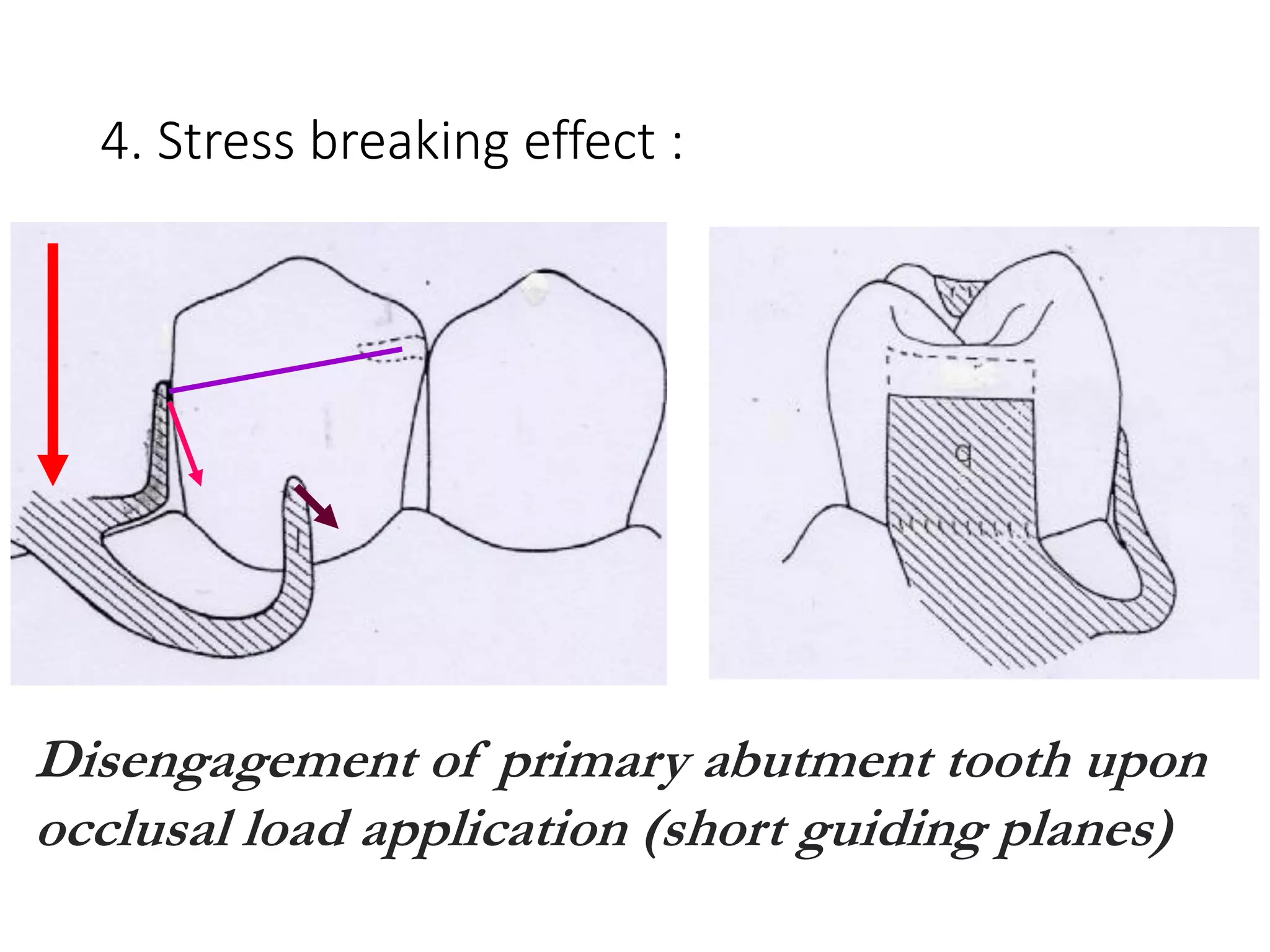
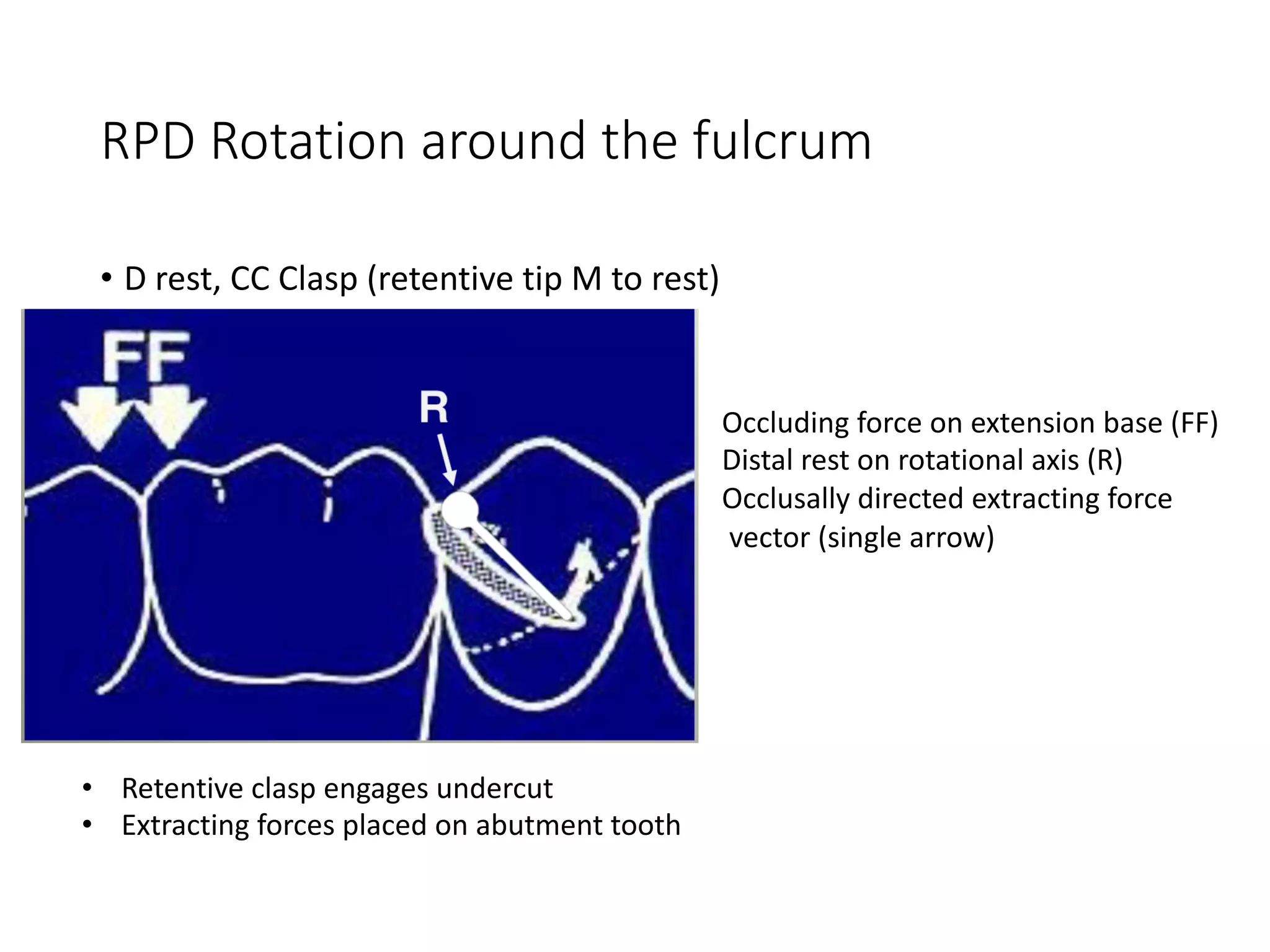
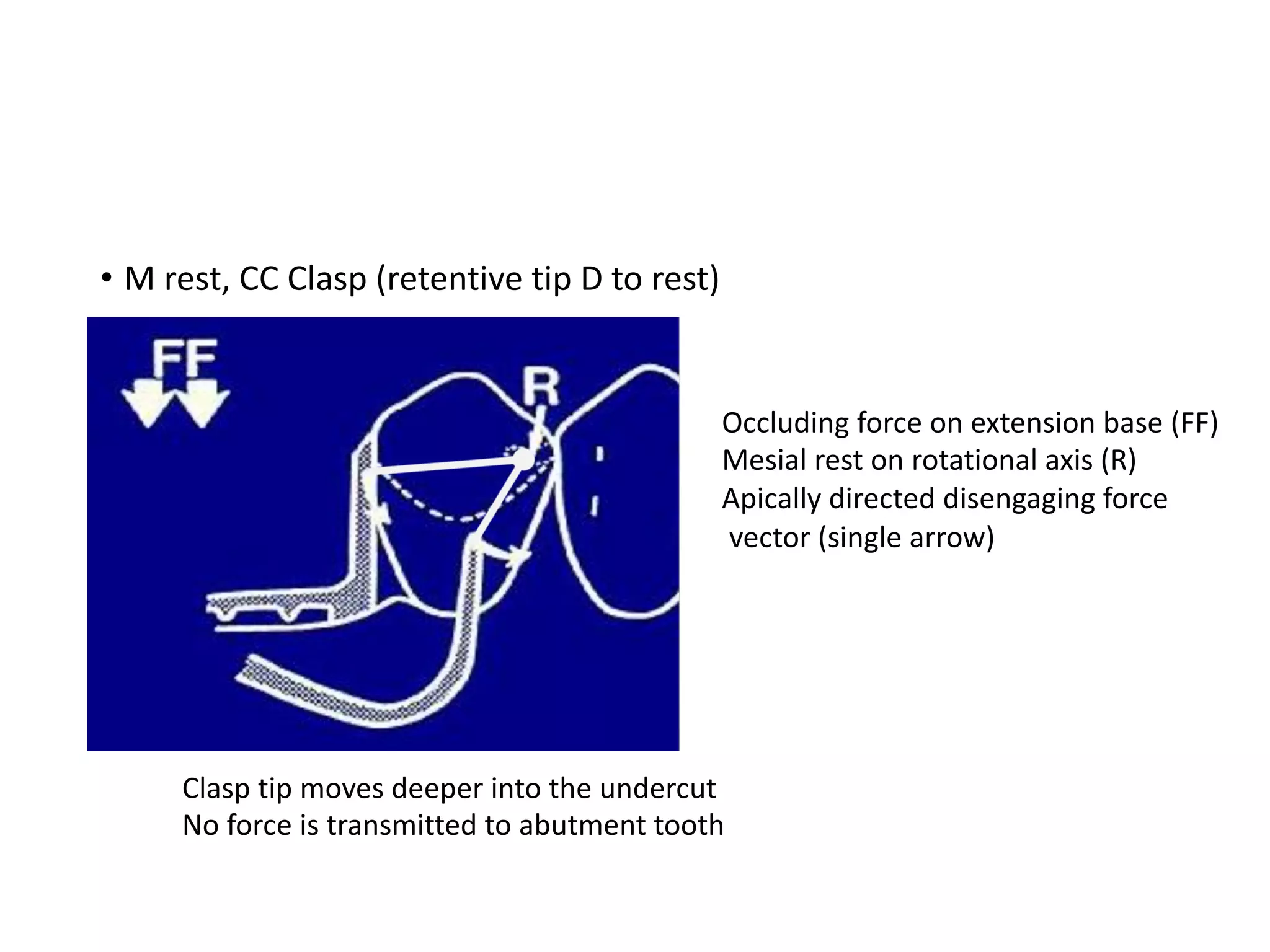
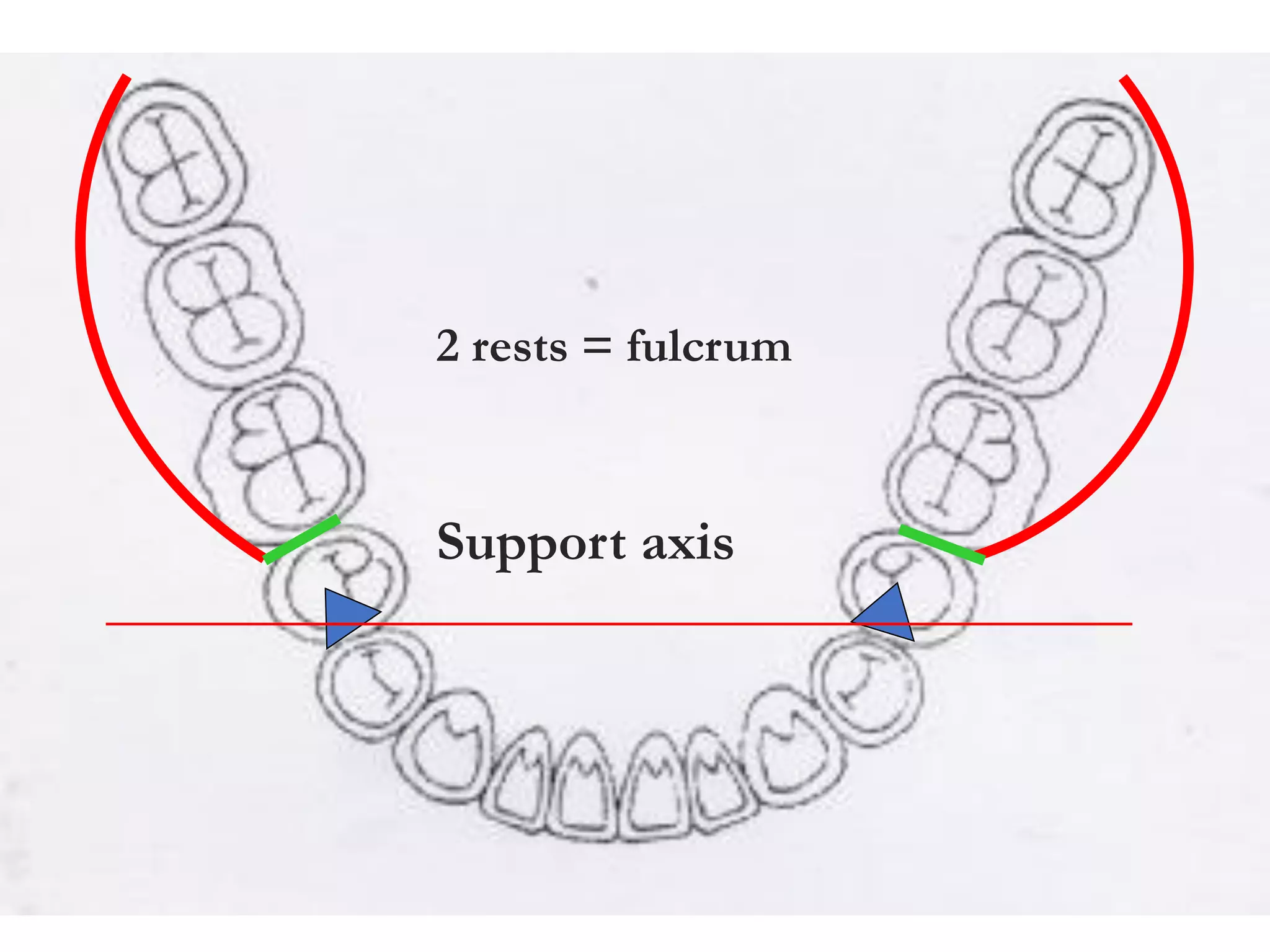
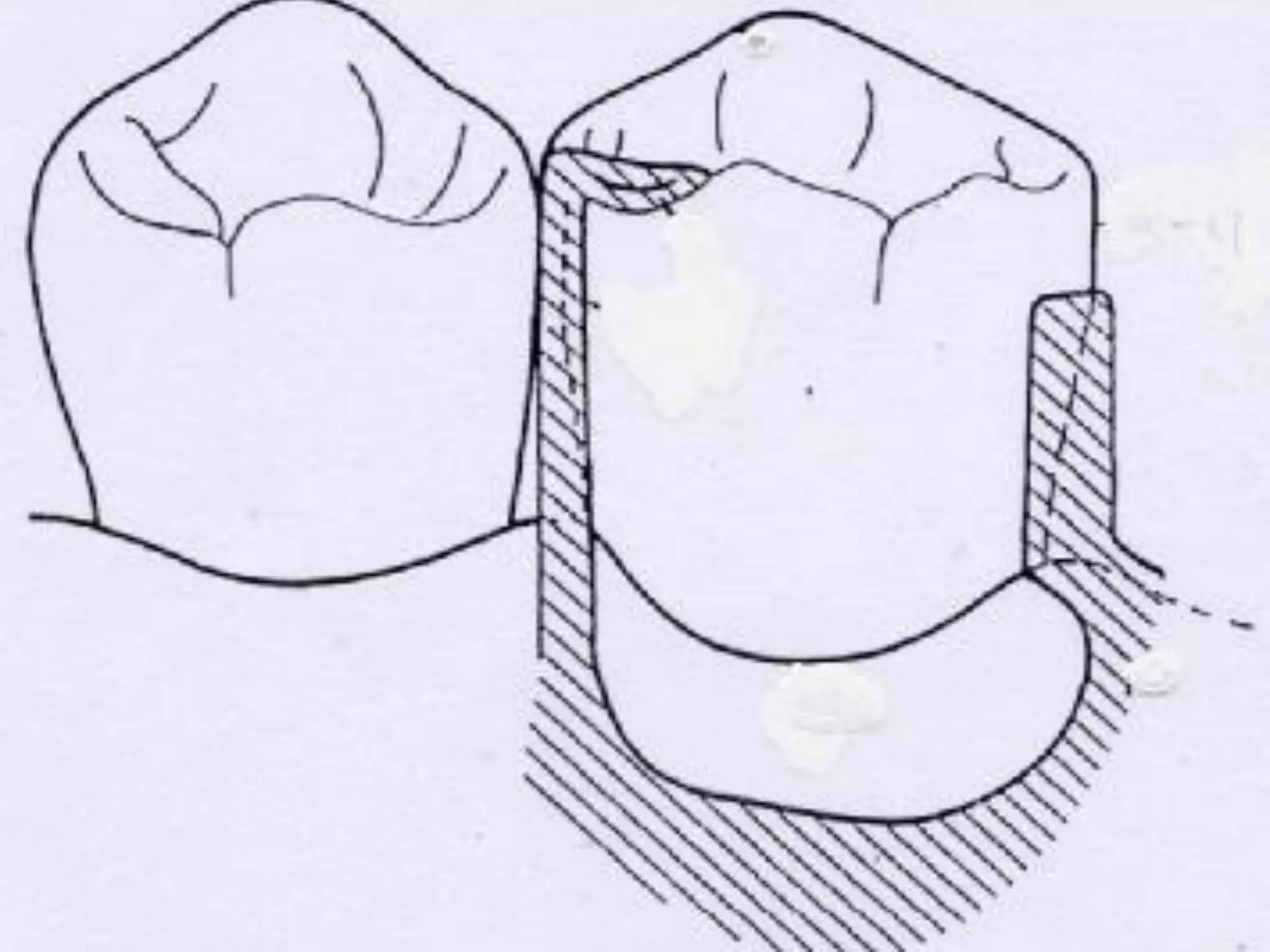
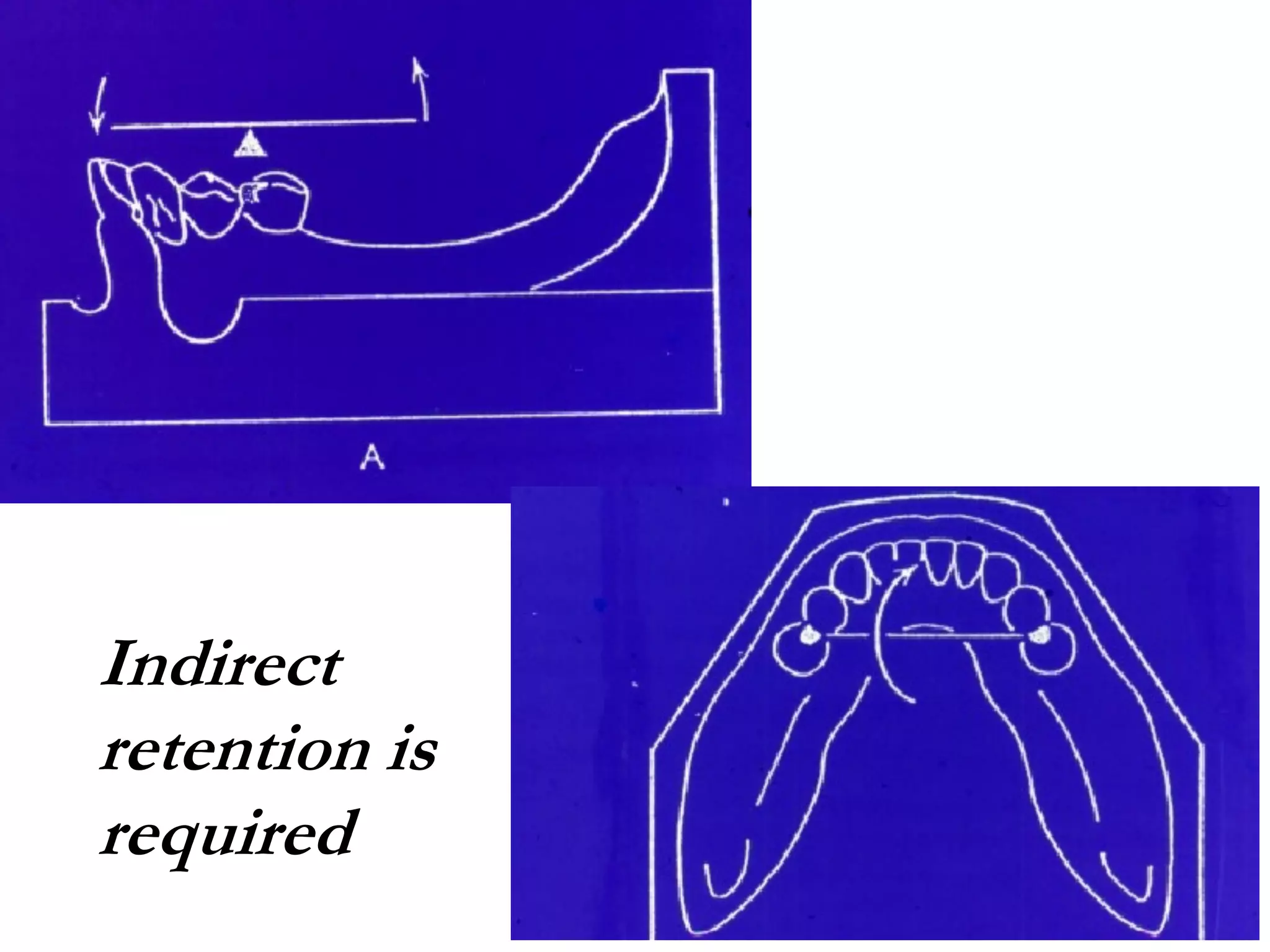
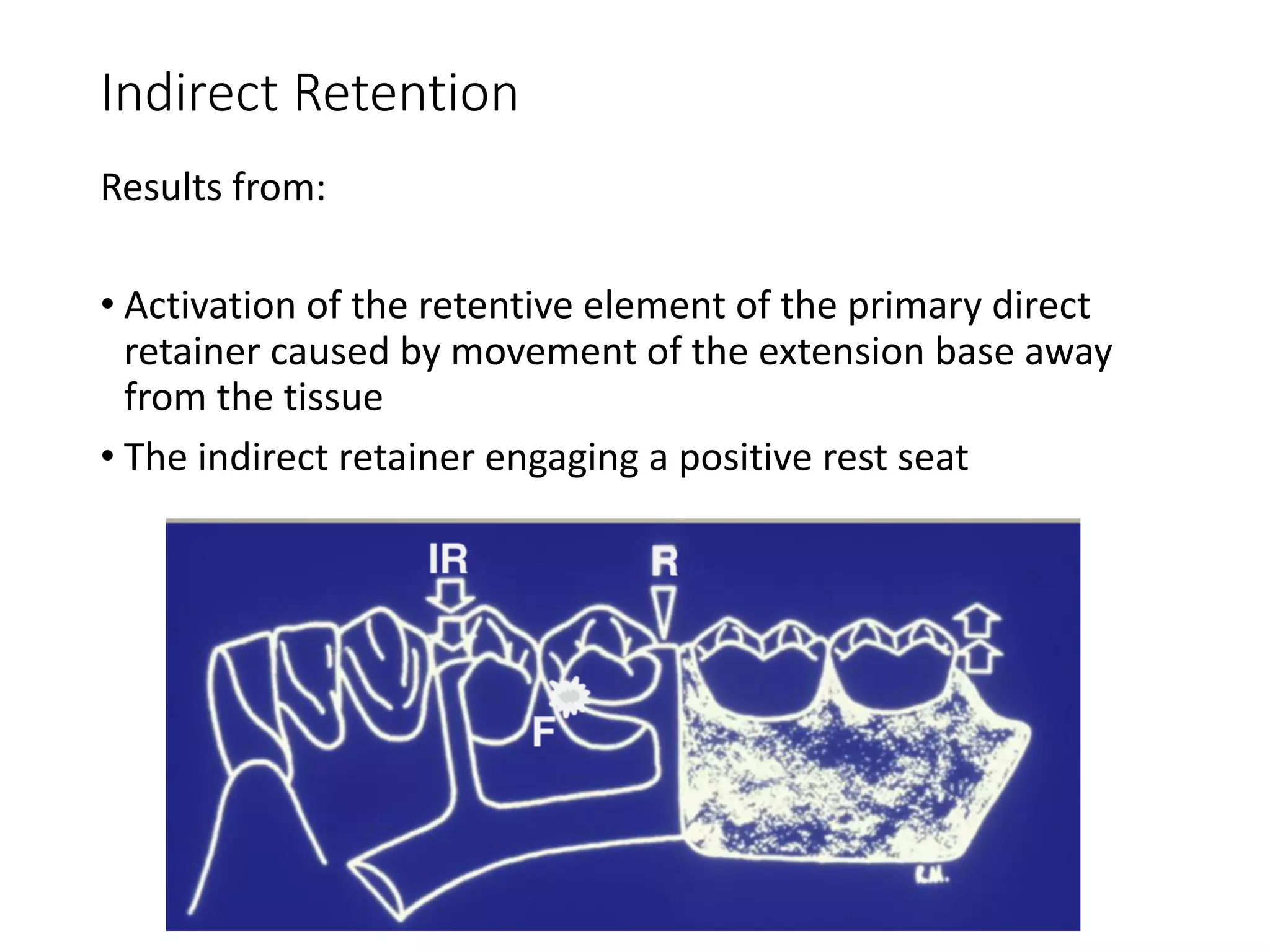
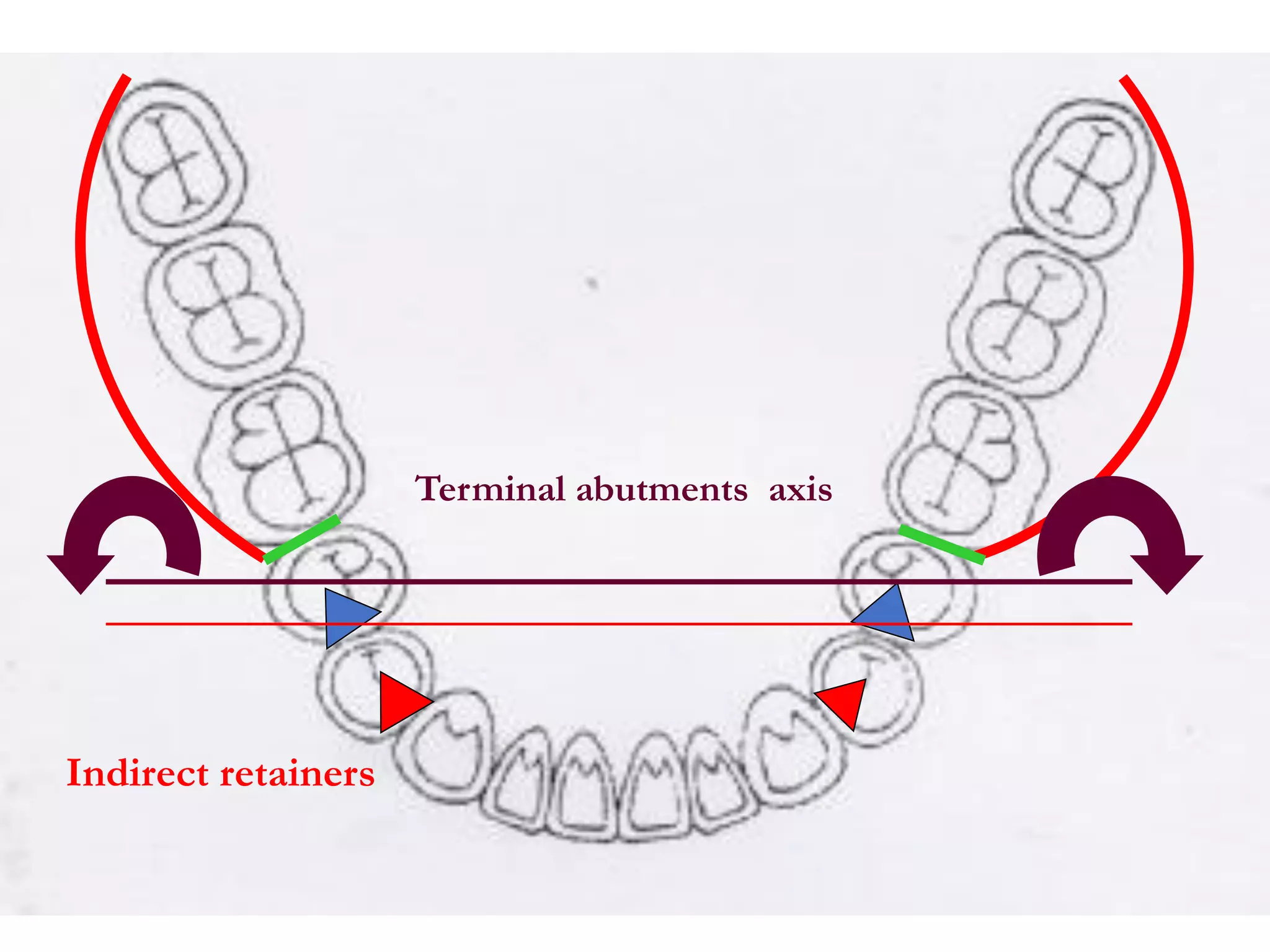
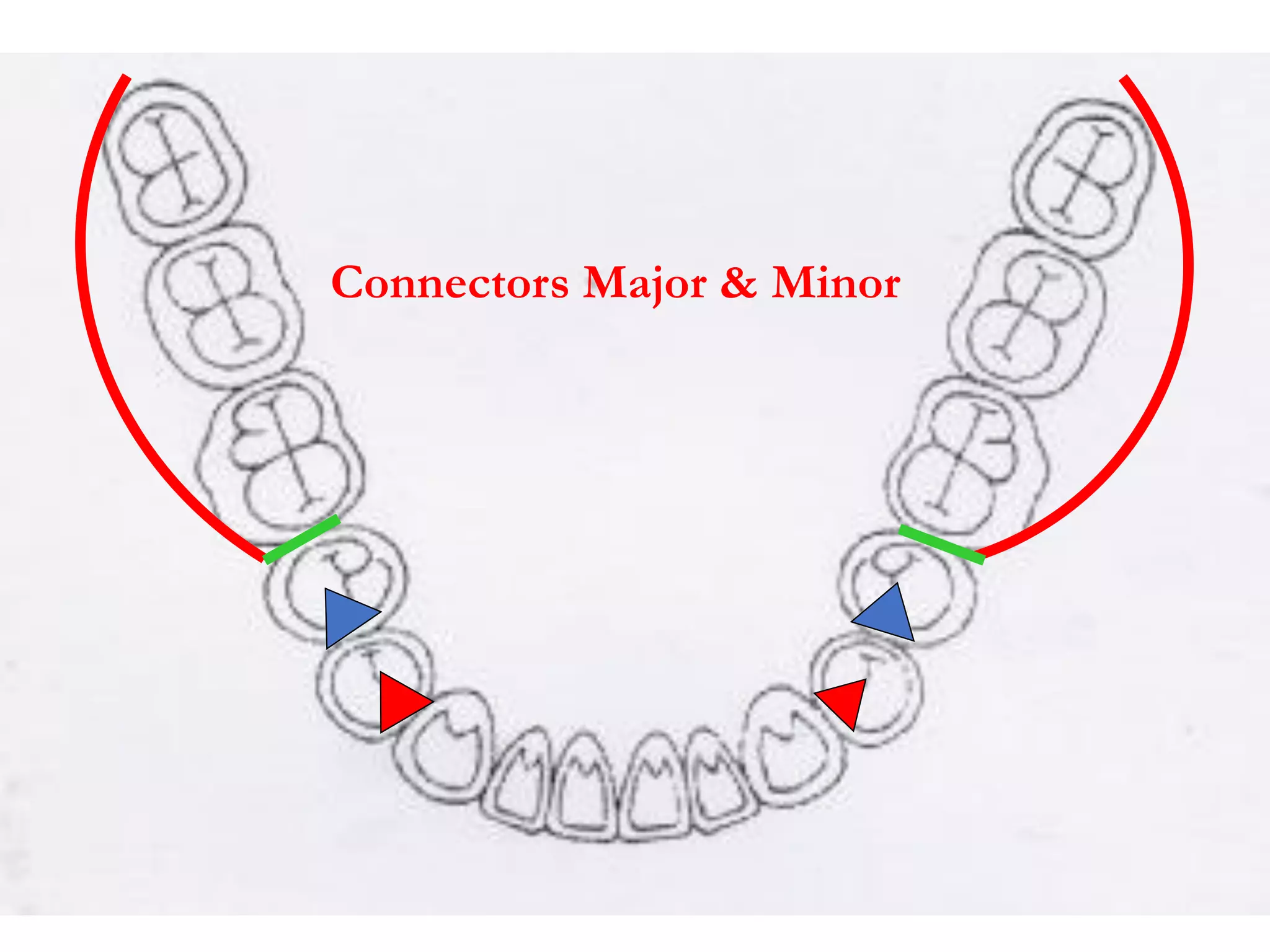
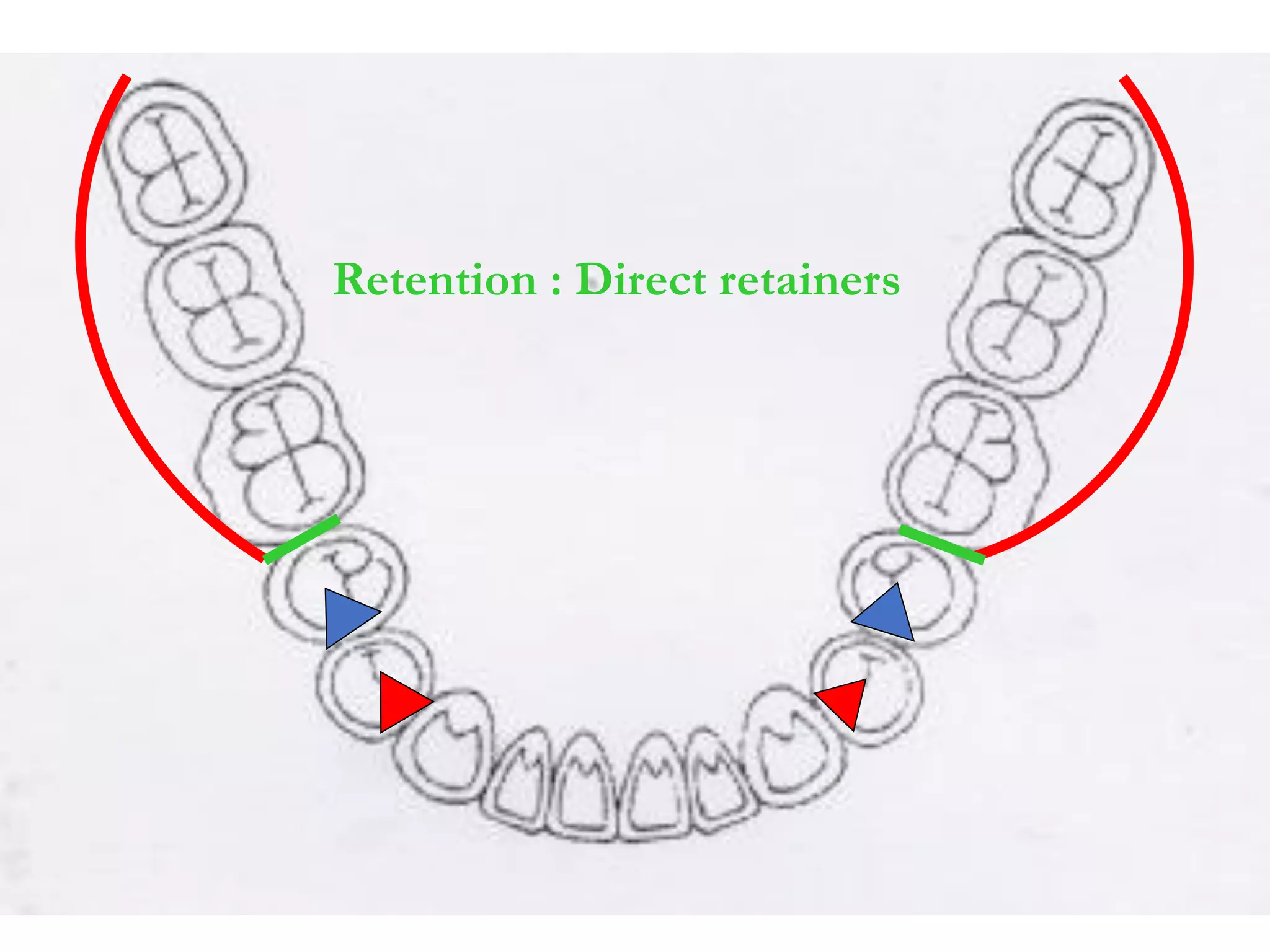
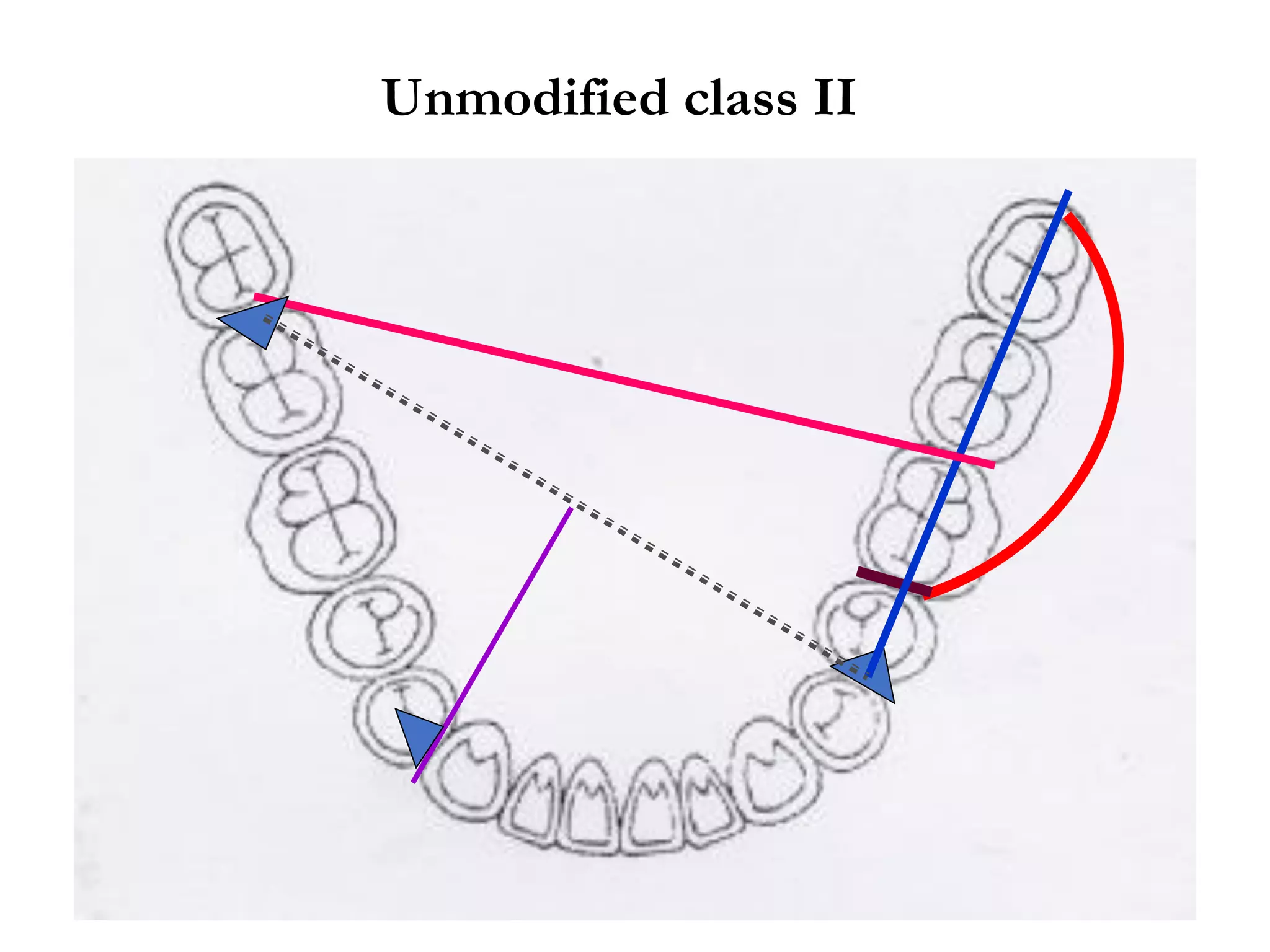
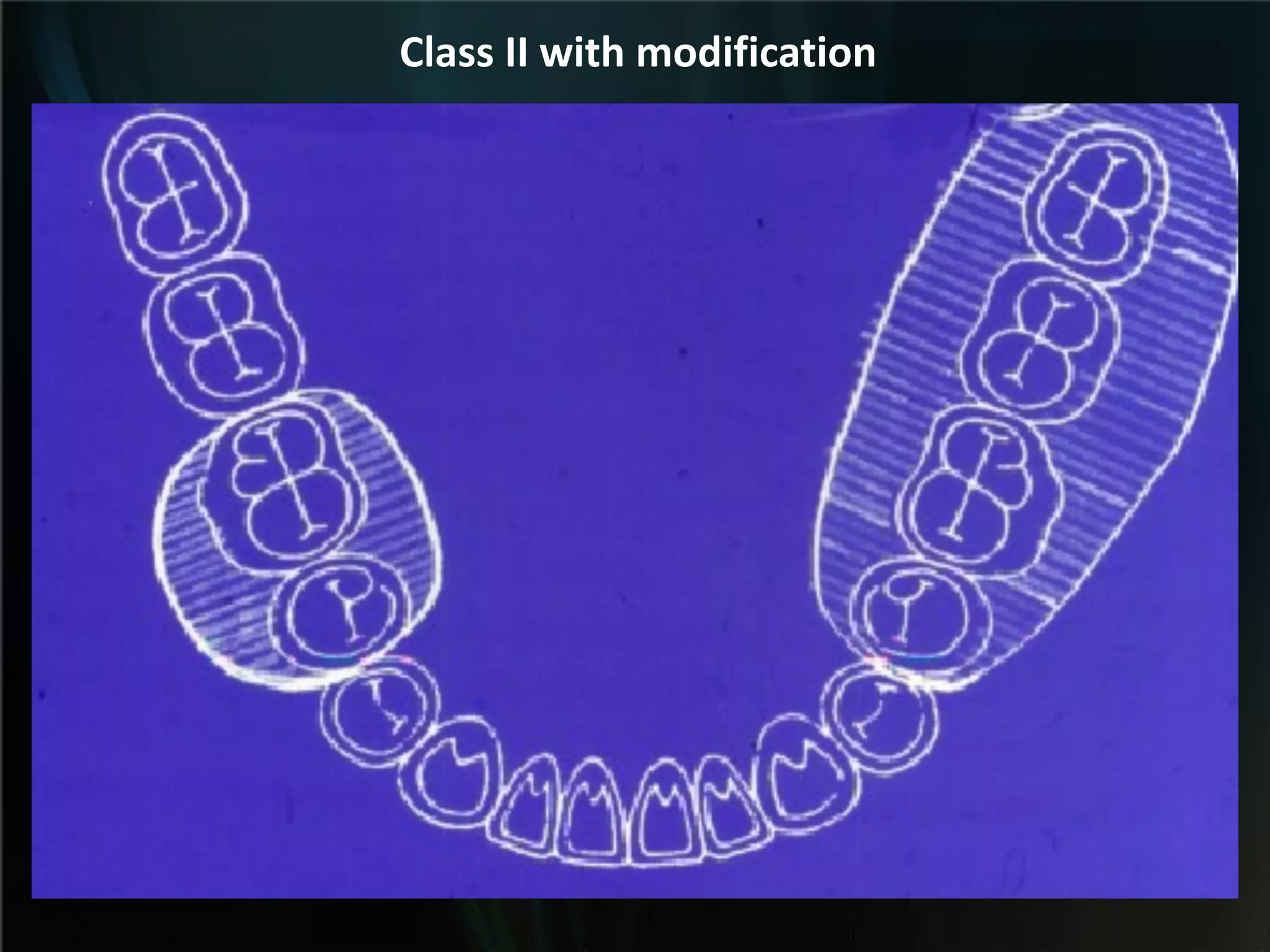
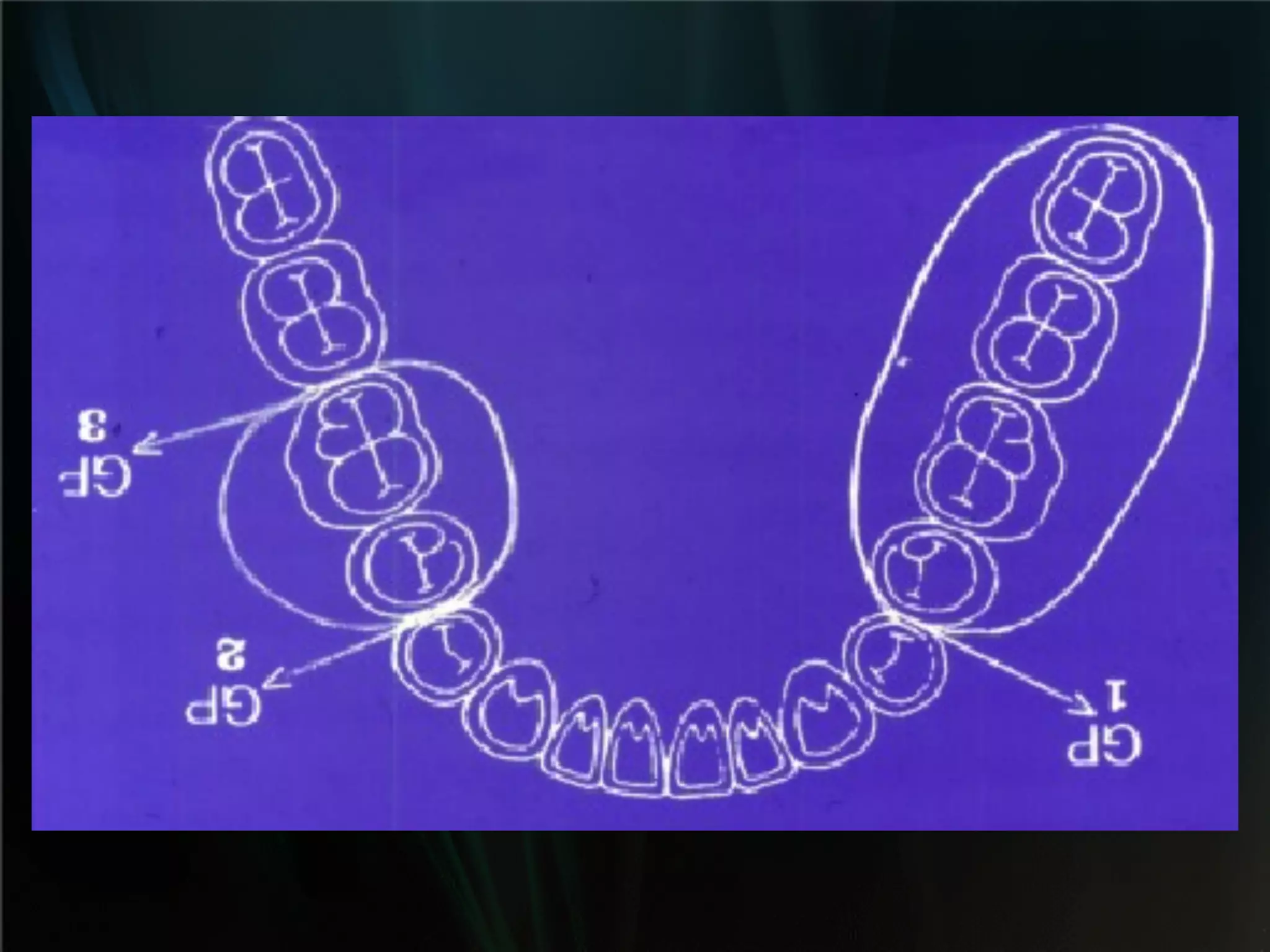
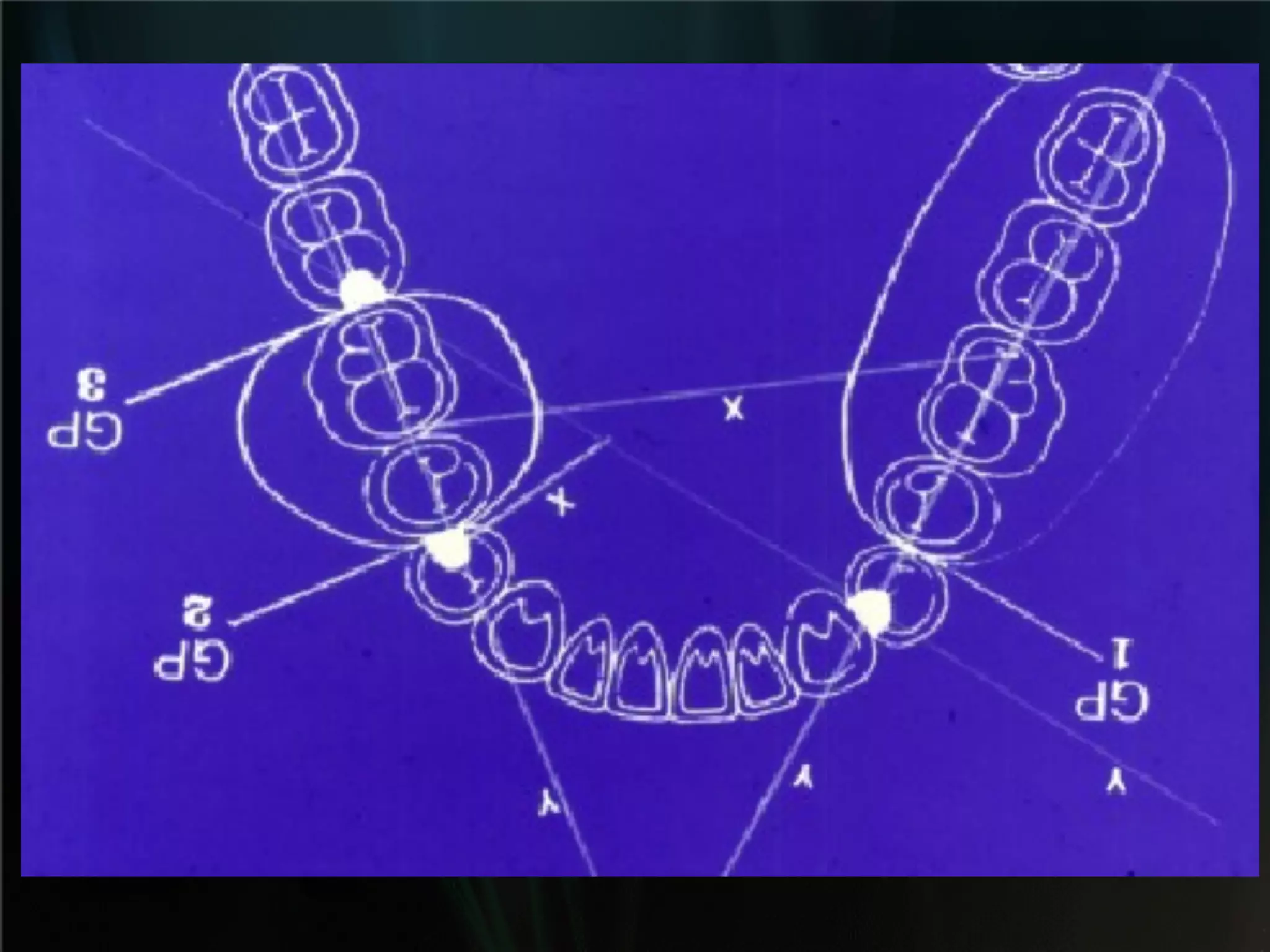
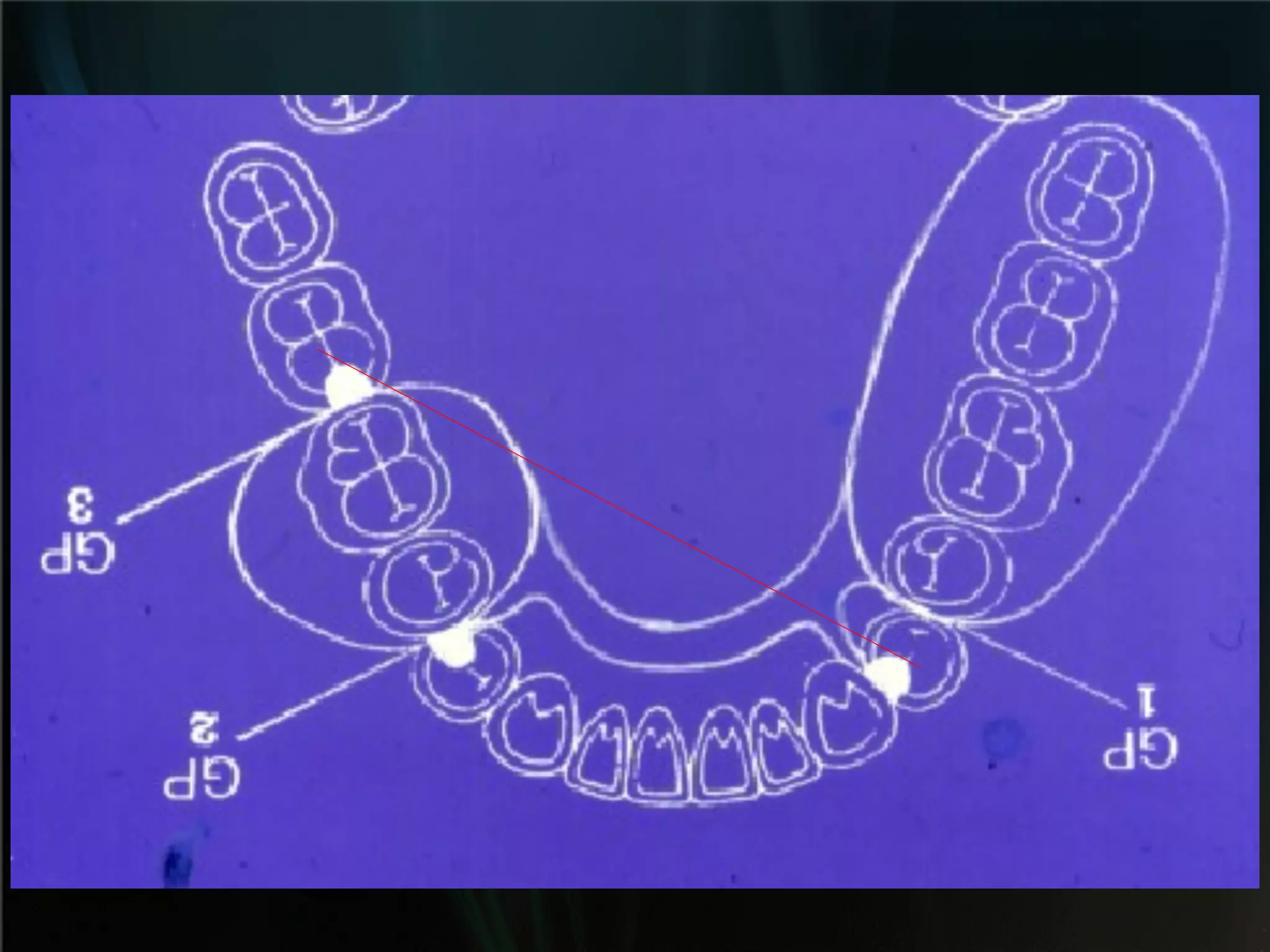
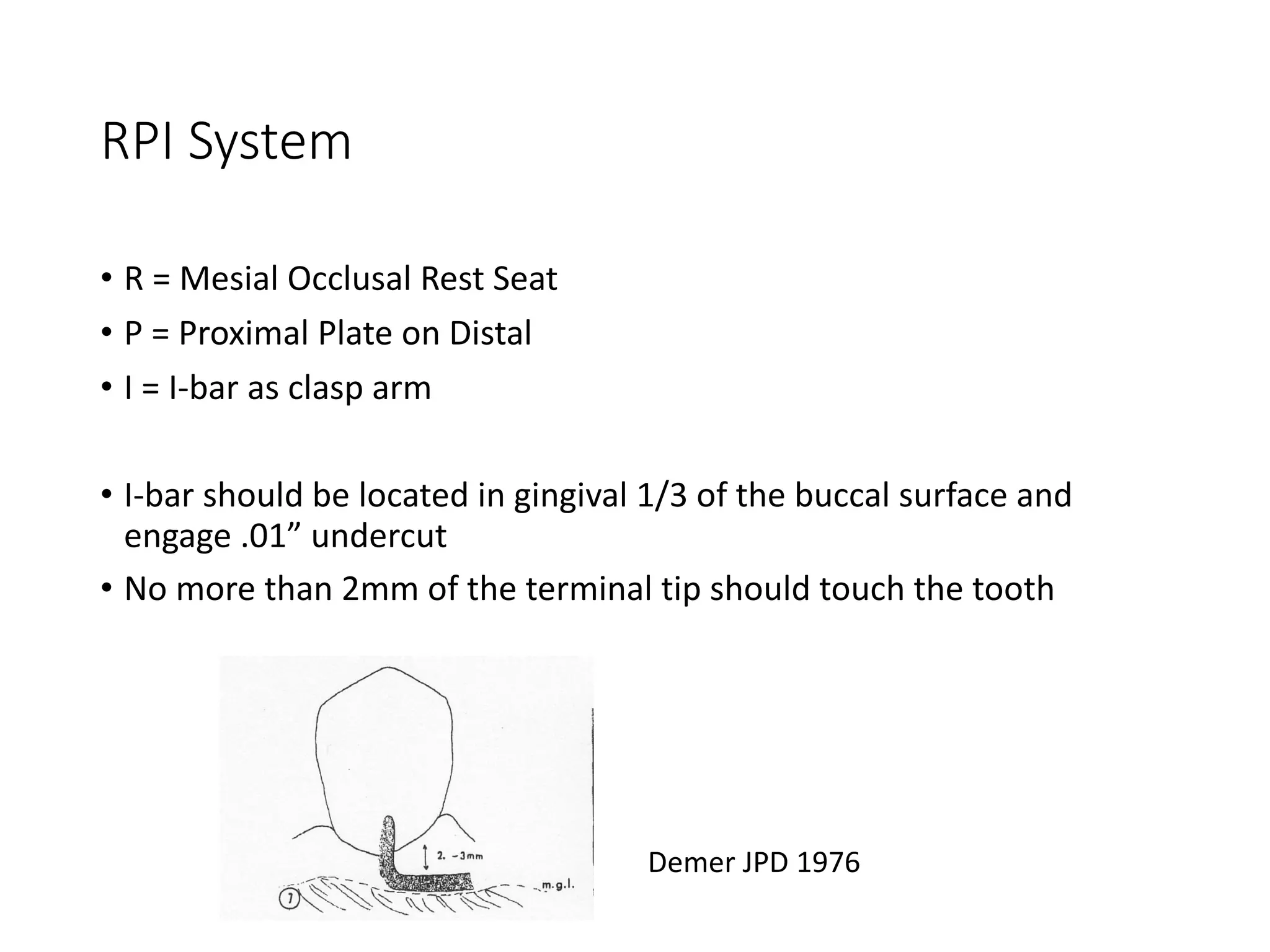
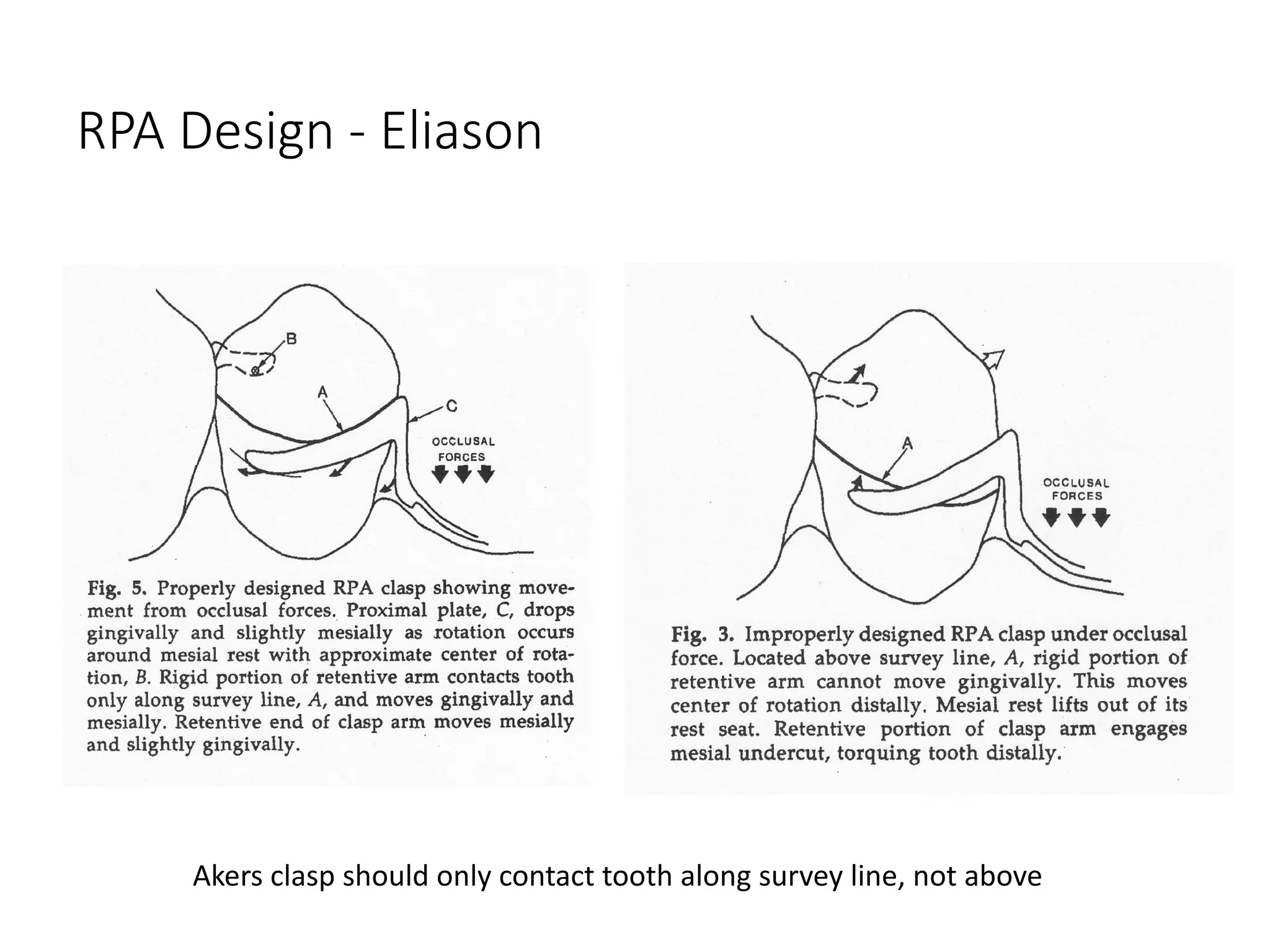
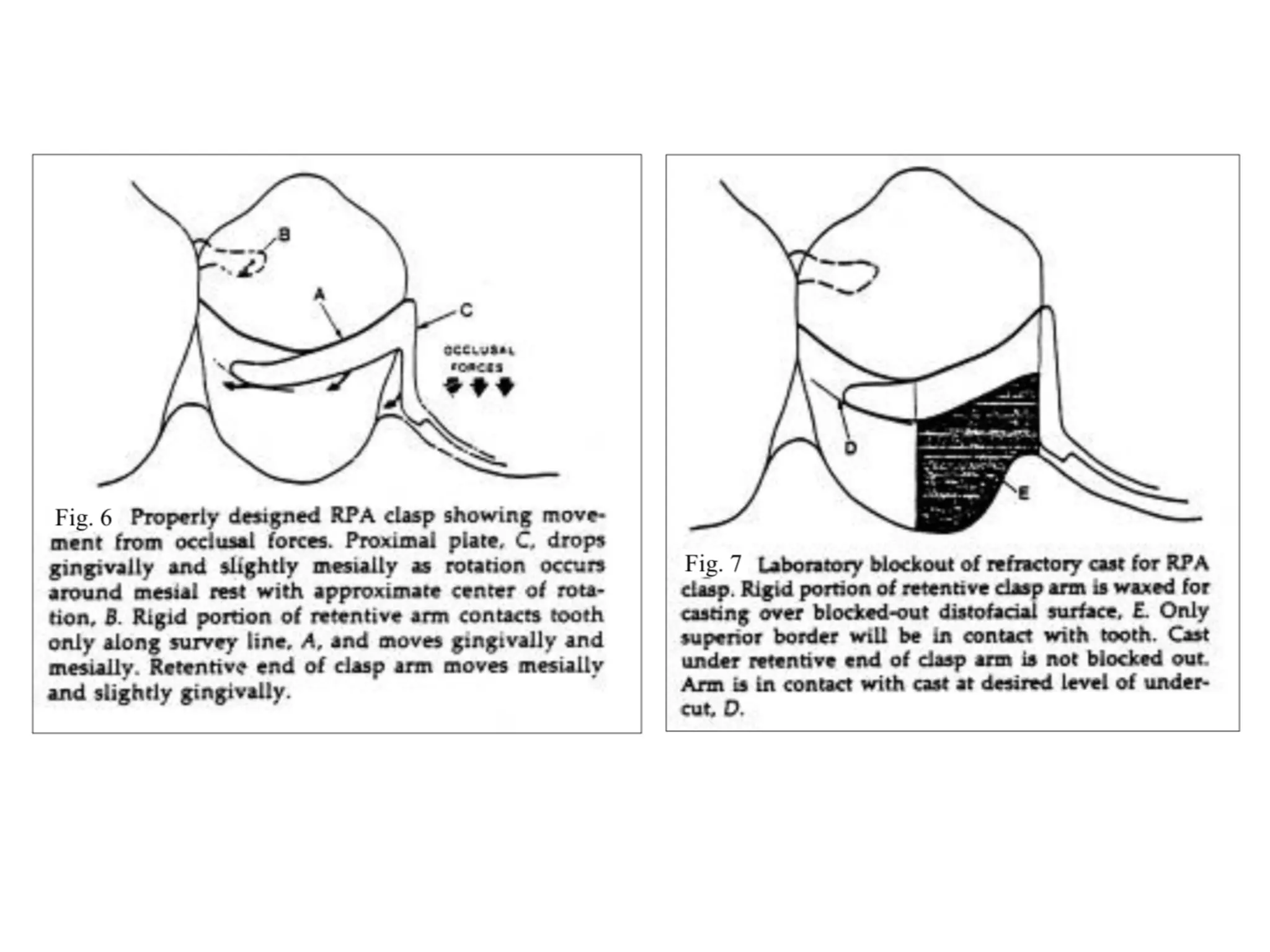
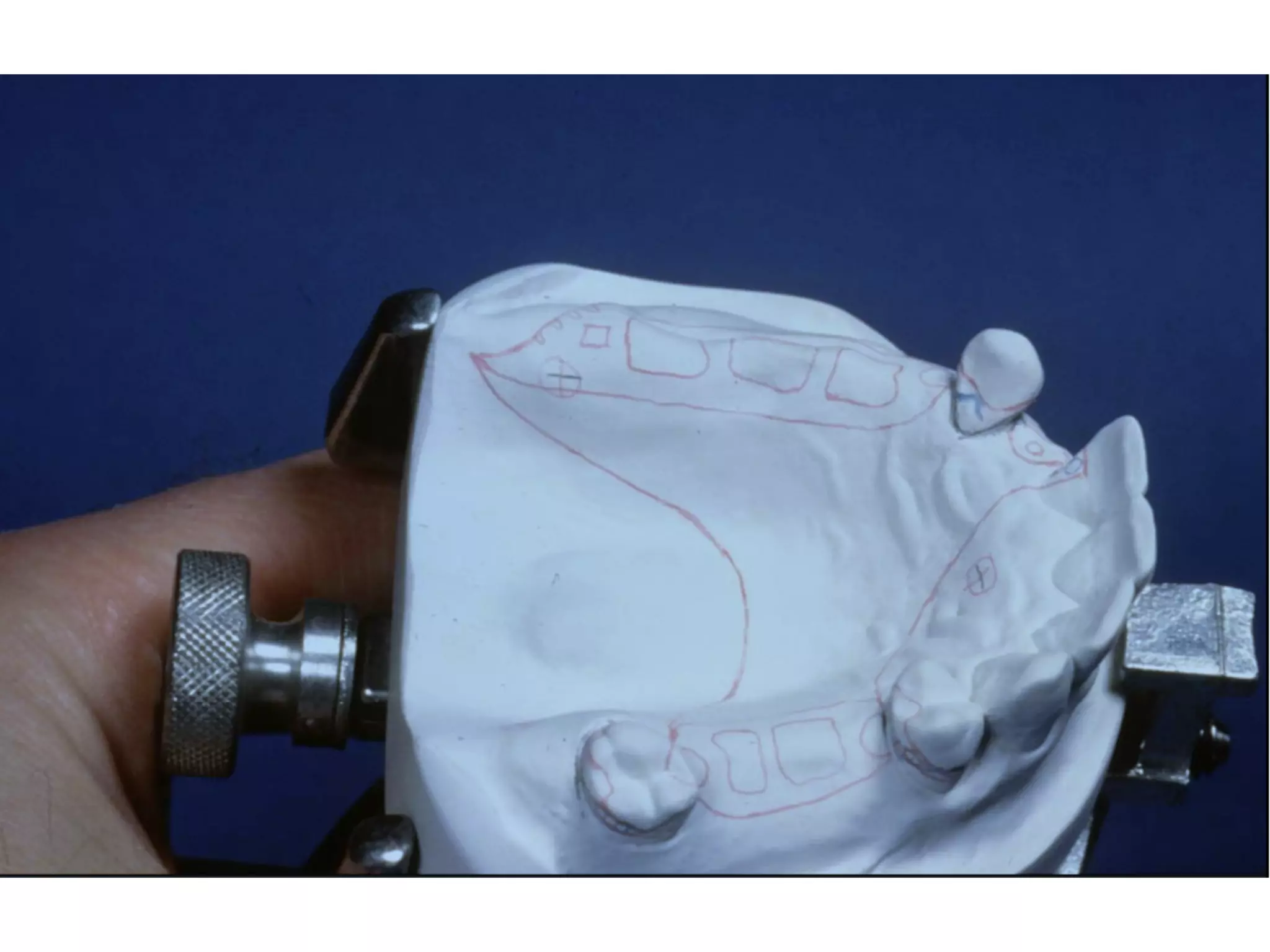
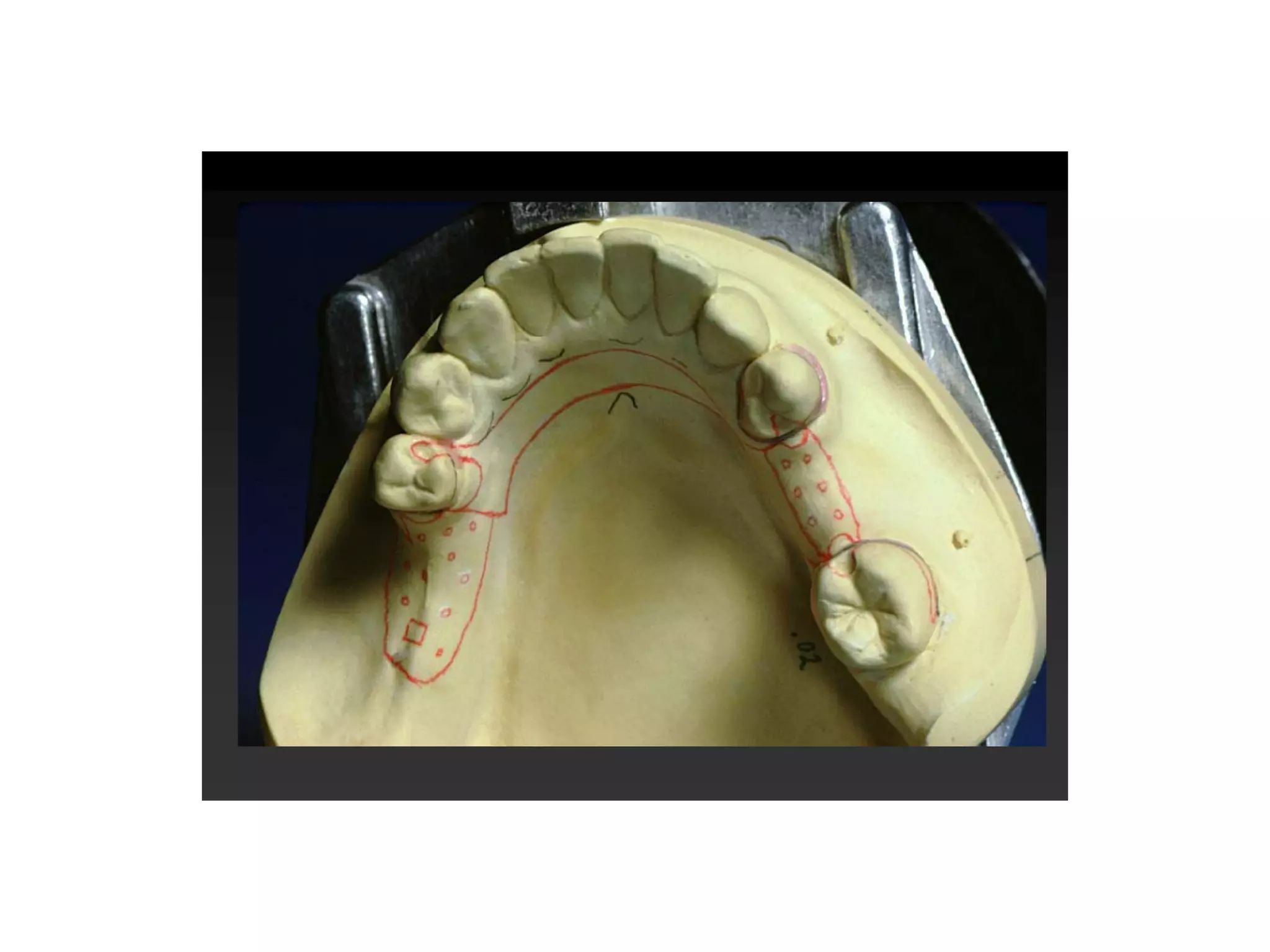
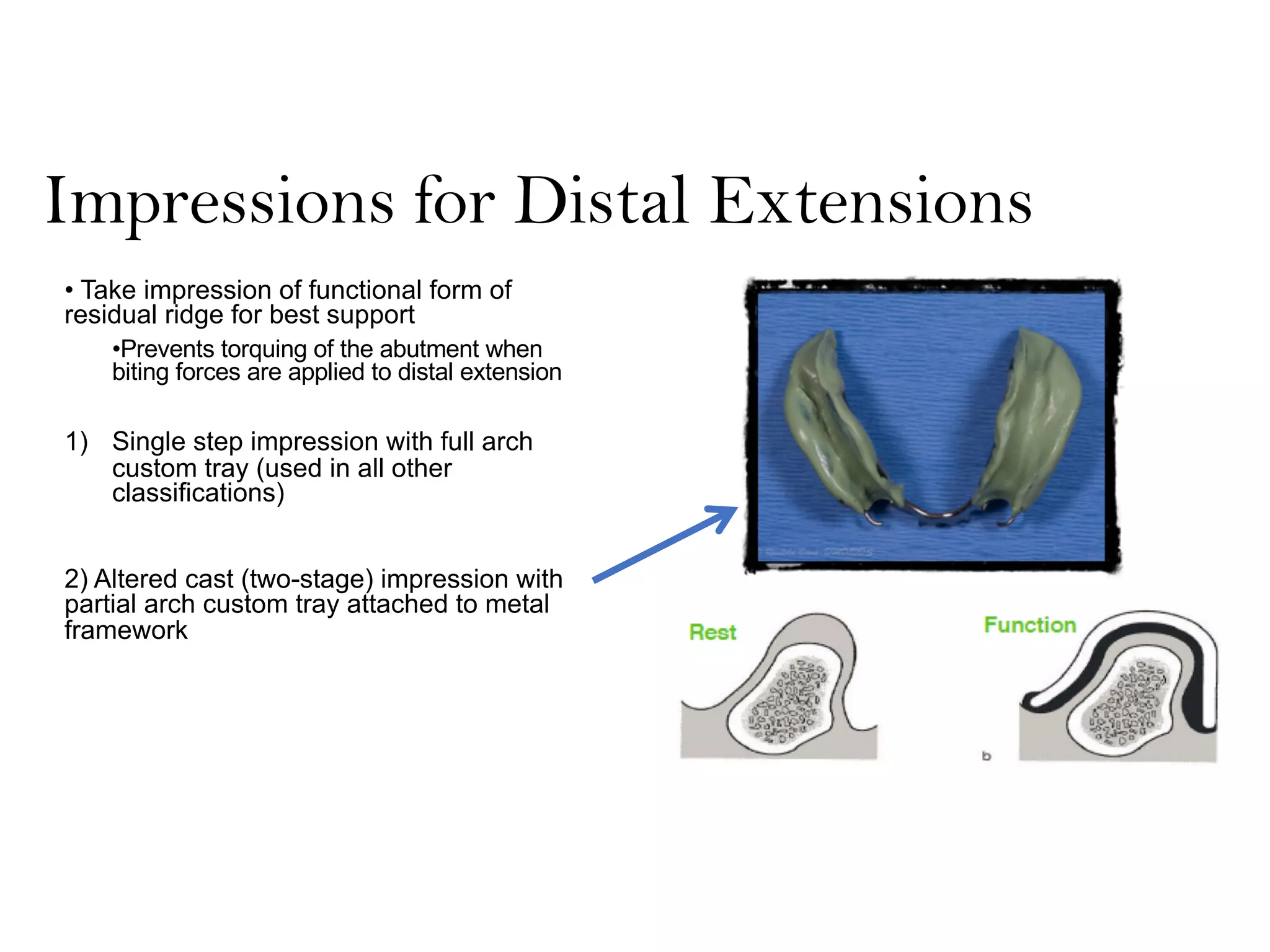
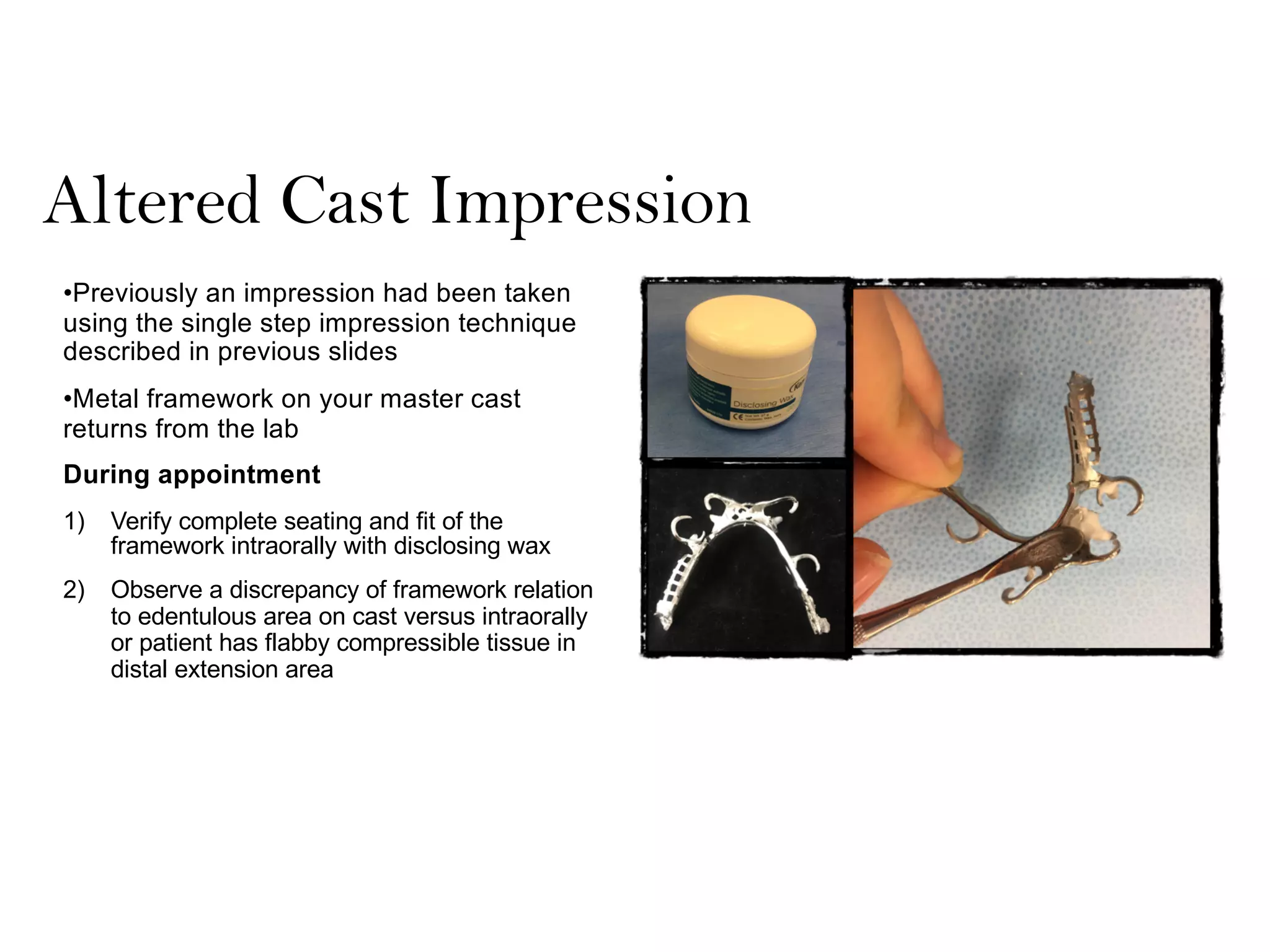
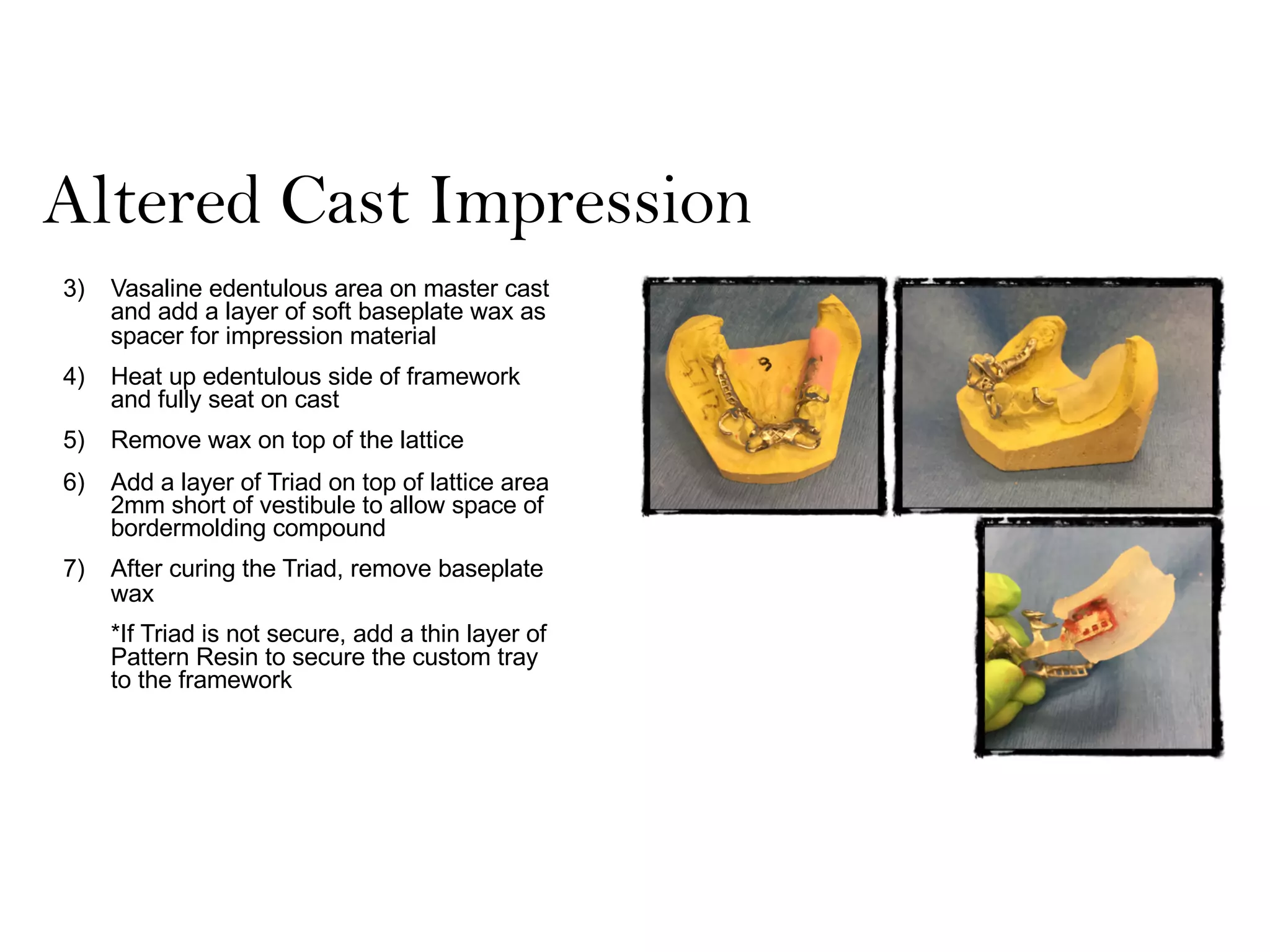
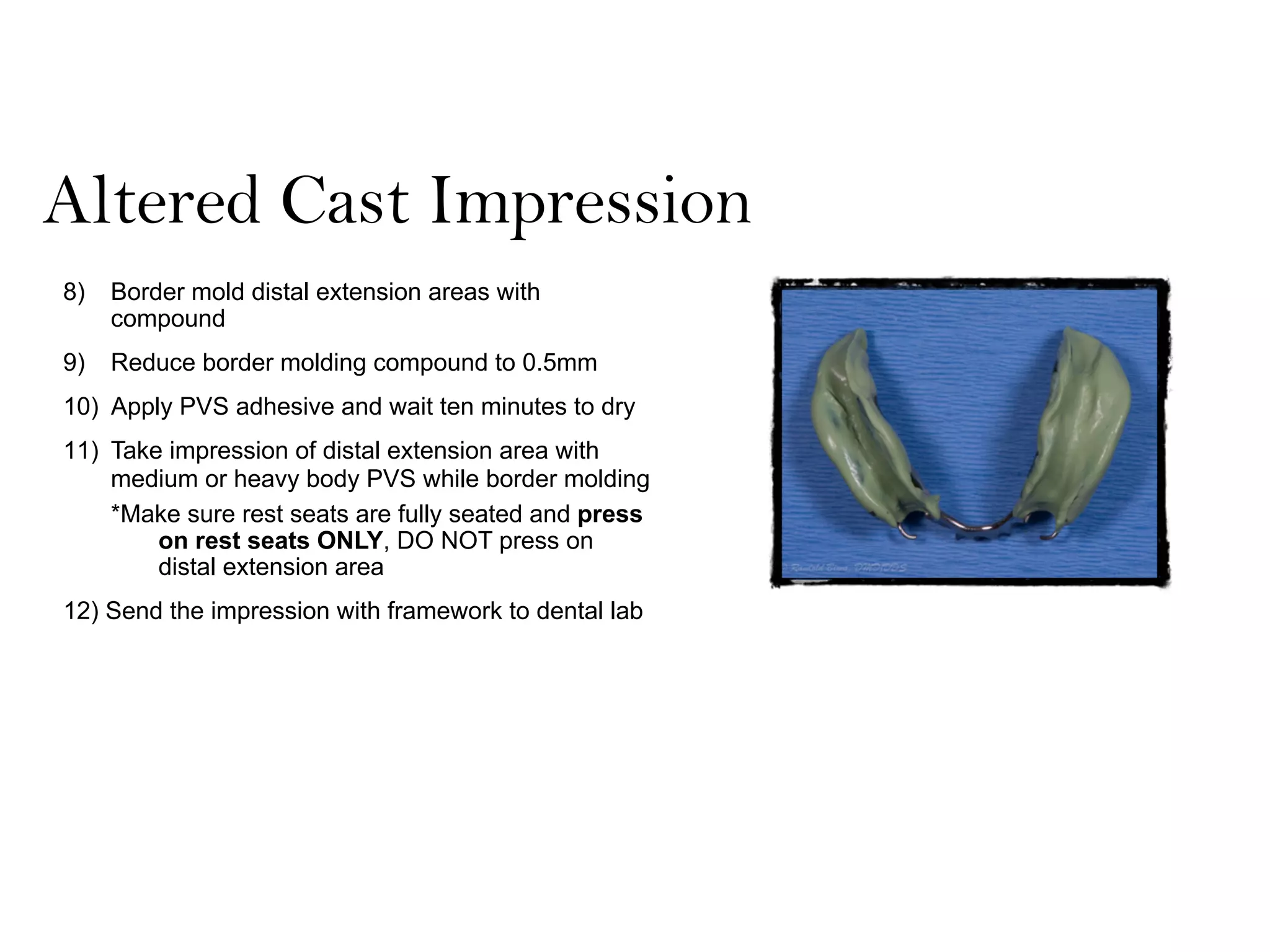
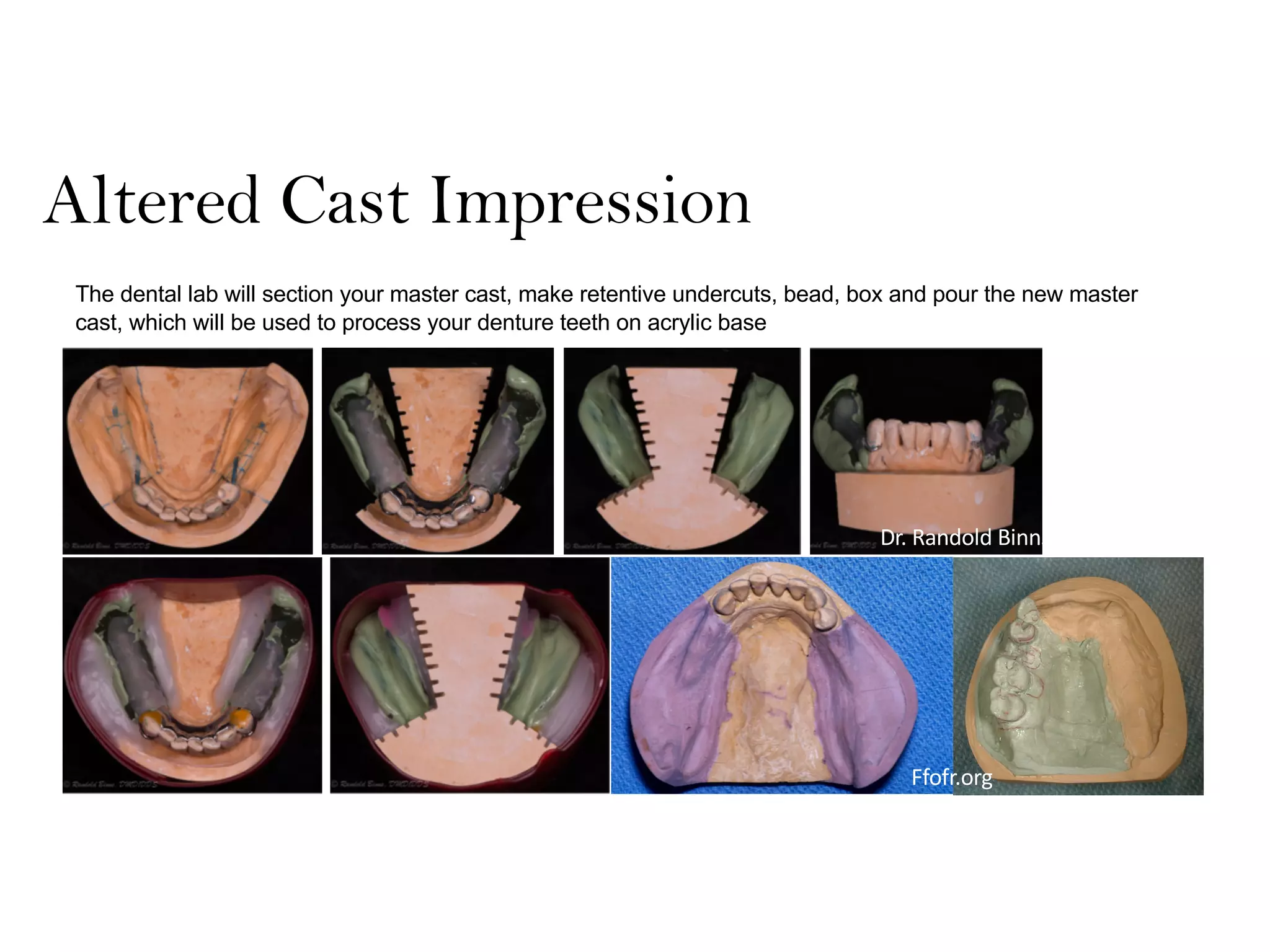
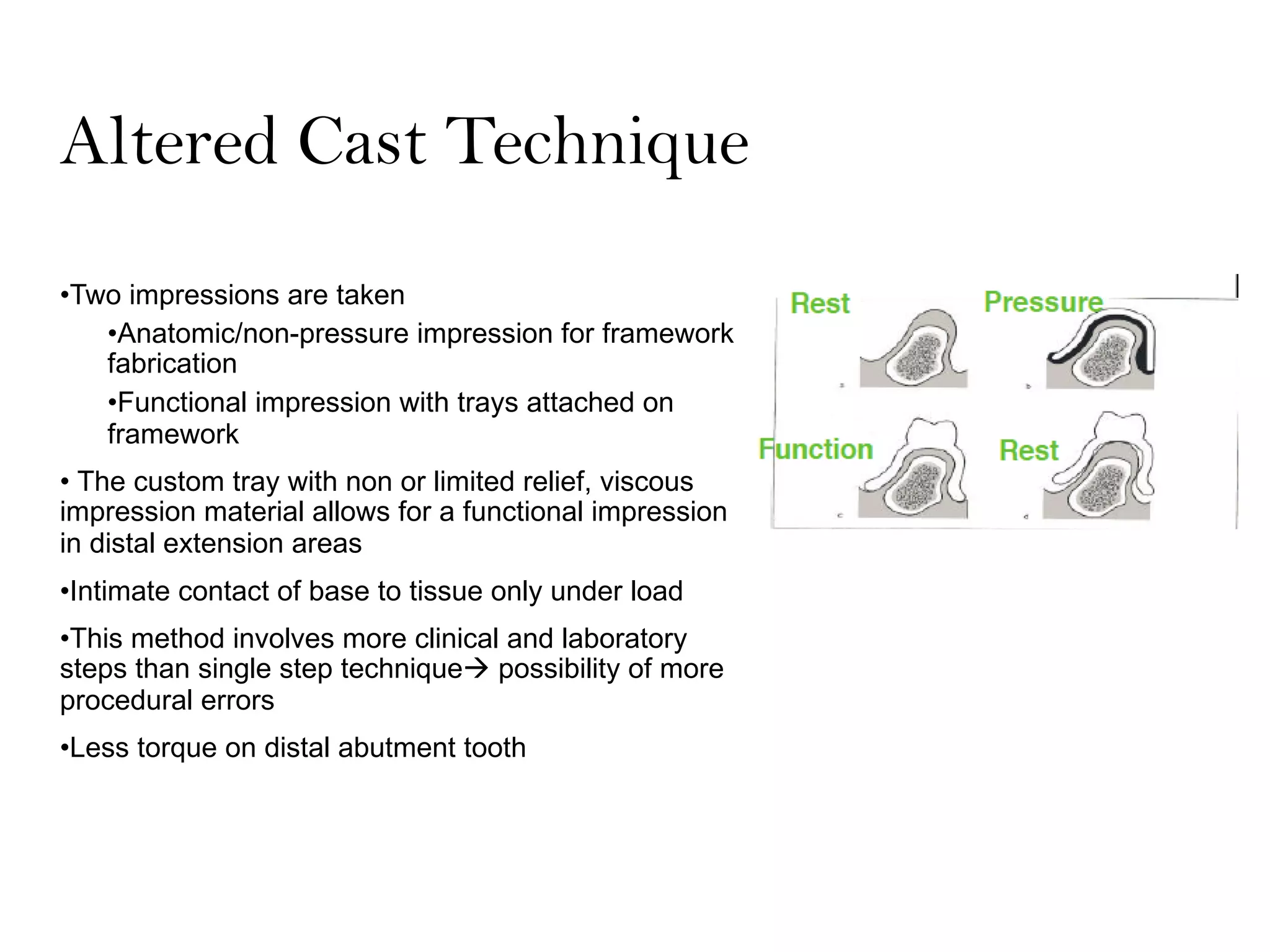
Class I and II Kennedy classification RPD cases differ in their sources of support. Class I cases rely on support from distal extension soft tissues and the primary abutment teeth, while Class II cases rely primarily on support from the abutment teeth. Due to the differential rigidity between teeth and edentulous ridges, RPDs rotate around an axis through the terminal abutments when occlusal forces are applied. Key biomechanical principles for RPD design include locating the primary axis of rotation, incorporating stress-releasing direct retainers, incorporating indirect retention, and considering support from the extension base. The altered cast technique involves border molding the distal extension for a functional impression to reduce torque on abutment teeth during