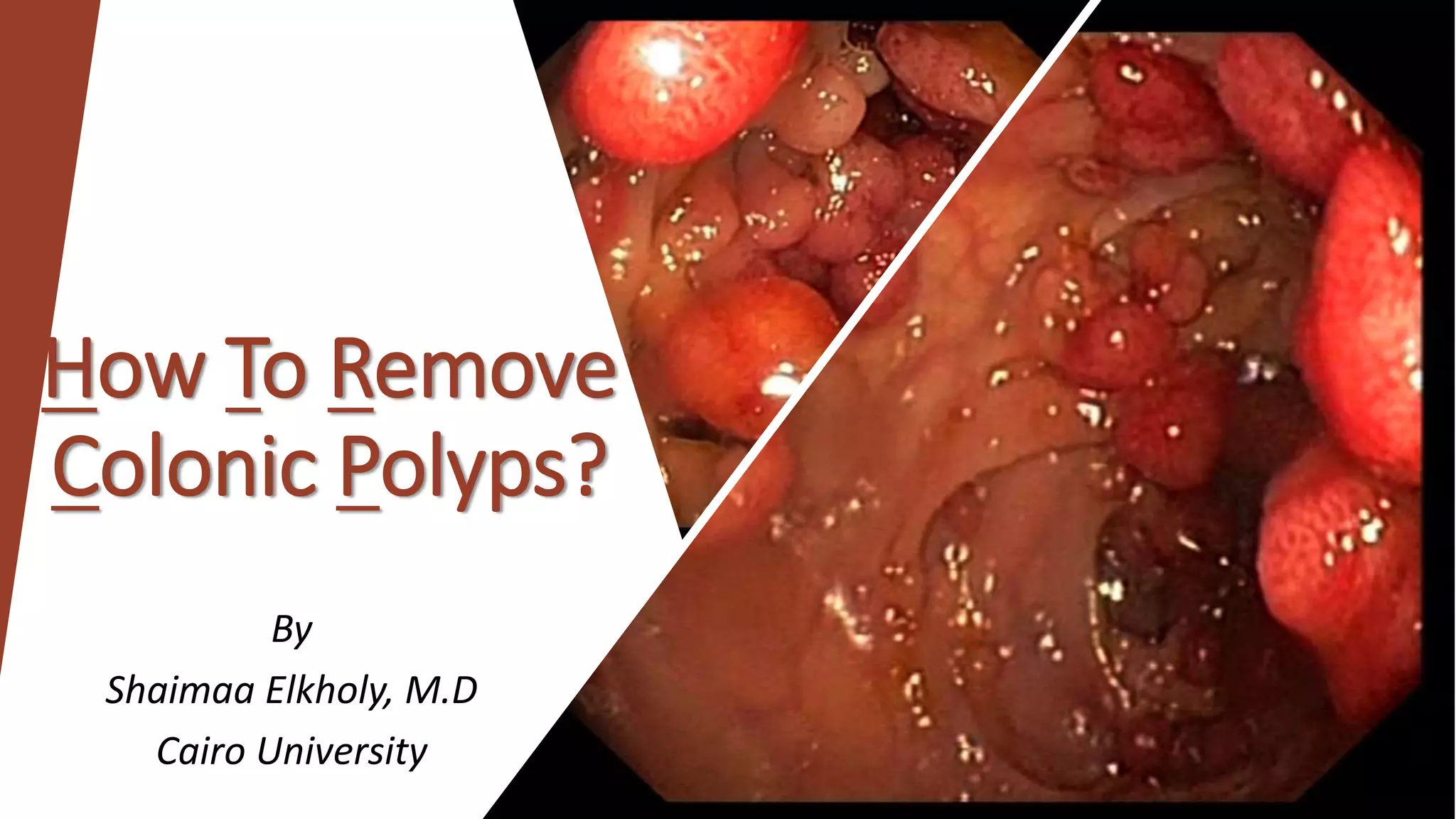
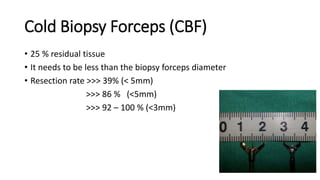
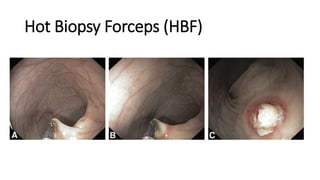
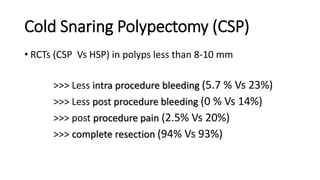
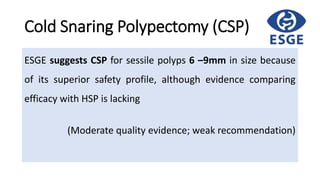
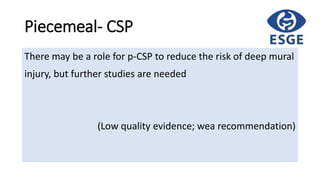
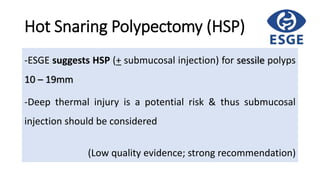
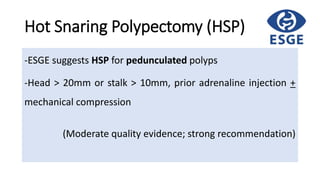
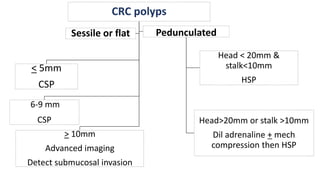
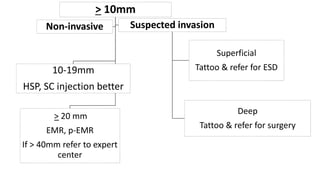
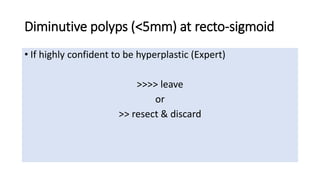
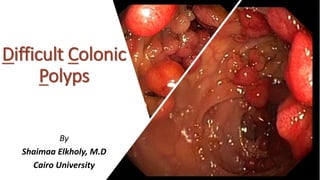
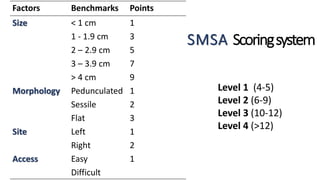
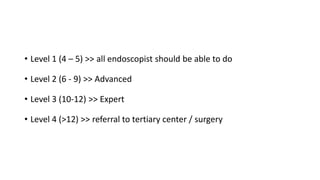
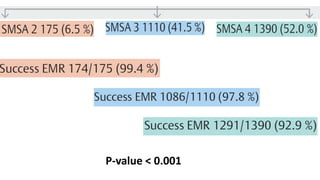
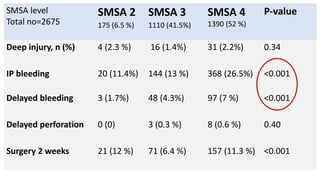
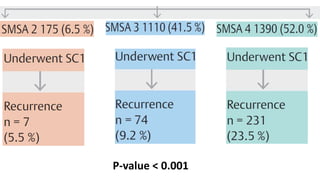
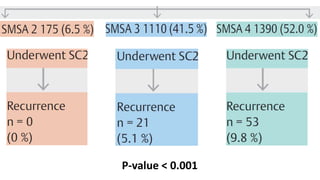
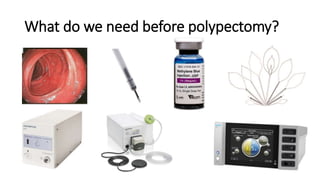
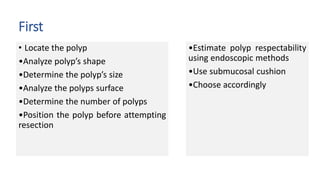
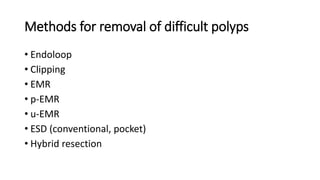
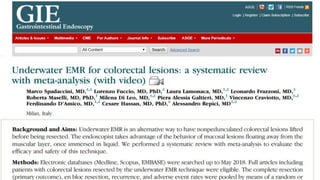
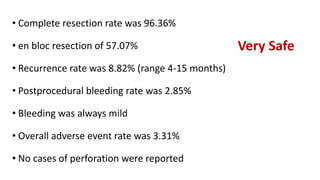
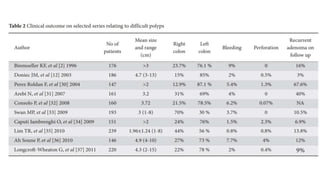
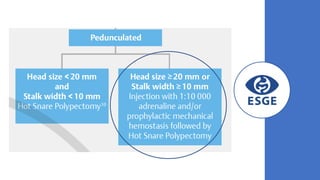
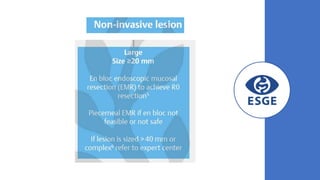
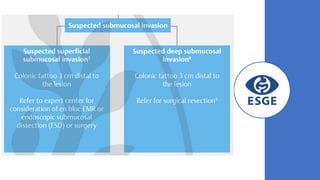
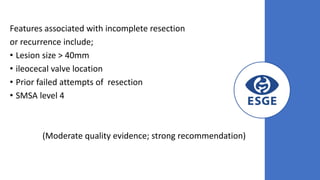
This document discusses methods for removing difficult colonic polyps. It describes various techniques including cold biopsy forceps, hot biopsy forceps, cold snare polypectomy, hot snare polypectomy, endoscopic mucosal resection (EMR), and endoscopic submucosal dissection (ESD). It provides details on these techniques and recommends methods based on polyp size, location, and complexity. For example, it recommends cold snare polypectomy for sessile polyps 6-9mm and hot snare polypectomy for sessile polyps 10-19mm. The document also describes a SMSA scoring system for classifying polyp difficulty and outlines factors associated with incomplete resection or recurrence.