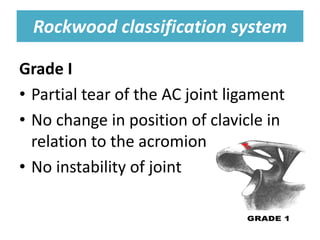
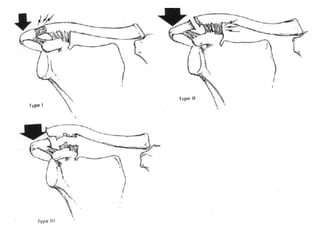
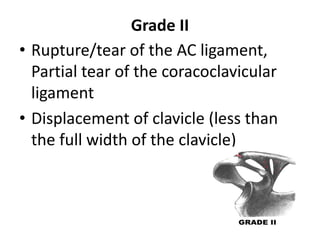
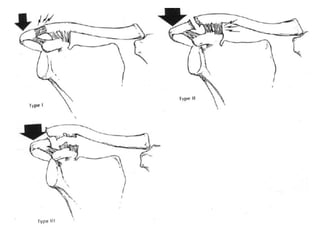
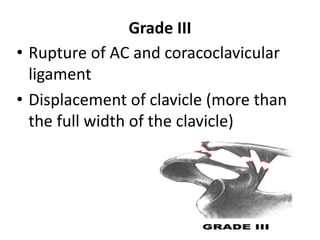
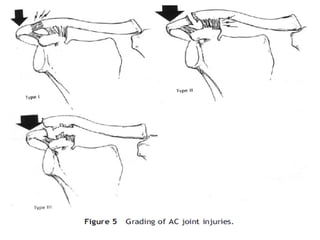
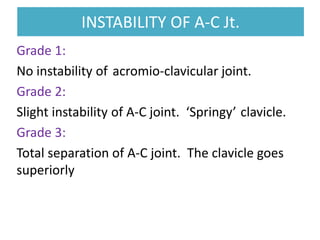
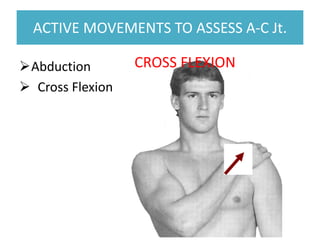
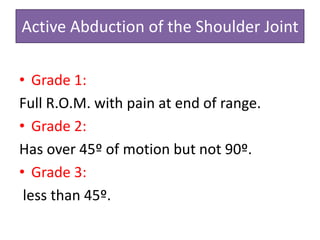
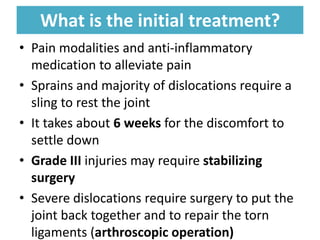
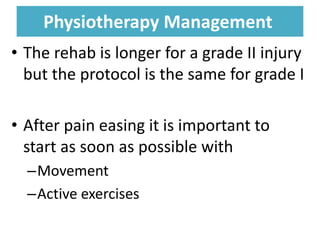
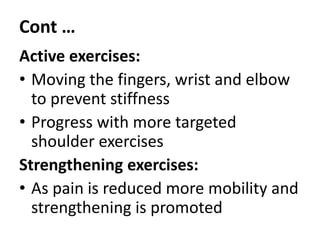
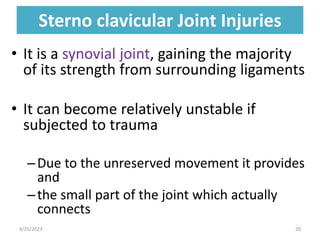
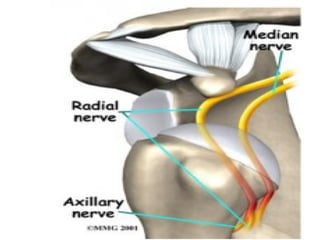
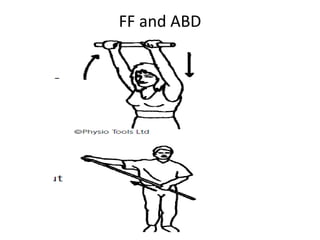
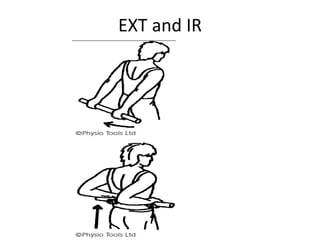
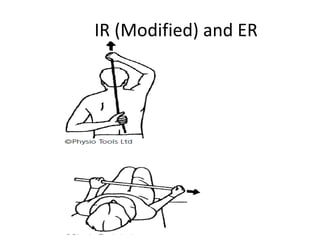
This document discusses disorders of the acromioclavicular (AC), sternoclavicular (SC), and glenohumeral (GH) joints. It describes common conditions like AC joint dislocation and arthritis. It also discusses signs, risk factors, classifications systems, treatments, and physiotherapy management for AC joint disorders. For SC joint injuries, it outlines signs, causes, and treatments. Finally, it provides details on shoulder dislocation types, diagnostic procedures, conservative and surgical management, and physiotherapy rehabilitation protocols.