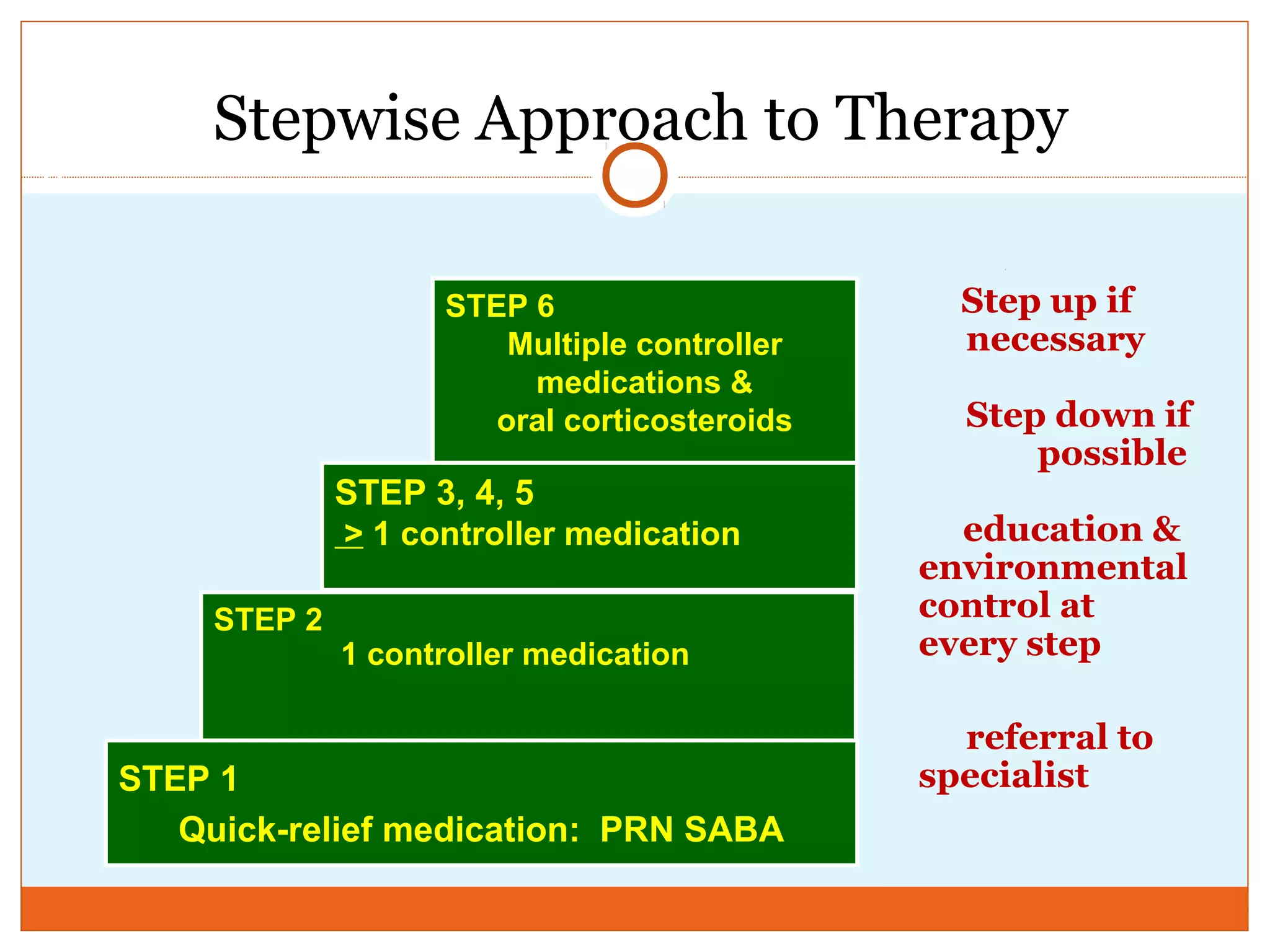
This document discusses asthma, including its definition, pathophysiology, triggers, diagnosis, and treatment. Some key points:
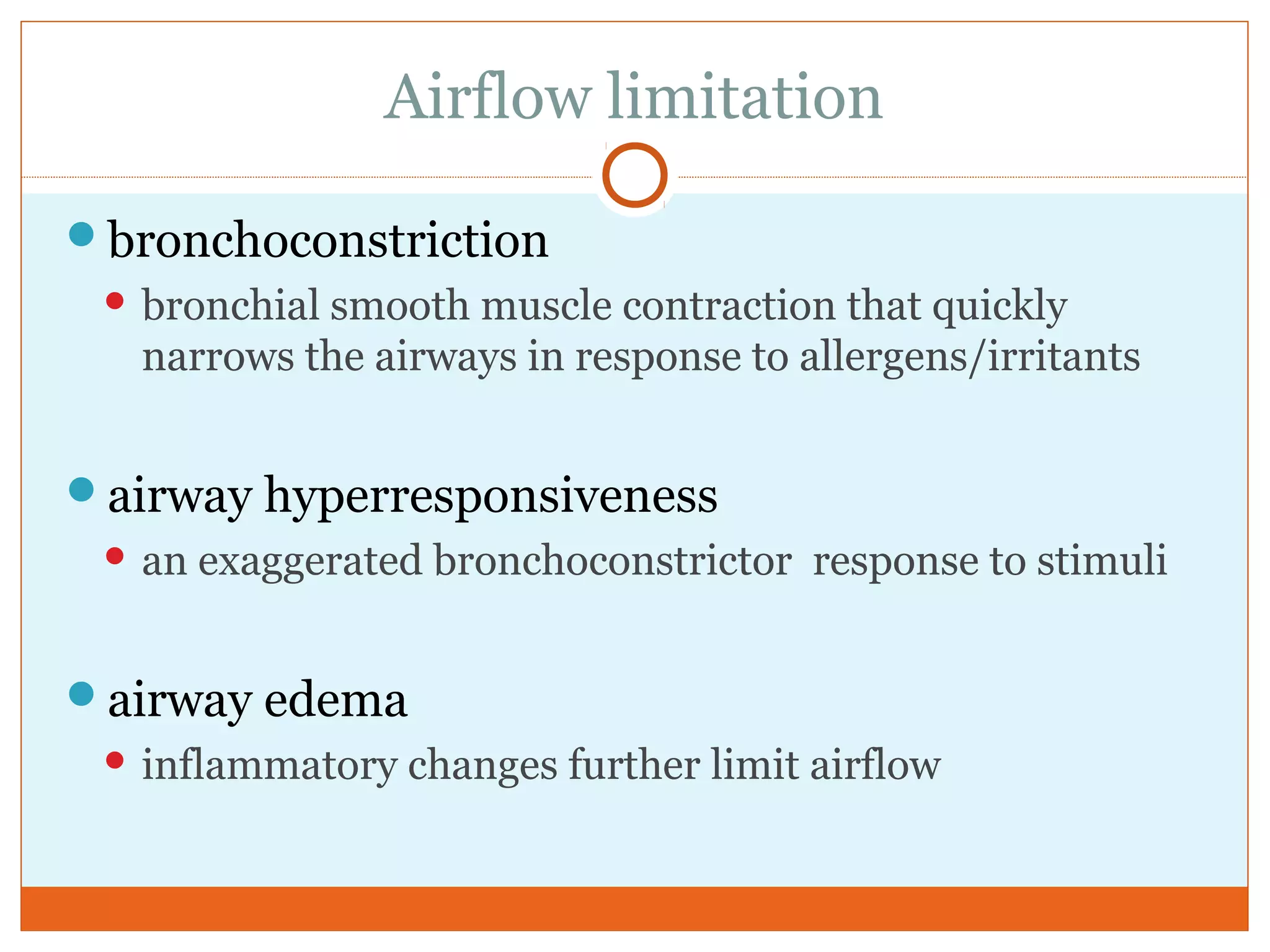
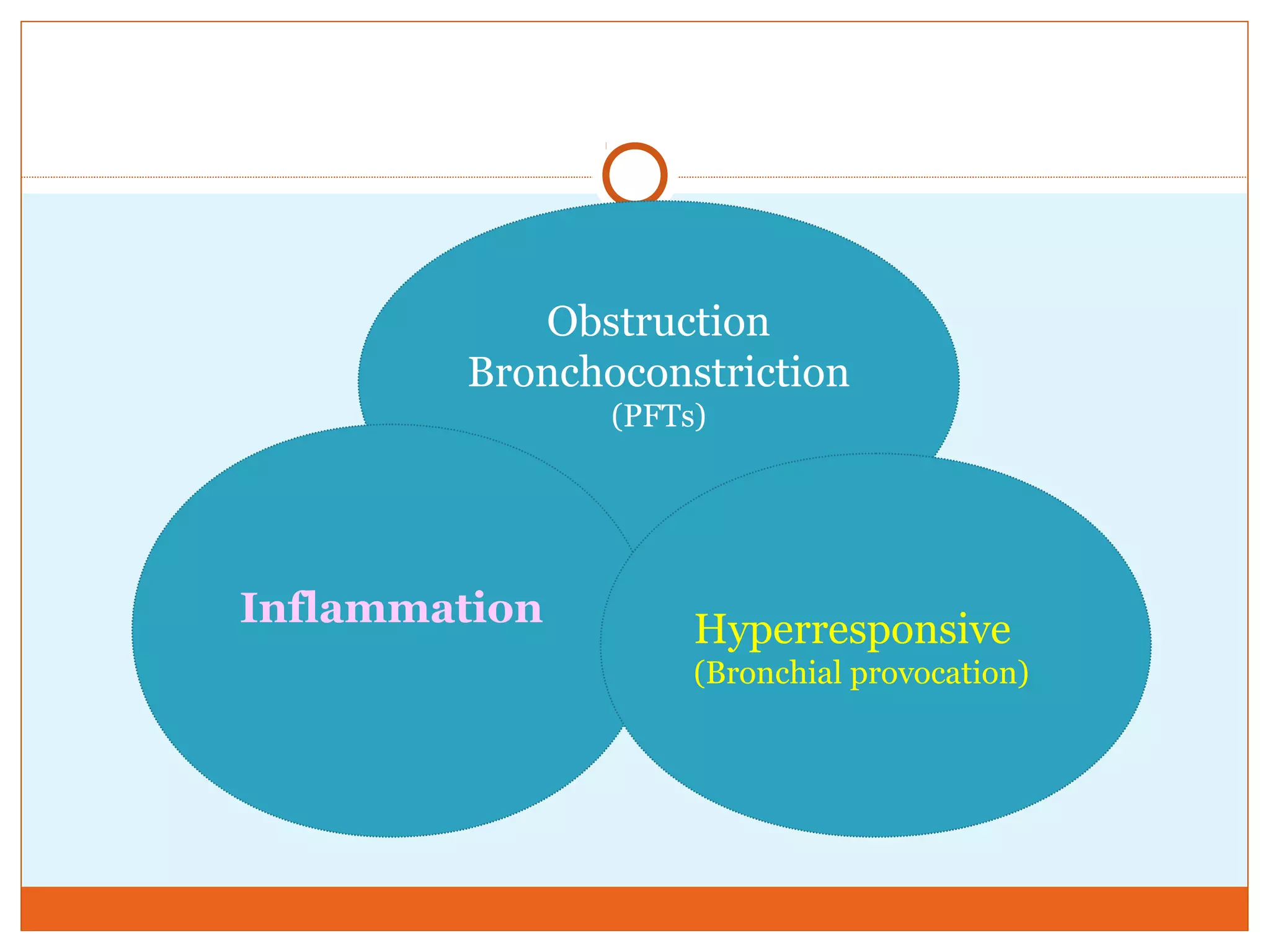
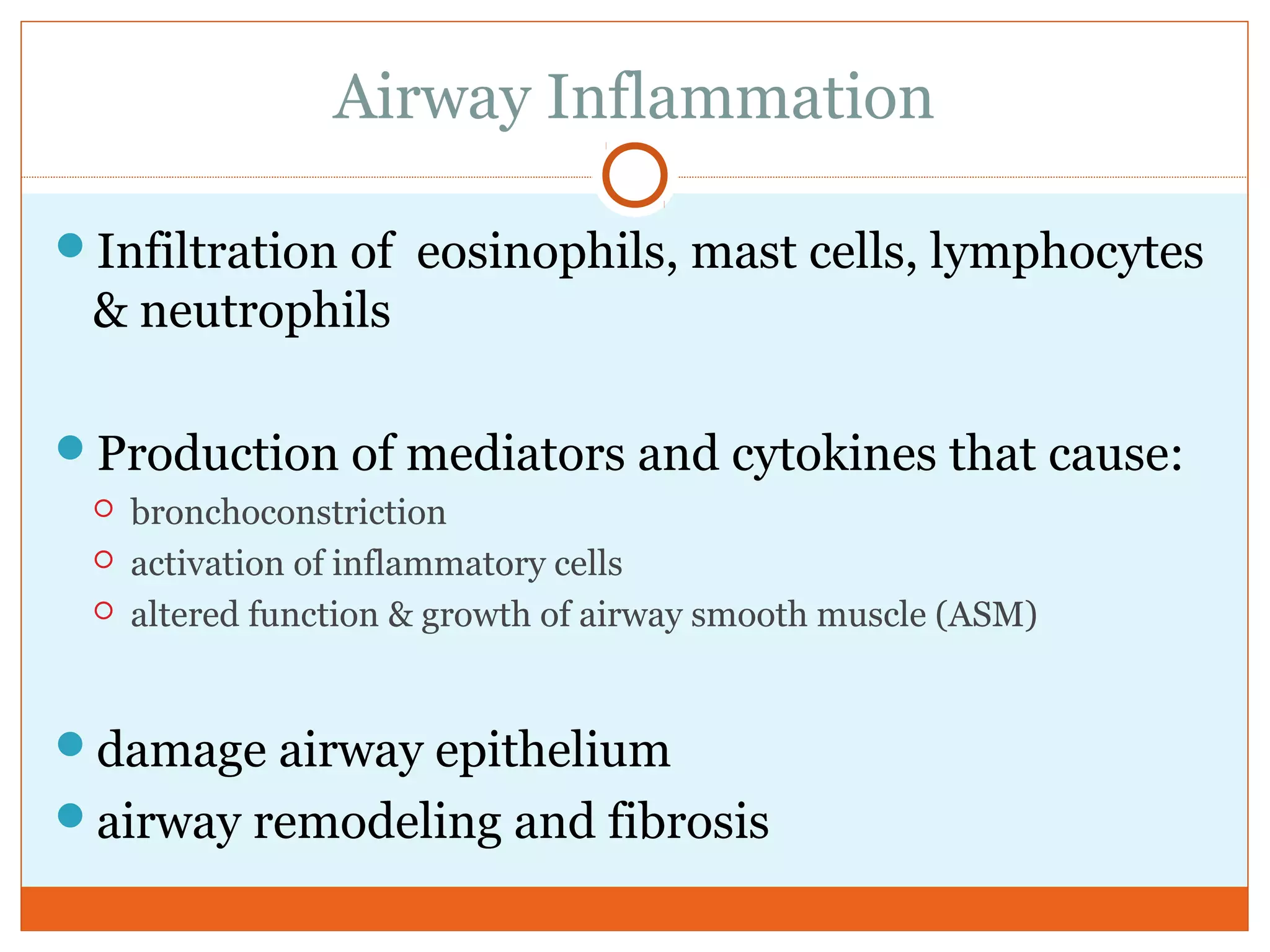
- Asthma is a chronic inflammatory disease of the airways characterized by reversible airflow obstruction.
- It affects over 25 million Americans and its prevalence has been increasing since the 1980s.
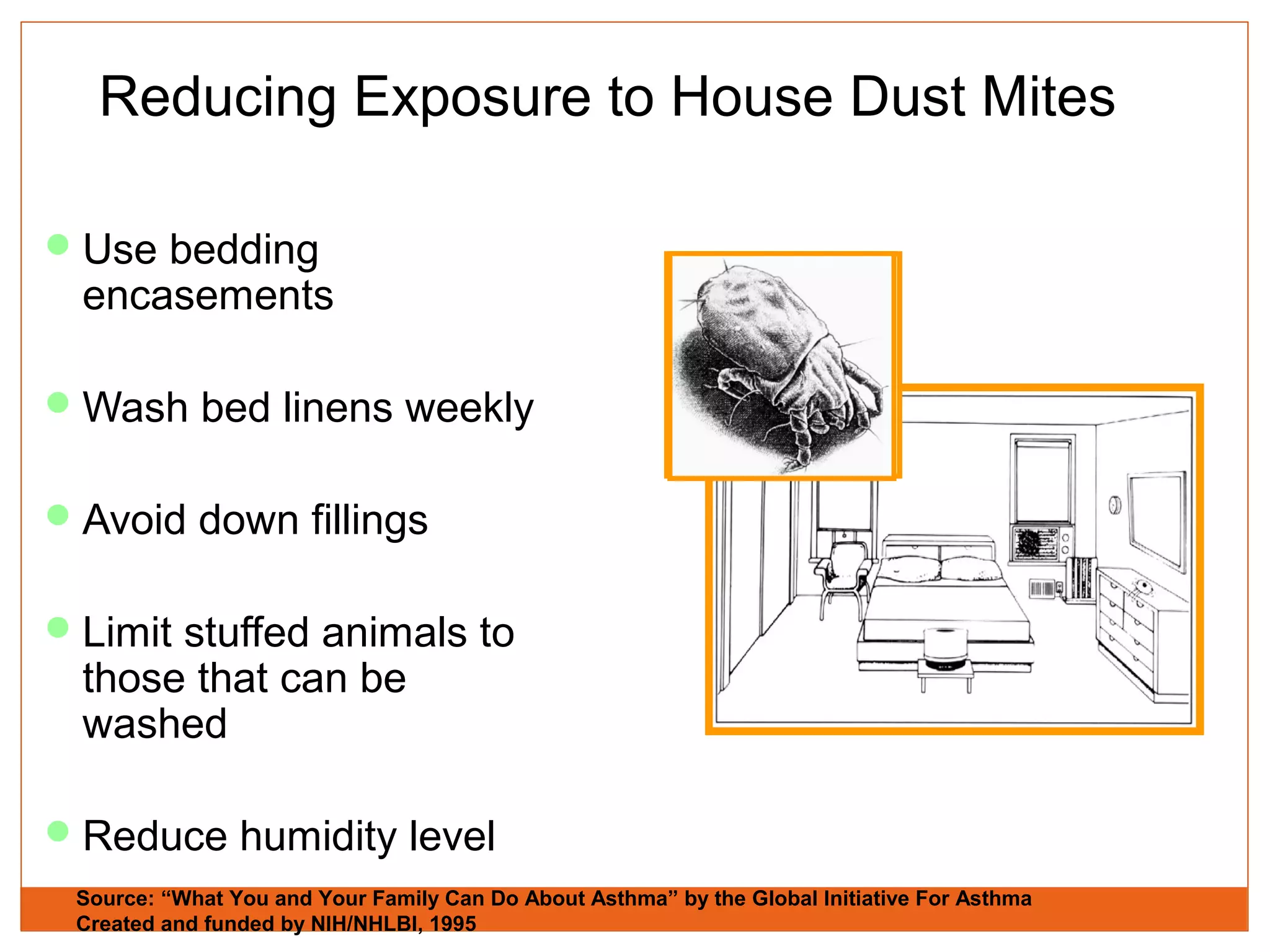
- Asthma can be triggered by allergens, viruses, exercise, weather, irritants and other factors.
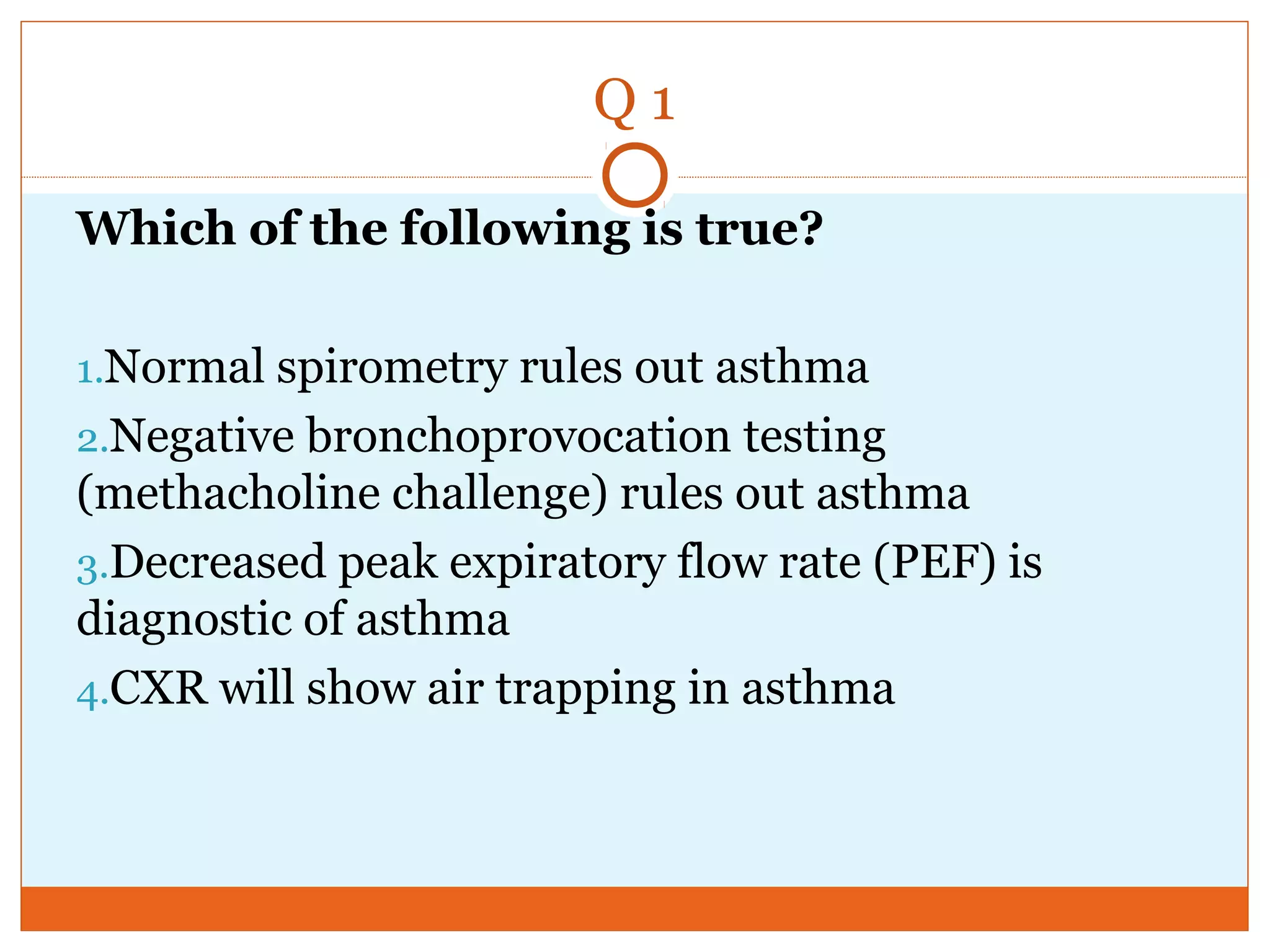
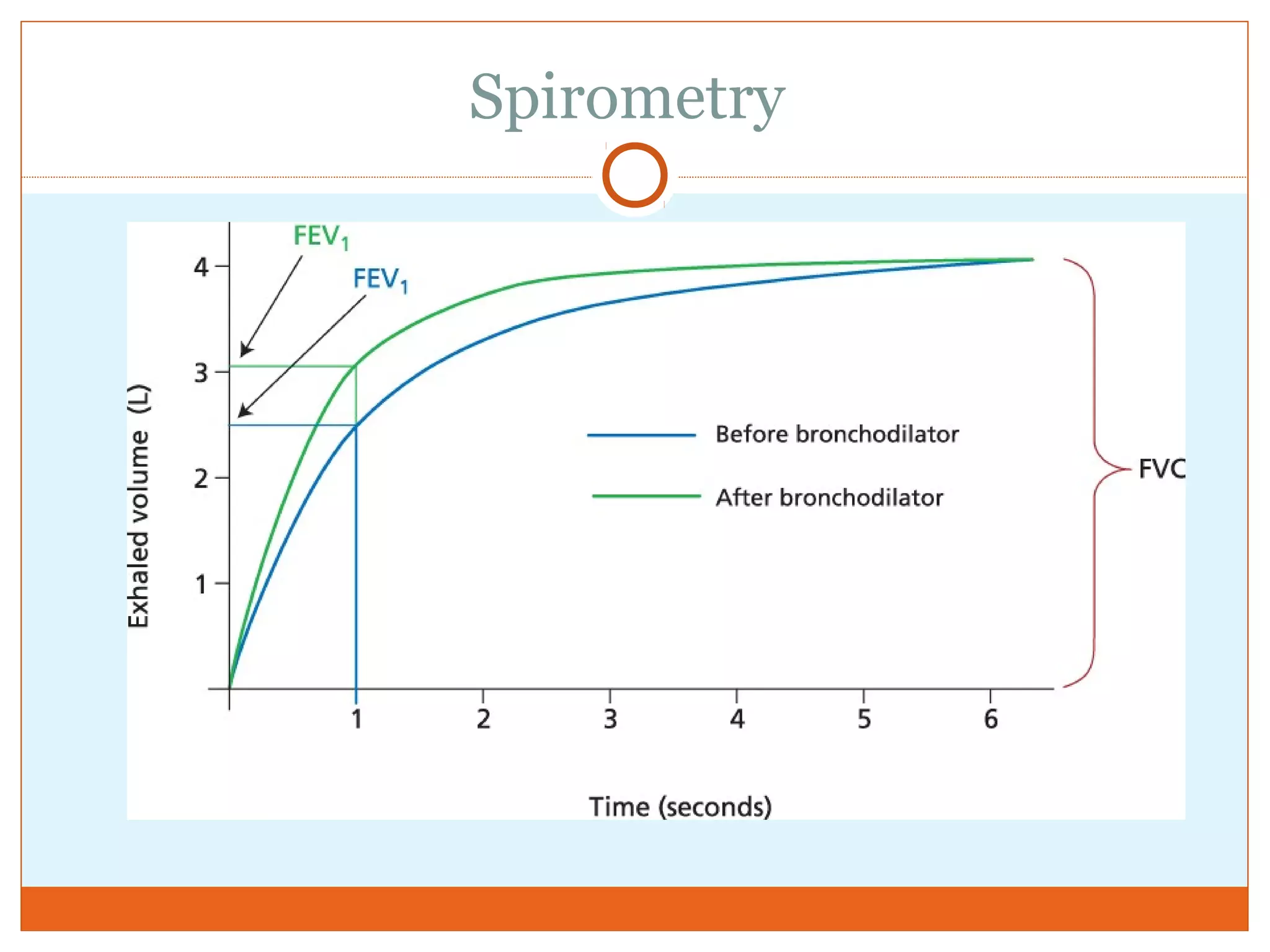
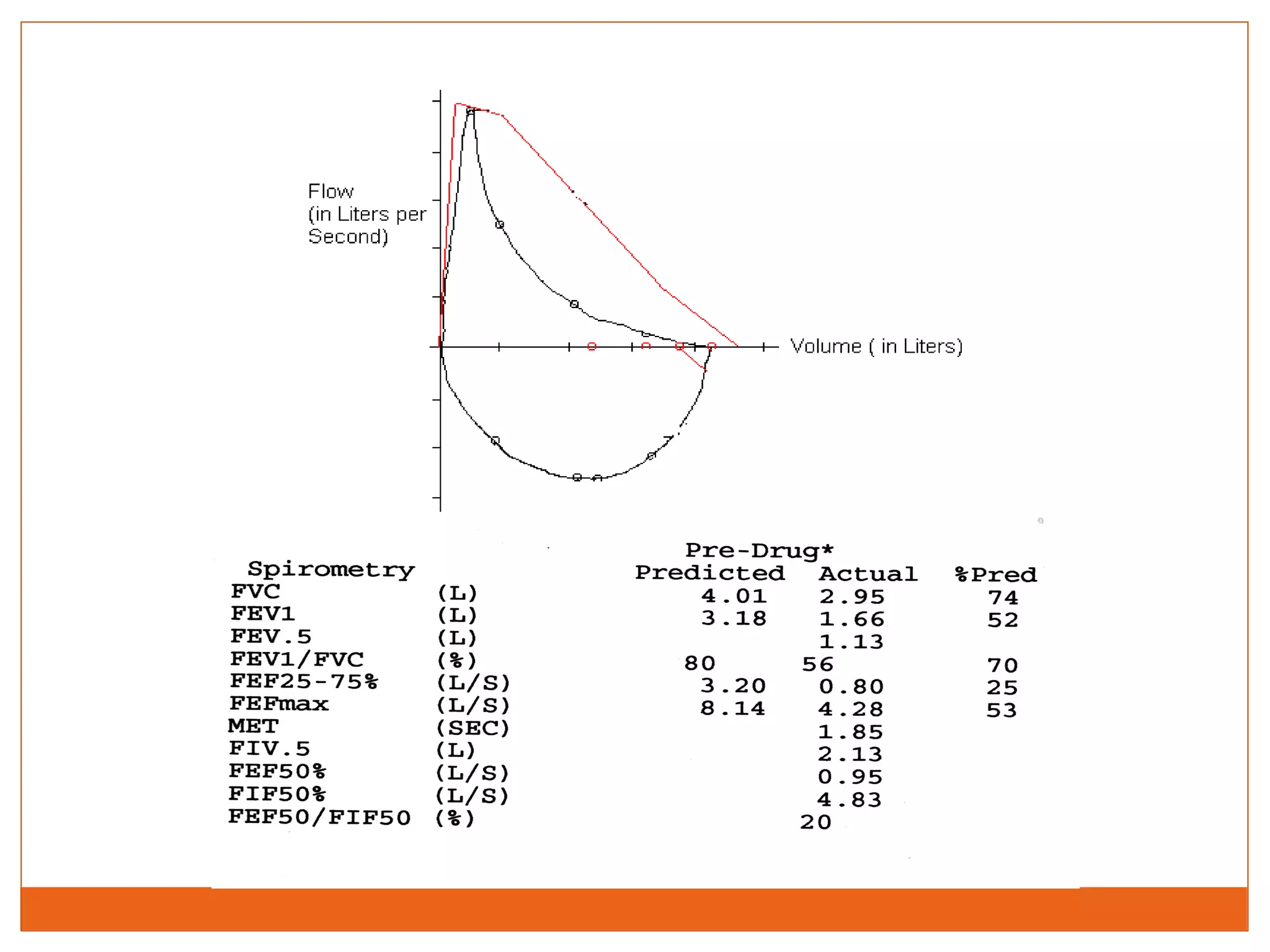
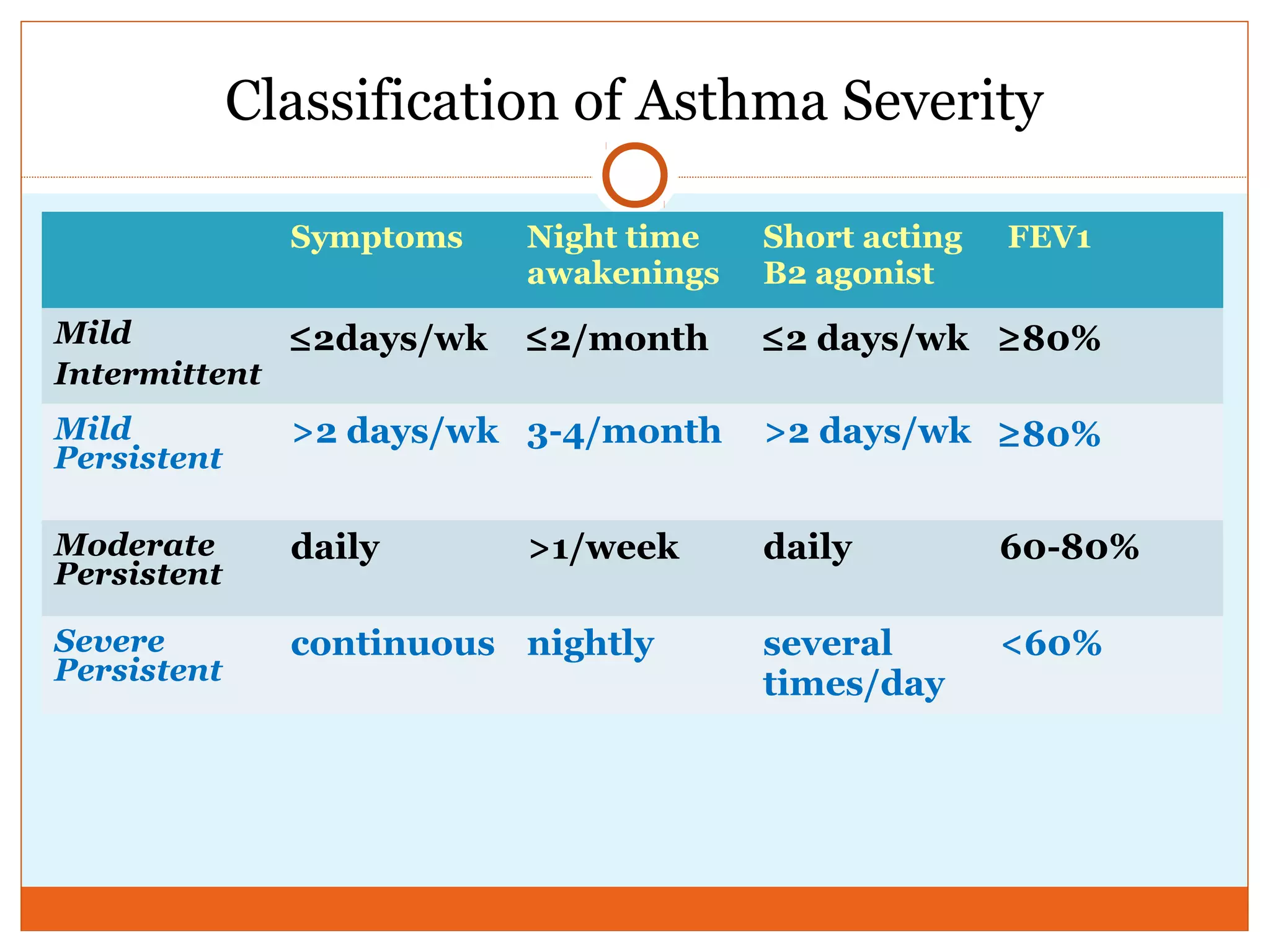
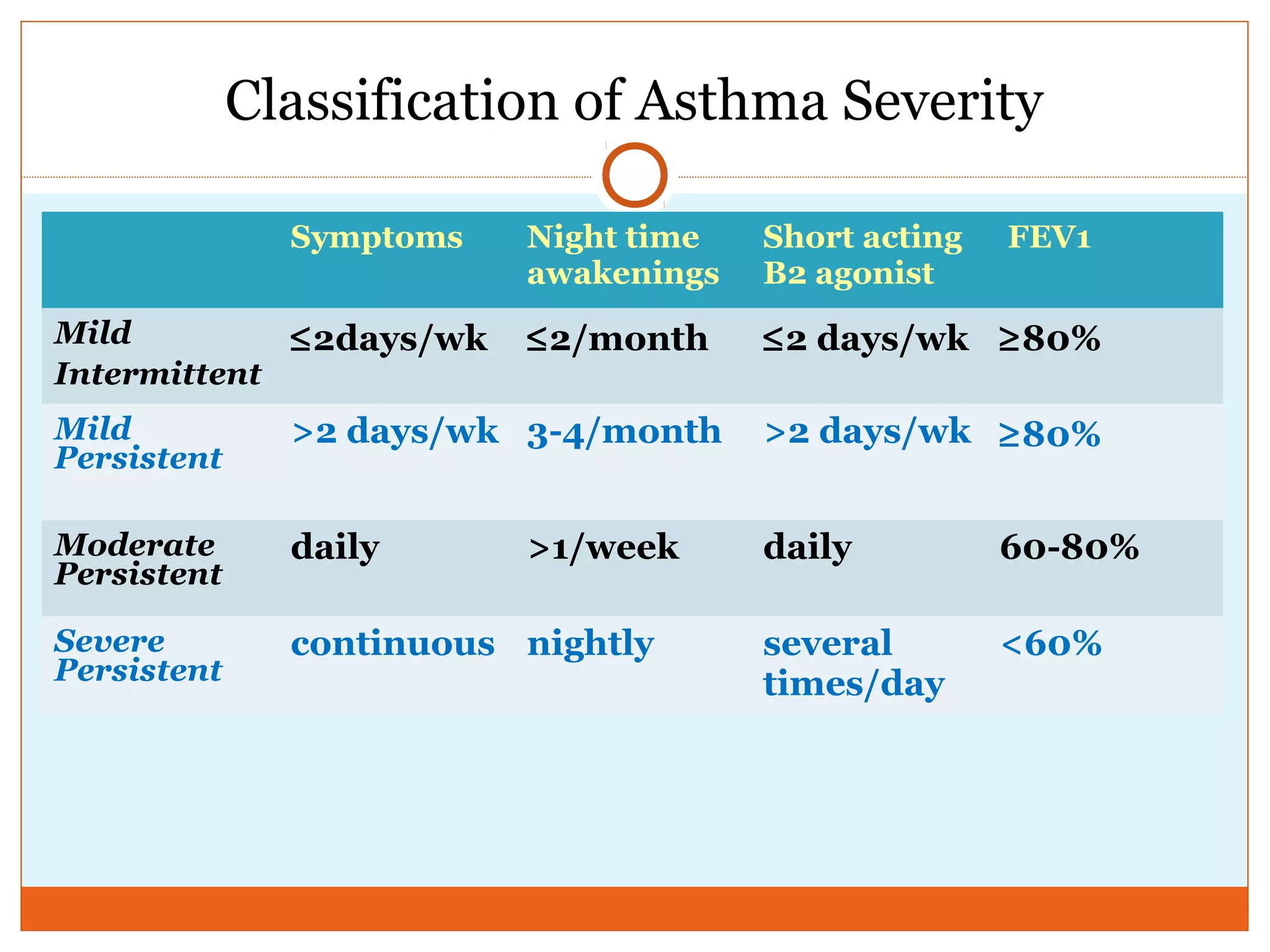
- Diagnosis involves assessing symptoms, lung function testing to detect reversible airflow obstruction, and ruling out other conditions.
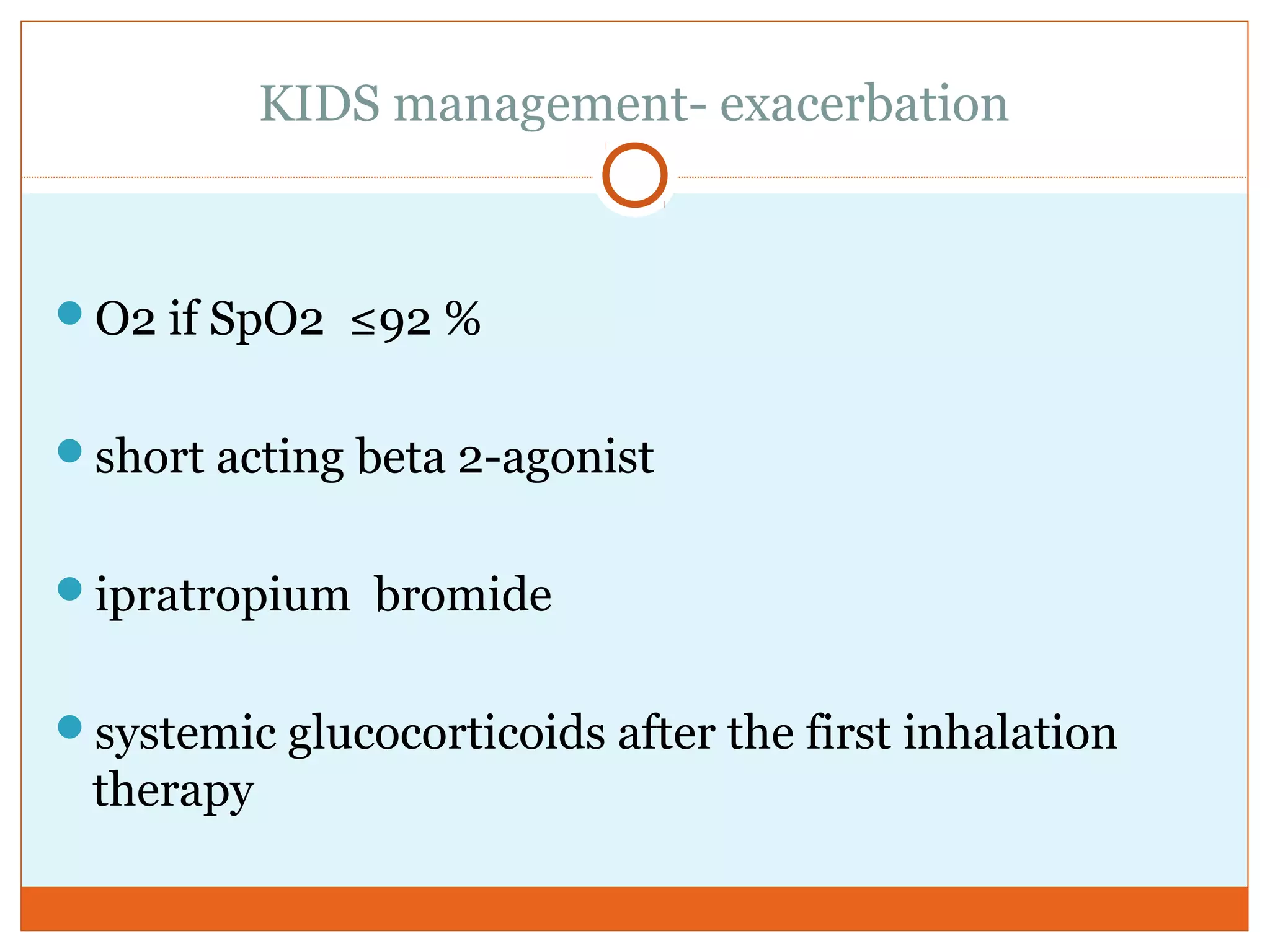
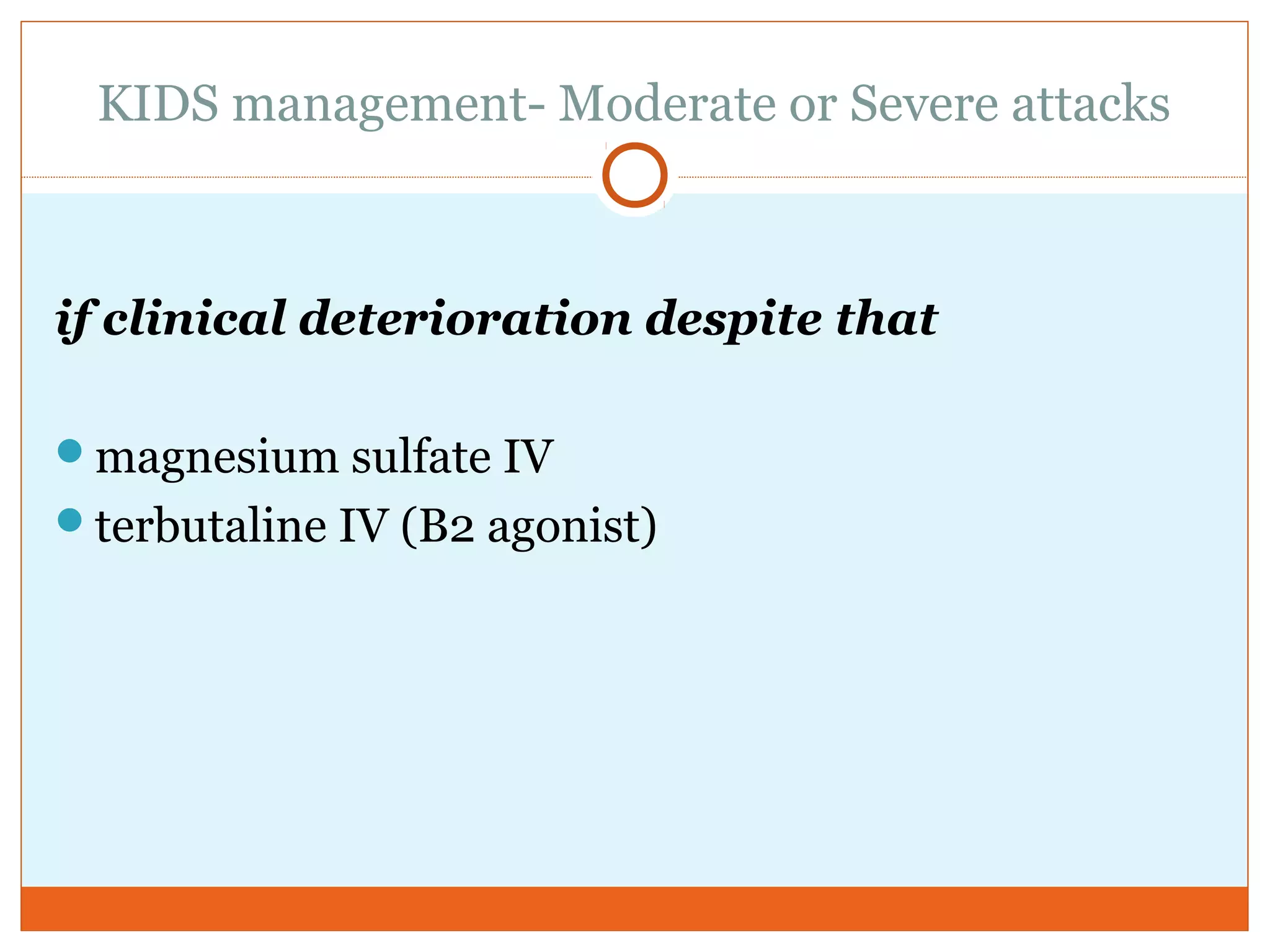
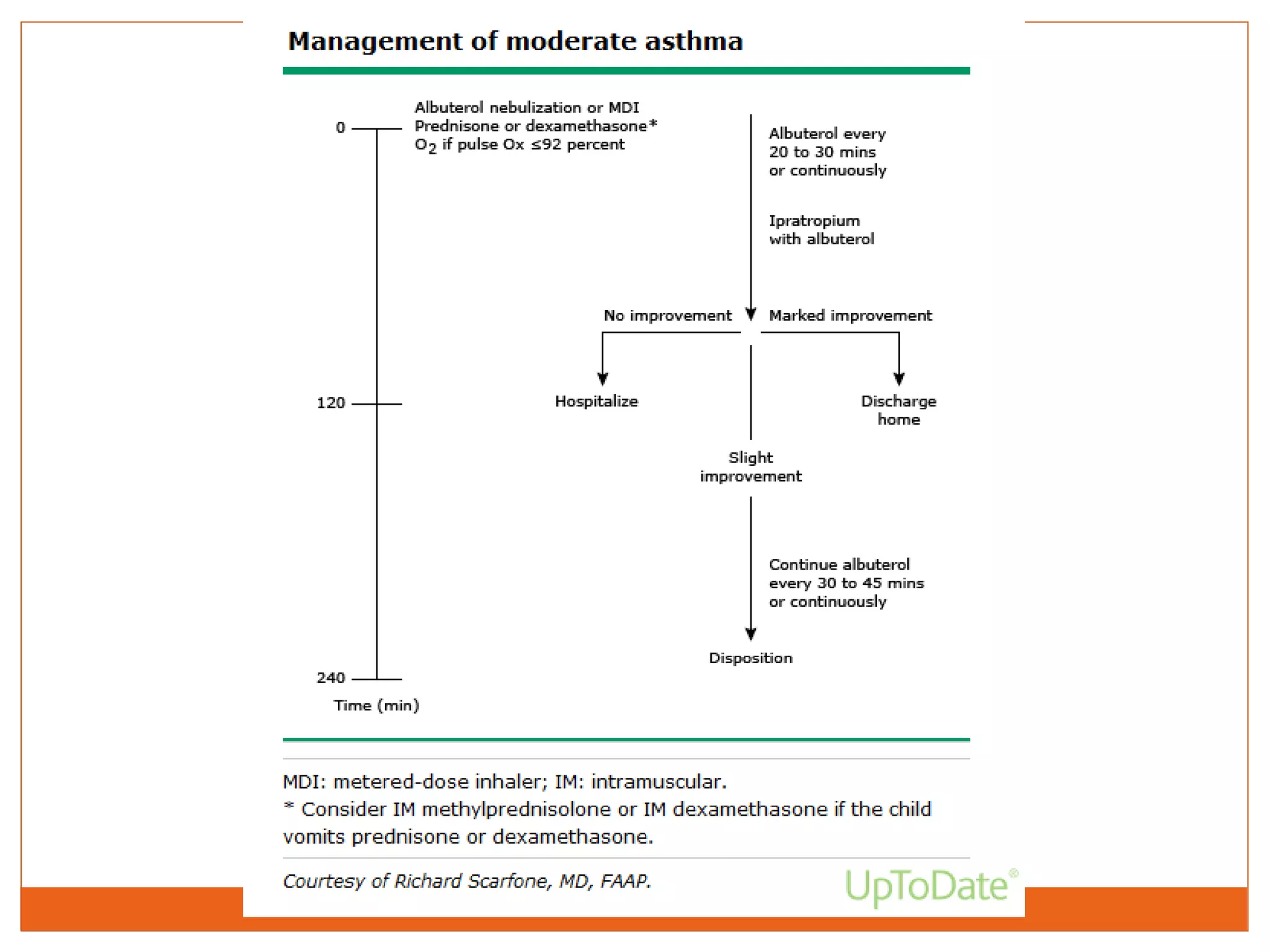
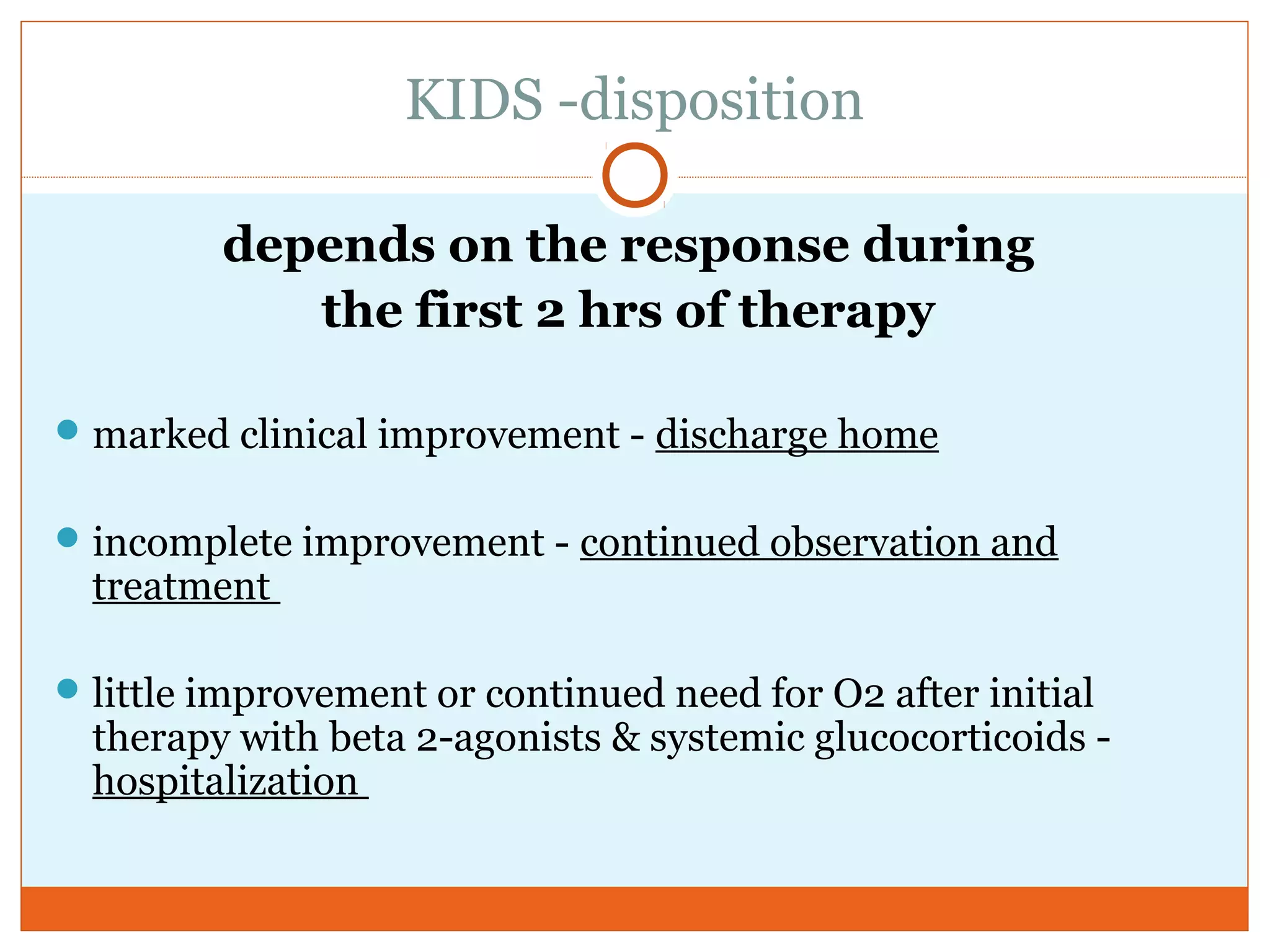
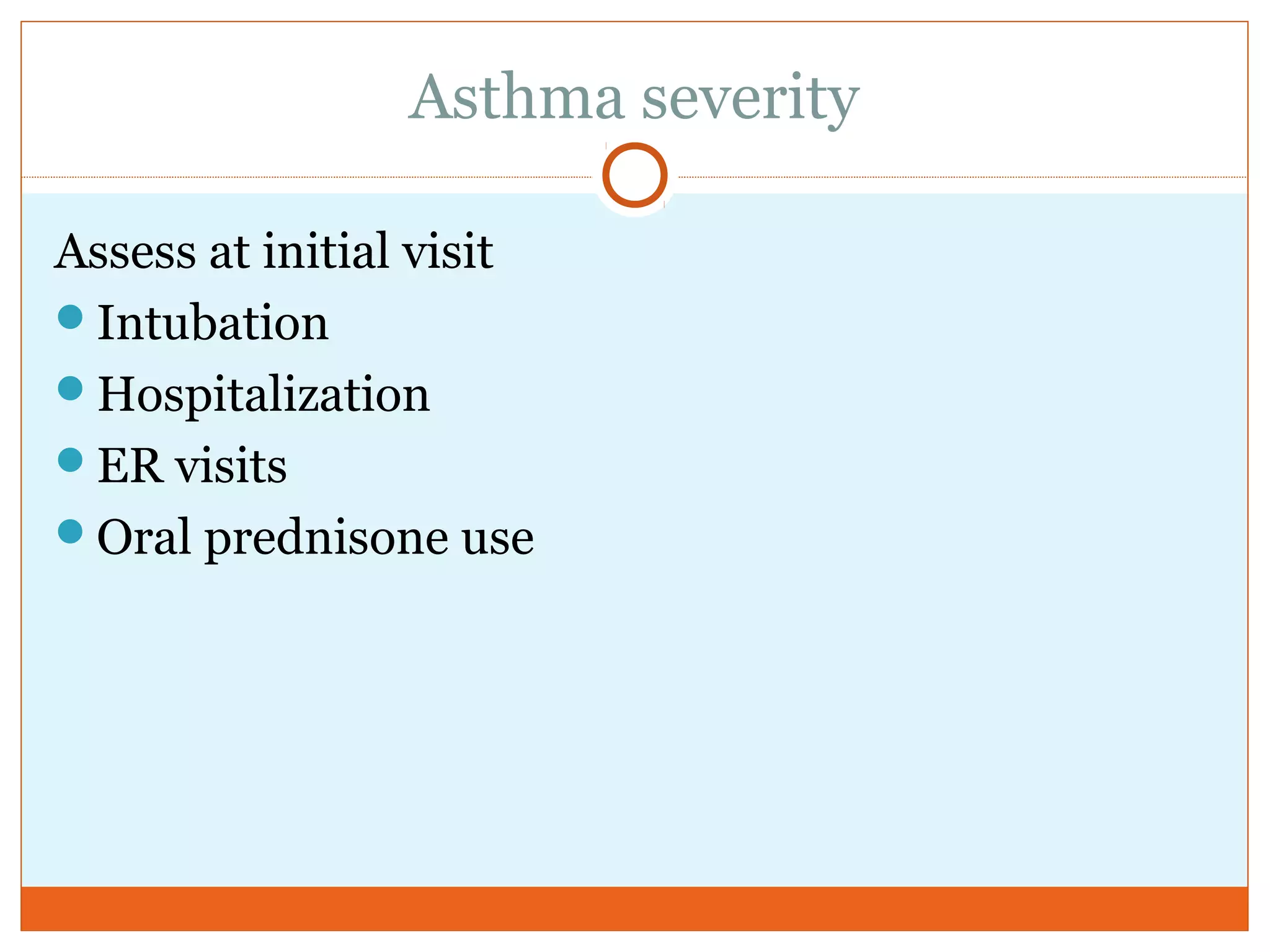
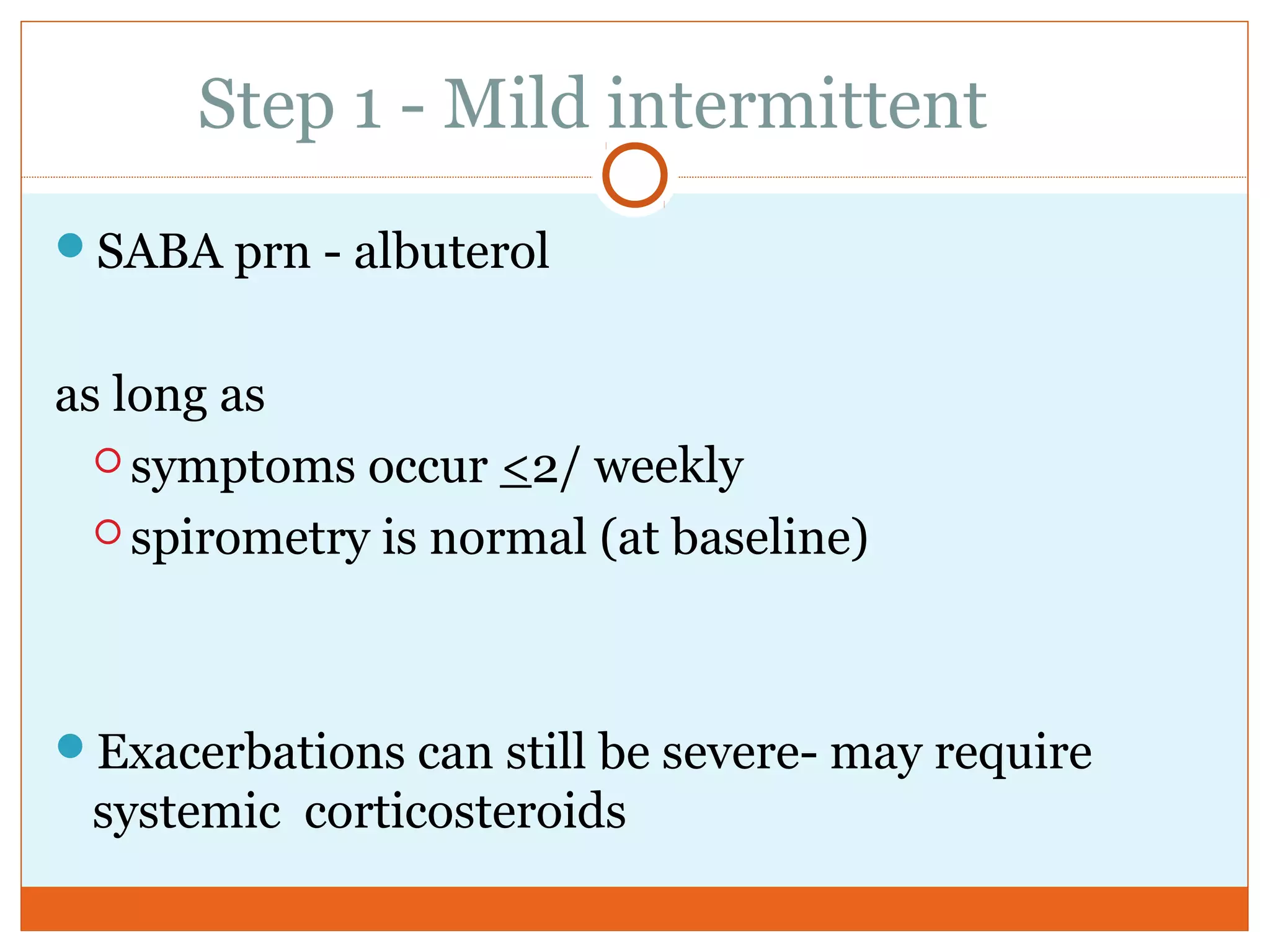
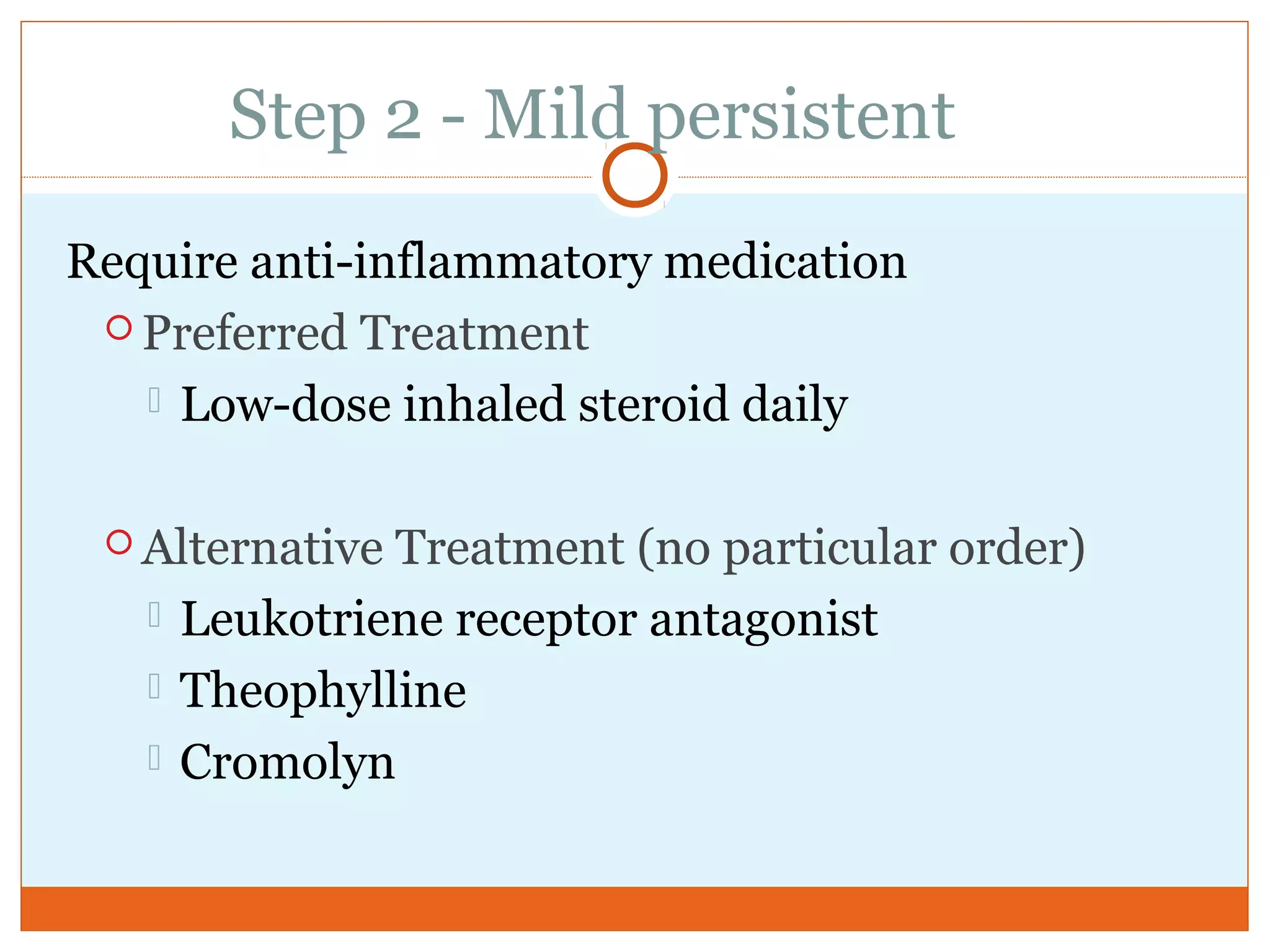
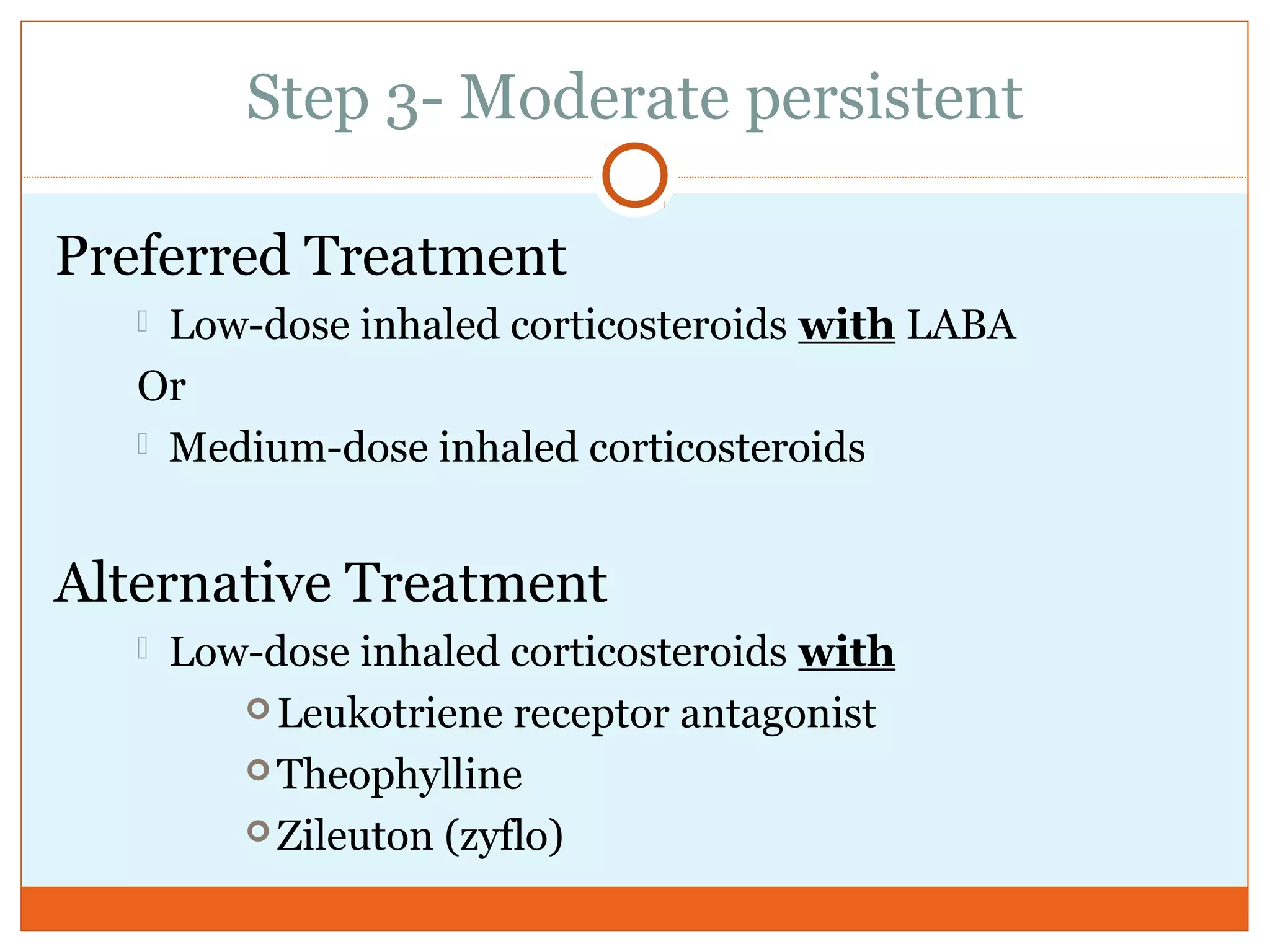
- Proper treatment and care can help control asthma and prevent its potentially serious consequences like hospitalizations and death.






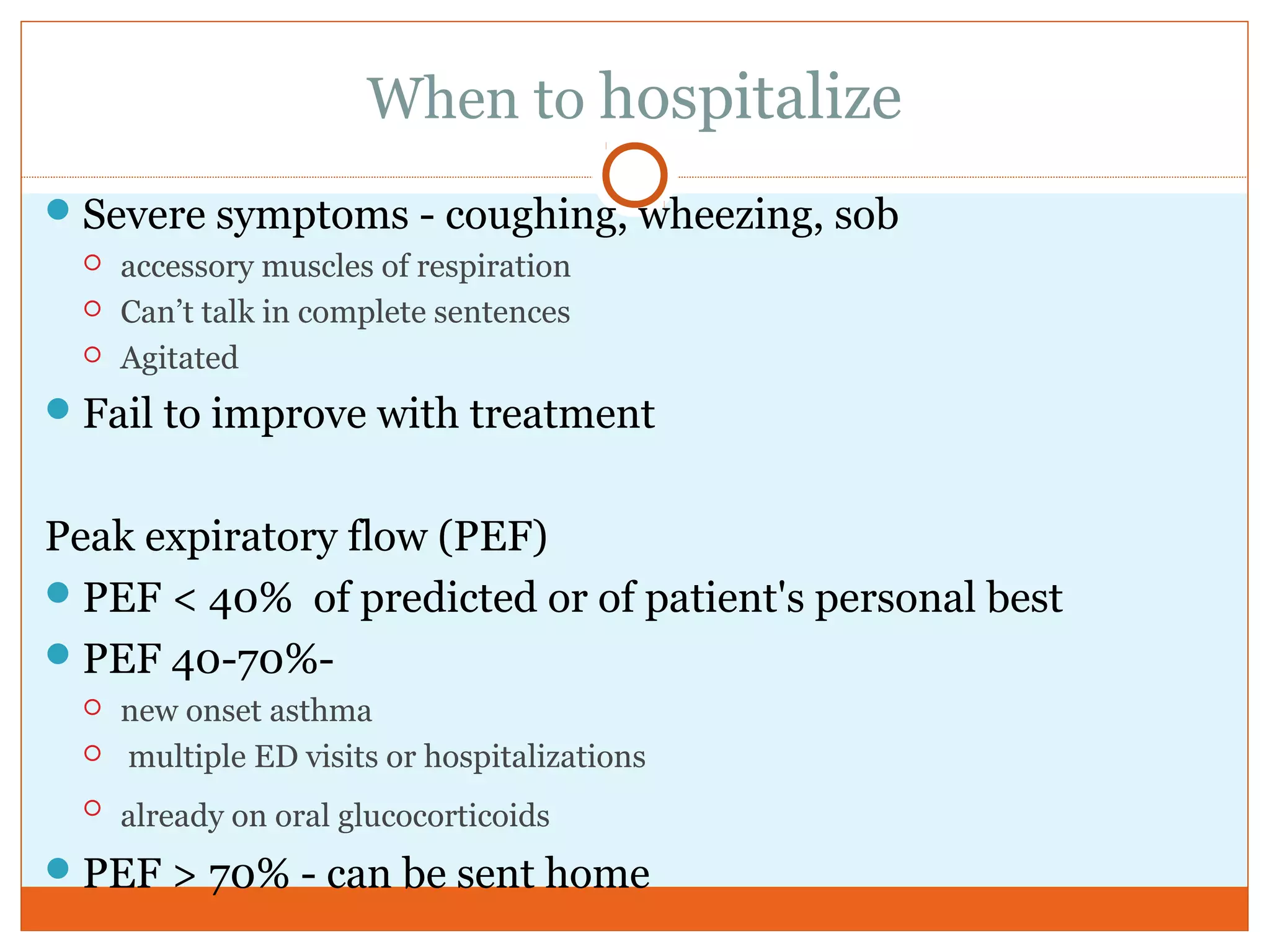
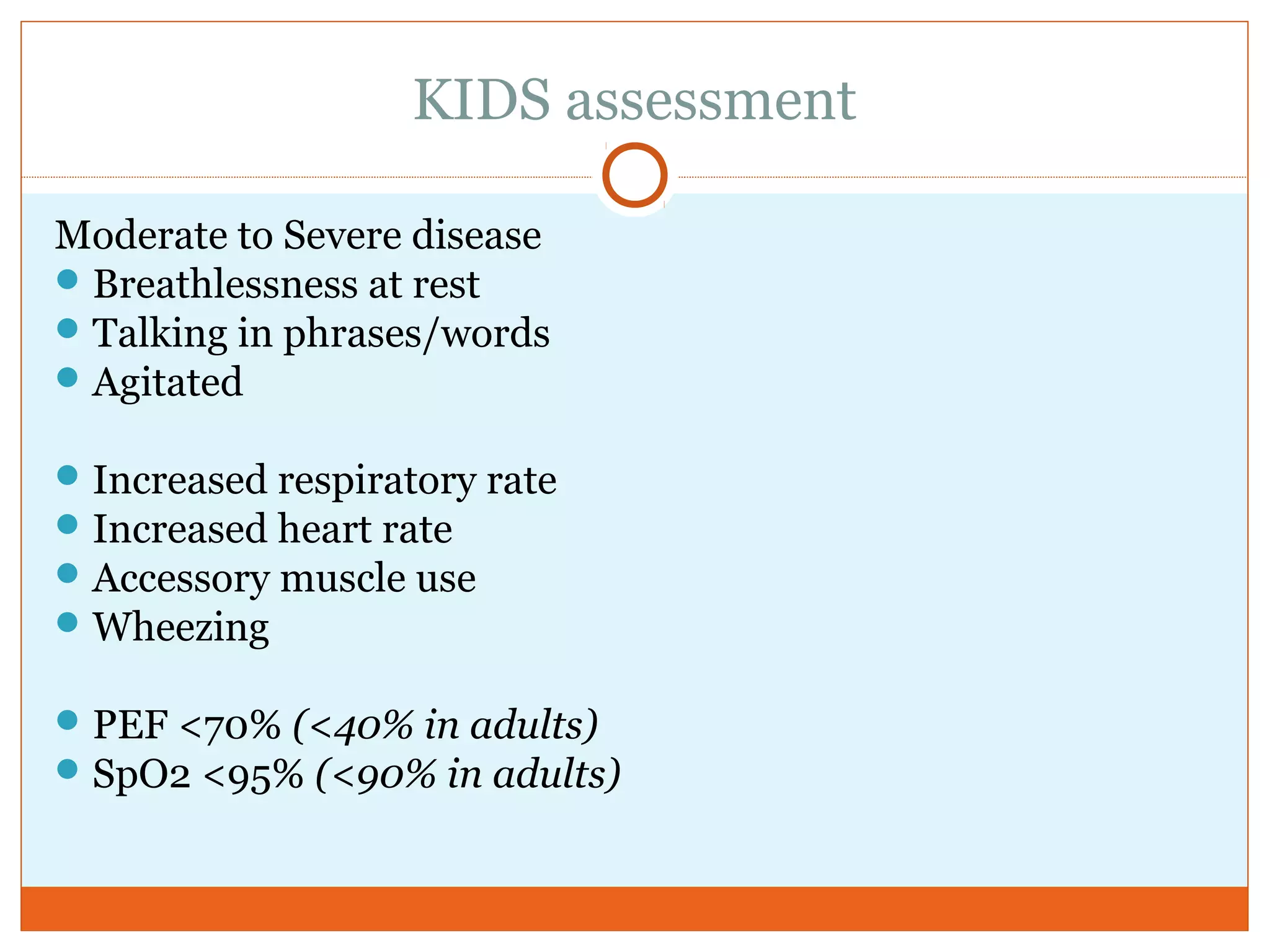
![ER Assessment
indicators of severe obstruction
Peak expiratory flow (PEF)
<40% predicted or <200 L/minute
pulse oximetry - oxygen saturation [SaO2]
SaO2 <90%
impending respiratory failure
Arterial blood gas (ABG) –hypercapnia
PEF <25% of normal (<100 to 150 L/min)](https://image.slidesharecdn.com/bpasthmacanvas2015-151003192018-lva1-app6892/75/Bp-asthma-canvas-2015-98-2048.jpg)