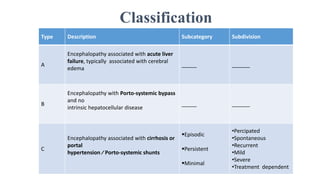
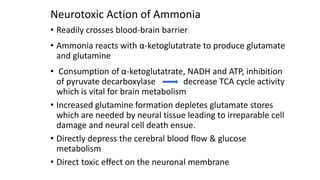
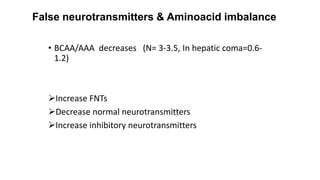
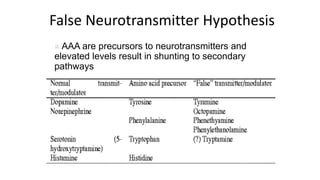
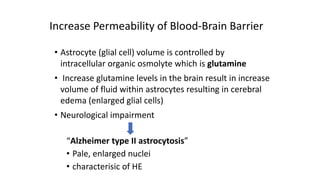
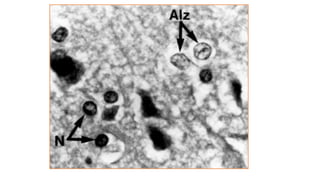
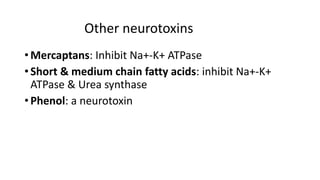
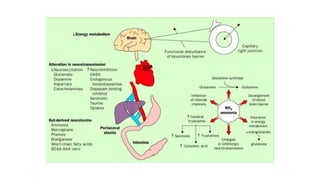
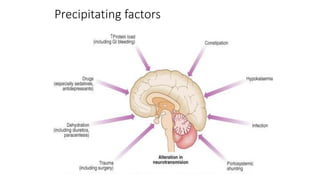
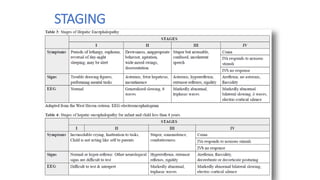
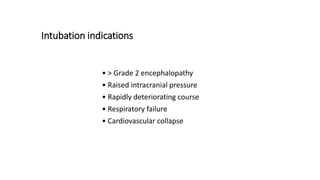
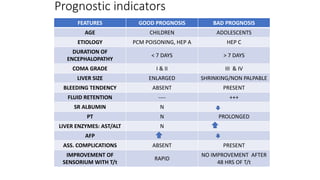
Hepatic encephalopathy (HE) is a neuropsychiatric disorder occurring in patients with liver dysfunction, classified into subcategories based on underlying conditions. The pathogenesis of HE involves mechanisms including ammonia toxicity and neurotransmitter imbalance, requiring careful management strategies like fluid regulation, glucose administration, and potential use of antibiotics or lactulose. Prognosis is influenced by factors such as age, duration of encephalopathy, and degree of liver function impairment.