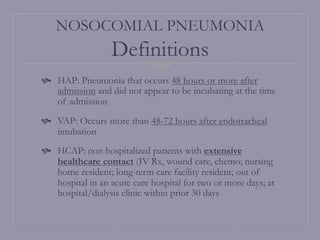
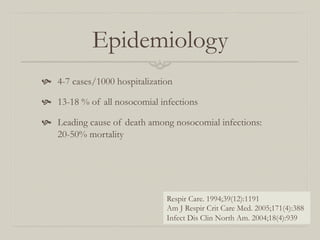
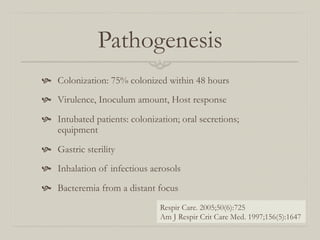
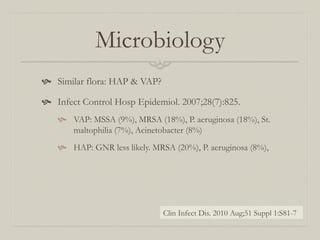
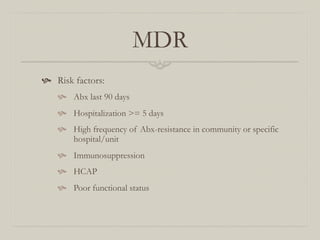
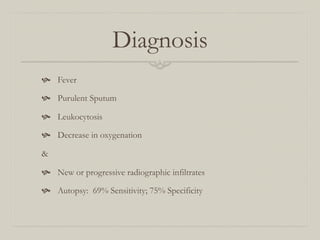
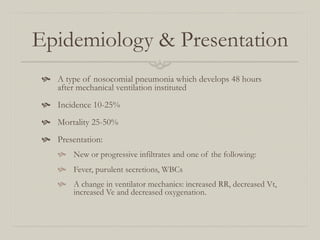
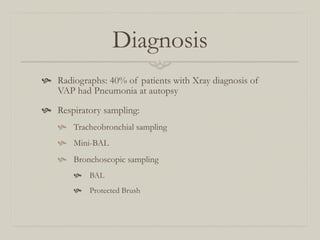
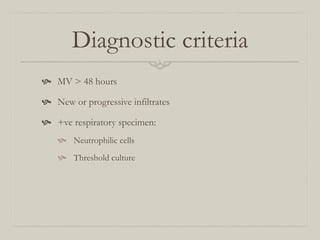
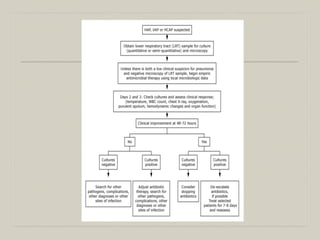
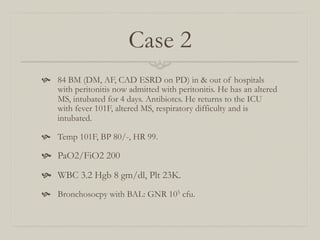
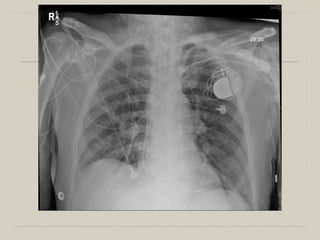
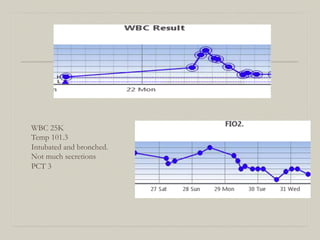
This patient likely has nosocomial pneumonia (either HAP or VAP) secondary to his multiple hospital admissions and prolonged intubation. He presents with fever, altered mental status, and respiratory distress - consistent with pneumonia. Given his multiple comorbidities and ESRD, he is high risk for poor outcomes. Broad spectrum antibiotics and further diagnostic workup are indicated.