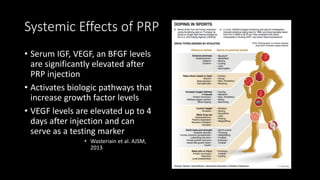
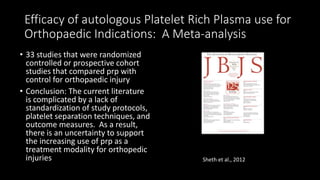
This document discusses platelet rich plasma (PRP), its history and uses, mechanisms of action, and clinical evidence. Some key points:
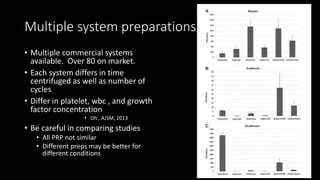
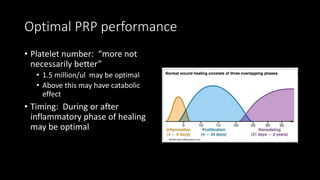
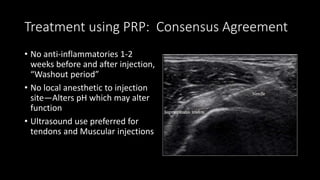
- PRP is concentrated platelets derived from centrifuging blood that delivers increased growth factors to enhance healing.
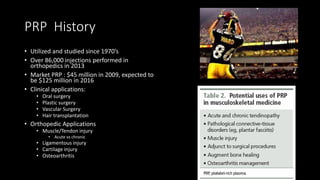
- It has been used since the 1970s and over 86,000 injections in 2013, though regulation and insurance coverage varies.
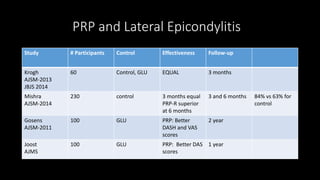
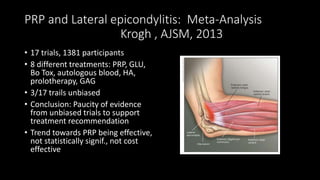
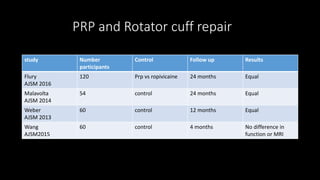
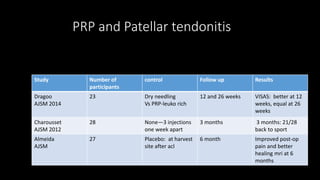
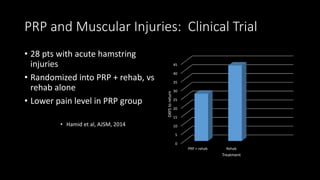
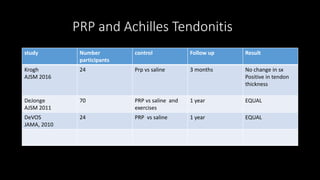
- Clinical applications include orthopedic injuries like tendinopathy and arthritis, as well as plastic surgery and hair restoration.
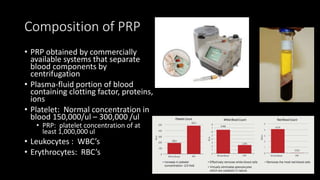
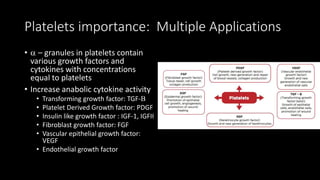
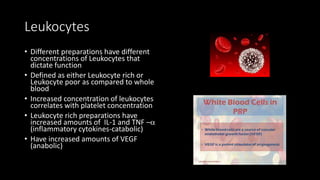
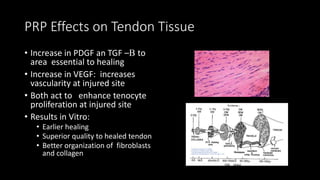
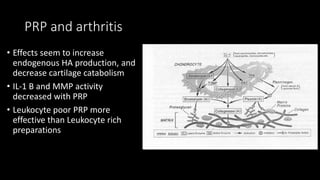
- Platelets contain growth factors that increase tissue healing through proliferation and vascularization. Composition and leukocyte concentration impact effects.
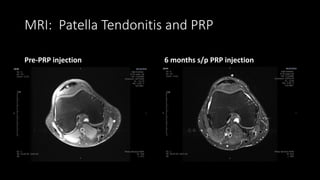
- Evidence for PRP in lateral epicondylitis and patellar tendin