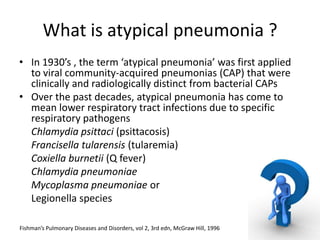
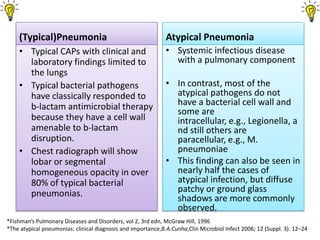
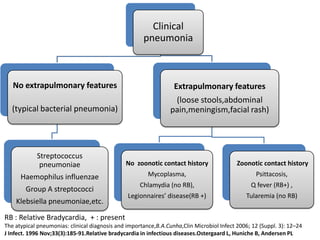
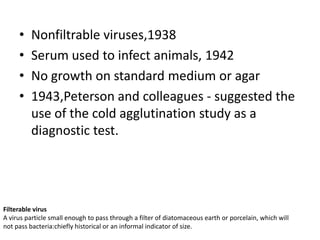
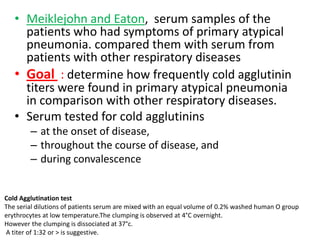
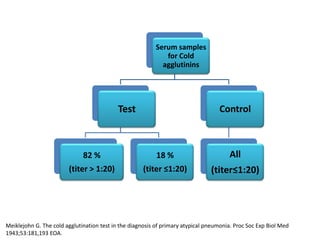
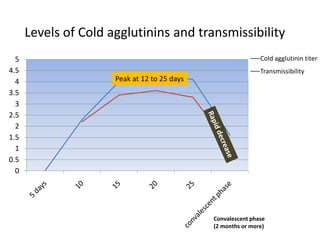
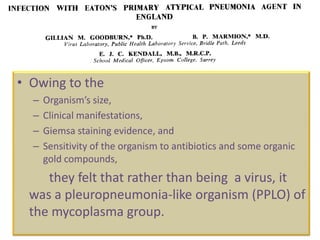
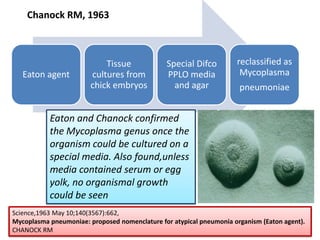
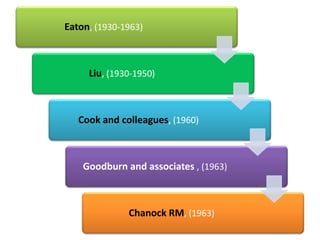
Atypical pneumonia refers to pneumonia caused by certain atypical pathogens rather than typical bacteria. In the 1930s, pneumonia cases emerged that were clinically distinct from bacterial pneumonia. Over decades, research identified the pathogens responsible as Chlamydia, Legionella, and Mycoplasma species. Through the 1930s-1960s, scientists like Eaton, Liu, and Chanock used techniques like cold agglutination testing, animal inoculation and staining to determine that Mycoplasma pneumoniae was the causative agent of the majority of atypical pneumonia cases, which they named the Eaton agent. This resolved the nature of the atypical pneumonia-causing organism.