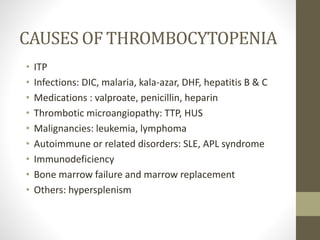
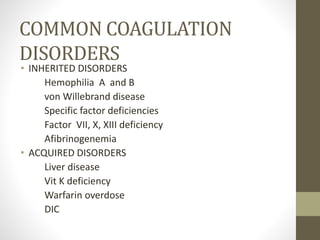
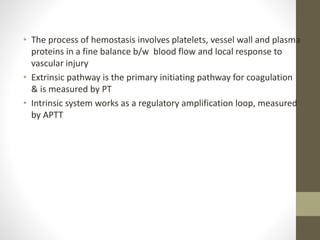
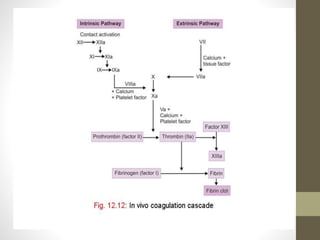
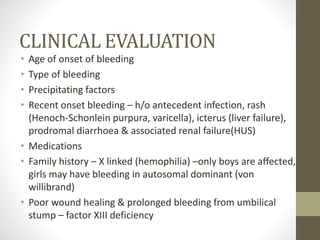
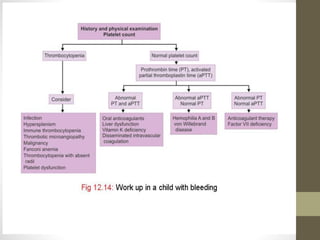
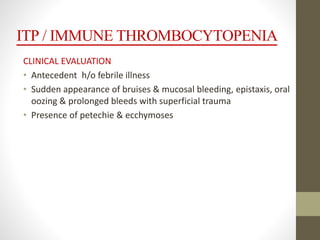
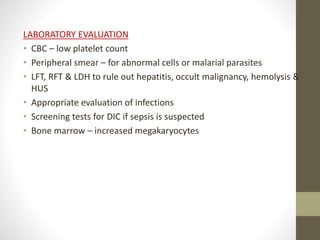
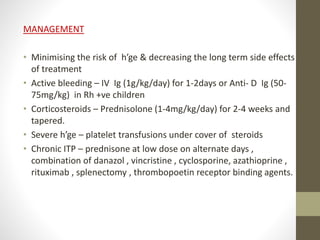
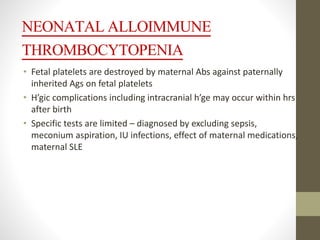
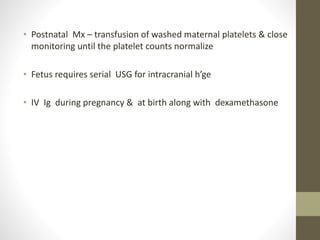
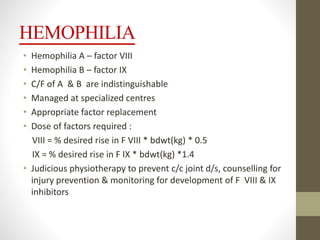
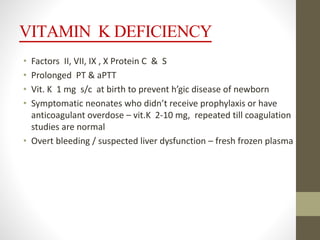
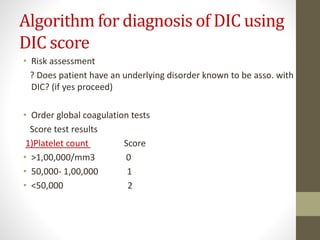
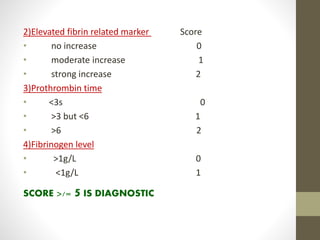
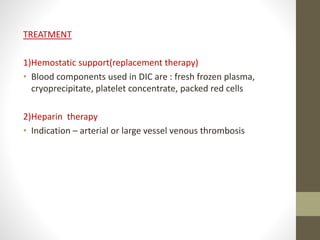
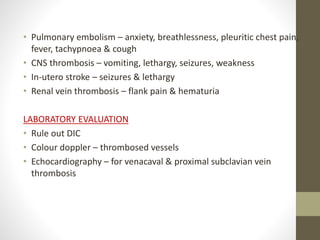
This document discusses the approach to managing bleeding in children. It covers various causes of bleeding including platelet disorders like thrombocytopenia from conditions like ITP, coagulation disorders, and dysfunctional fibrinolysis. It provides details on evaluating the clinical history and performing examinations and lab tests to identify the underlying cause. Specific conditions discussed in more depth include ITP, hemophilia, vitamin K deficiency, and DIC. Treatment approaches are described for replacing coagulation factors, corticosteroids, IVIG, platelet transfusions, and managing thrombotic disorders.