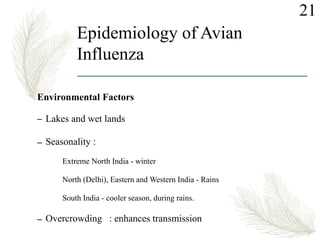
This document provides an overview of avian influenza, including its history, types, epidemiology, pathogenesis, clinical features, diagnosis, treatment, vaccination, and prevention/control. Some key points include:
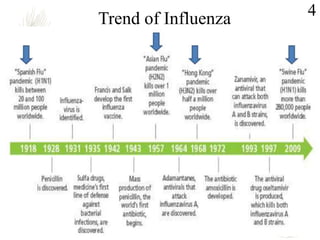
- Avian influenza was first recorded in Italy in 1878 and there have been several global pandemics, including the deadly 1918 Spanish Flu.
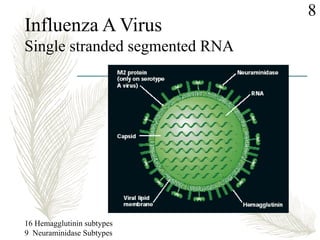
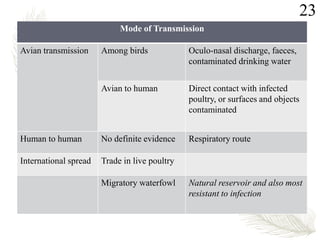
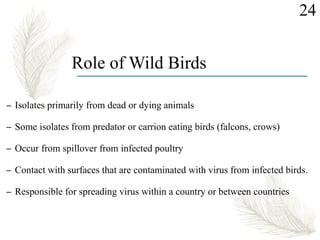
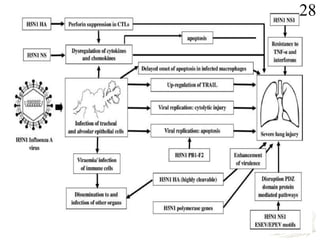
- It is caused by influenza A viruses that can infect multiple species like birds, pigs, and humans. The H5N1, H7N9, and H9N2 subtypes pose the greatest risk to humans.
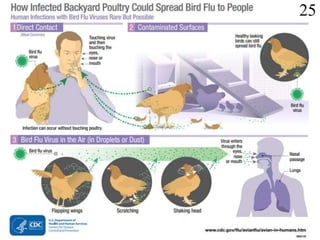
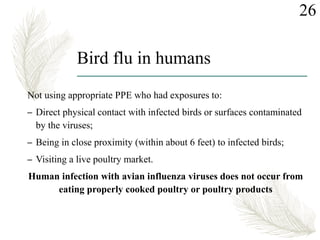
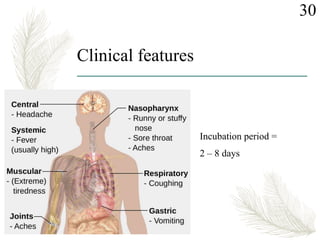
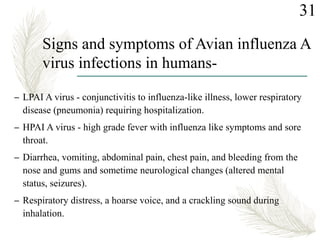
- Humans usually get infected through direct contact with infected birds or contaminated environments. Signs can range from mild to severe pneumonia and
![7Family Orthomyxoviridae
Genus Influenza virus
Types Type A Type B Type C
Sub types or
sero types
17 H and 10 N
Infect multiple species;
Human, Avian, Swine,
equine etc
No subtypes
Infect humans
No sub types
Infect humans
and pigs
Public Health
Importance
Causes Pandemics
Spanish Flu [A (H1N1)]
1918-19;
Asian Flu [A (H2N2)]
1957-59;
Hongkong Flu
[A (H3N2)] 1968-68;
“Swine Flu”
[A (H1N1)] 2009-10
Causes Epidemics,
seasonal Influenza
outbreaks and sporadic
cases.
Causes
Epidemics
Seasonal
Influenza
Causes mild
respiratory
disease
Does not Cause
epidemic](https://image.slidesharecdn.com/avianinfluenza-180908152055/85/Avian-influenza-7-320.jpg)



![1. Information on Avian influenza [online]. 2017April 13 [cited 2018 feb 02]; Available
from: URL :https://www.cdc.gov/flu/avianflu/index.htm
2. Influenza (avian and other zoonotic) [online]. 2018 [cited 2018 feb 02]; Available
from: URL : http://www.who.int/mediacentre/factsheets/avian_influenza/en/
3. Influenza [online]. 2018 [cited 2018 feb 02]; Available from: URL :
http://www.who.int/influenza/human_animal_interface/en/
4. Avian Influenza in India [online]. 2009 [cited 2018 feb 02]; Available from: URL :
H5N8 Avian Influenza in India | HealthMap.
http://www.healthmap.org/site/diseasedaily/article/h5n8-avian-influenza-india-
113016
5. Analysis of recent scientific information on avian influenza A(H7N9) virus [online].
2017 feb 10 [cited 2018 feb 02]; Available from: URL : 04/02/2018 WHO | Analysis
of recent scientific information on avian influenza A(H7N9) virus
http://www.who.int/influenza/human_animal_interface/avian_influenza/riskassessme
nt_AH7N9_201702/en/
6. How Infected Backyard Poultry Could Spread Bird Flu to People [online]. 2017 feb
10 [cited 2018 feb 04]; Available from: URL :
https://www.cdc.gov/flu/pdf/avianflu/avian-flu-transmission.pdf
66References](https://image.slidesharecdn.com/avianinfluenza-180908152055/85/Avian-influenza-64-320.jpg)